Unemployment, Job Retention, and Productivity Loss Among Employees With Depression
Abstract
OBJECTIVE:This study comprehensively assessed the work outcomes of employees with depression. METHODS: We collected baseline and six-month follow-up survey data from 229 employees with depression and two employee comparison groups: a group of healthy patients for the control group (N=173) and a group with rheumatoid arthritis (N=87), a frequent source of work disability. Outcomes included new unemployment and, within the employed subgroup, job retention (versus job turnover), presenteeism (that is, diminished on-the-job performance and productivity), and absenteeism. RESULTS: At the six-month follow-up, persons with depression had more new unemployment—14 percent for persons in the dysthymia group, 12 percent for persons in the major depression group, and 15 percent for persons in the group with both dysthymia and major depression, compared with 2 percent for persons in the control group and 3 percent for persons in the rheumatoid arthritis group. Among participants who were still employed, those with depression had significantly more job turnover, presenteeism, and absenteeism. CONCLUSIONS: In addition to helping employees with depression obtain high-quality depression treatment, new interventions may be needed to help them to overcome the substantial job upheaval that this population experiences.
Studies have alerted us to the rising tide of chronic health problems worldwide and the social and economic burdens that they entail (1,2). Depression is a leading cause of this burden (1), costing the United States an estimated $26.1 billion annually in medical care and $44 to $51.5 billion annually in terms of lost productivity (3,4).
This study builds on research about the impact of depression on employment by focusing on employed individuals with depression and assessing multiple outcomes that are relevant to employees and employers. We report on unemployment rates among participants at the six-month follow-up and, among those employed, rates of job retention (sustained employment in the same job) versus job turnover (exiting a job), health-related presenteeism (diminished on-the-job performance and productivity), and absenteeism (missed work time and productivity loss caused by missed work time). We hypothesized that employees with depression would be at an employment disadvantage compared with other employees.
Although previous research has linked depression to adverse outcomes, such as joblessness and productivity loss, most studies have had weak external validity. Information about the impact of depression on employment has been generated from cross-sectional observational studies or from randomized controlled trials of depression treatment, many of which included employment outcomes as a secondary endpoint (5,6,7,8). Studies have included participants who were not working at baseline or were working very few hours, omitted employee comparison groups of persons who were not depressed, and assessed only one main outcome indicator, such as the employment rate. Finally, many studies were conducted during a period of great economic growth (early 1990s to 2001) and nearly full employment, which may have influenced the results (9). The purpose of our longitudinal study was to comprehensively assess work outcomes among employees with depression.
Methods
We used baseline and six-month follow-up data from the Health and Work Study sample, including 229 employees with depression in three subgroups: those with dysthymia (N=59), major depressive disorder (N=85), and both dysthymia and major depressive disorder (N=85) (10). To help us calibrate and interpret results, the Health and Work Study included two comparison groups: 173 healthy employees in the control group, whom we expected to have minimal job difficulties, and 87 employees with rheumatoid arthritis, whom we expected to experience employment problems (11). The healthy control group did not have any major chronic, potentially disabling health problems.
Participants were recruited from physicians' offices in Massachusetts between February 2001 and May 2003. Physicians were affiliated with the Tufts Health Plan, the Fallon Clinic, or Harvard Pilgrim Health Care. At baseline, all the participants were insured, but insurance was not an entry criterion. Study protocols were reviewed and approved by the human investigations review board of the Tufts-New England Medical Center and by the institutional review boards of each participating site.
Individuals were eligible if they were aged 18 to 62 years and worked at least 15 hours per week. Individuals were excluded from the study if they were planning to retire within two years, received disability benefits, had an active disability claim, abused alcohol or drugs, had a pregnancy or delivery within the past six months, had bipolar disorder, were unable to speak or read English, or were given a diagnosis of at least one of 11 potentially disabling medical conditions (heart attack in the past 12 months, chronic chest pain [angina], congestive heart failure, stroke, diabetes, cancer [other than skin cancer] that is currently being treated, chronic low back pain involving pain radiating down one's leg, back pain without radiating leg pain, degenerative neuromuscular conditions [for example, multiple sclerosis and amyolateral sclerosis], severe headache pain occurring more than two times a week, and severe joint pain due to osteoarthritis occurring more than two times per week).
Eligibility was assessed by using data from a self-administered brief screener, a longer screening interview, and a physician-reported checklist. This process was used to accurately identify patients with depression as well as to minimize response burden.
During routine office visits, patients were offered the brief screener. Items on the screener addressed employment status, retirement plans within two years, pending disability or worker's compensation claims, alcoholism, and depression. The screener used the CAGE questionnaire to measure alcoholism (12). To measure mental health, the screener used the three-item depression prescreener from the World Health Organization (13), two items that assessed history of bipolar disorder, and a sensitive and specific patient-administered depression screening instrument (PC-SAD) for assessing dysthymia and major depressive disorder (14).
Completed screeners were scanned on site, and potentially eligible patients with depression or rheumatoid arthritis were selected for further assessment. Because we anticipated identifying more healthy patients from the control group than we needed to achieve statistical power, a control group selection algorithm was programmed into the scanner, selecting only one out of every ten healthy patients screened for the control group.
After this brief screener step, the physician of each potentially eligible patient was asked whether any exclusionary diagnoses were present and, if applicable, to document rheumatoid arthritis. Physicians were asked to rule out depression secondary to an underlying medical condition (for example, hyperthyroidism) or medical treatment (for example, medication regimens affecting mood). We informed physicians if their patients screened positive for depression.
Next, eligible patients were sent a package to obtain baseline measurements. An interviewer followed up with a phone call to explain the study further, answer questions, ask additional eligibility questions—such as whether the patient had a history of bipolar disorder or had a recent bereavement—and administered the Patient Health Questionnaire Depression Scale (PHQ-9), a self-administered instrument for assessing major depression (15). Because some individuals were difficult to reach or interview by phone, we allowed them to complete these questions by mail as part of the self-administered baseline questionnaire. A study investigator reviewed the mail responses and determined whether the eligibility criteria were met.
Eligible individuals were enrolled after a signed consent form was returned. Each enrollee was asked to complete mail surveys at baseline and every six months for 18 months. The follow-up surveys each repeated a set of core questions. This article reports data for the six-month follow-up questions, which have been completed. Cash incentives were provided ($20 for the baseline survey and $10 for each follow-up survey).
Measures
We included four outcome measures. Follow-up employment status was determined by asking the respondents whether, at any time in the past two weeks, they worked for pay. Job retention versus job turnover was determined by asking participants in the employed subgroup whether during the past six months they were fired, were laid off, quit a job, changed occupations, changed employers, or became self-employed. To validate reported job turnover, we also compared baseline and six-month follow-up occupational data.
Presenteeism was assessed with the Work Limitations Questionnaire (WLQ) (16). The WLQ has been validated in a range of patient and employee groups, including employees with symptoms of depression (17,18). Scale scores reflect the percentage of time in the previous two weeks an employee was limited on the job in performing four types of job tasks: physical demands (for example, lifting), time management (for example, working the required hours), mental and interpersonal demands (for example, concentrating on work), and output demands (for example, handling the workload). Scales are scored from 0, limited none of the time, to 100, limited 100 percent of the time. Scores are weighted and aggregated to generate a productivity loss index score. The index is a weighted sum of scale scores that indicates reduction in output per hour compared with the output of a healthy (not limited) employee. A technical report about the WLQ scoring is available from the authors.
Absenteeism, or the total number of days missed, was measured by the sum of responses to two items from the WLQ work absence module: "In the past two weeks, how many full workdays did you miss because of your health or medical care?" and "In the past two weeks, what was the total number of days you missed part of a workday because of your health or medical care?" A full day of work missed was given a value of 1, and a partial day of work missed was assigned a value of .5. Additionally, to indicate lost productivity related to work absences, we computed the ratio of the number of hours missed from work to the number of usual work hours. We converted days missed to hours missed by assuming that a full-time employee worked eight hours per day and a part-time employee worked six hours per day. We classified 6.2 percent of the sample as part-time employees because they worked 30 hours per week or less.
Besides the outcome variables, we reported two additional outcomes for the subgroup of participants who were employed at follow-up: change in the number of hours worked per week and change in income.
We compared outcomes across the five groups: dysthymia, major depression, both dysthymia and major depression, rheumatoid arthritis, or control. Participants were assigned to groups on the basis of the results of the multi-step screening process. Patients with rheumatoid arthritis and depression (N=8) were classified as having rheumatoid arthritis.
We also compared the groups for other variables. Depressive symptom severity was assessed by self-report at baseline and follow-up with the PHQ-9 scale (19). The number of comorbid medical conditions was ascertained with a checklist (based on the Medical Outcomes Study version) that determined whether a physician had diagnosed any of 11 conditions that would exclude individuals from the study (20). Health status was measured by using the physical health component score and the mental health component score of the Medical Outcomes Study 12-Item Short-Form Health Survey (SF-12) (21). Demographic characteristics included age, gender, and race or ethnicity as well as baseline measurements of education level, marital status, median annual income adjusted for age and gender, years at the present job, number of jobs held since the age of 18 years, whether the participant is self-employed, whether the participant is employed at more than one job at once, and the imputed company size (number of employees).
Baseline occupation reflects the six-digit 1990 standard occupational classification (SOC) coding procedure (22). To obtain the SOC code, participants' responses to standard open-ended questions were coded and assigned to one of 23 major occupational groups. These groups were then combined into three broad categories: professionals, managers, and technicians; sales, service, and support; and production, construction, repairs, and transportation.
Participants were considered to have obtained some type of treatment for depression if they reported current use of an antidepressant medication or a visit to a health care provider for an emotional problem during the past three months. This study was not designed to assess treatment outcomes; thus the data are mainly descriptive.
Analysis
Descriptive statistics are presented for all the variables. Differences between the groups were tested with analysis of variance. Follow-up data are presented. Outcomes for the groups were adjusted for baseline age, gender, and number of physician-diagnosed medical comorbidities. Longitudinal comparisons of WLQ scores and absences included participants employed at baseline and the six-month follow-up who had the necessary data (N=451). All analyses used Stata 7.0 (23).
Response
Of 14,274 screeners completed in physician offices, 8,237 (58 percent) were for patients from the control group that were randomly excluded by the control group selection algorithm (90 percent of those eligible for the control group), and 4,124 (29 percent) did not meet the initial eligibility criteria. Of the remaining 1,913 individuals (13 percent of the total population screened), 642 (34 percent) were ineligible, 599 (31 percent) did not complete the screening process (leaving eligibility unknown), and 672 (35 percent) were confirmed to be fully eligible. Among the 672 eligible patients, 572 (85 percent) enrolled in our study and 100 (15 percent) declined. No statistically significant differences were found between these two groups in employment, the physical health component score, the mental health component score, and the percentage who screened positive for depression (p<.05). Persons who declined to participate in our study tended to be younger and male (p<.05).
Results
Of the 572 participants enrolled in our study, most were female (461 participants, or 81 percent) and white (521 participants, or 92 percent). Approximately half the participants (292 participants, or 51 percent) had professional, technical, and managerial occupations; 237 participants (42 percent) were in sales, support, and service positions; and 40 participants (7 percent) were in production, construction, repairs, and transportation positions (data were missing for three participants). The mean number of hours worked per week was 38.6±.5, and a small group of participants (40 participants, or 9 percent) was self-employed. As shown in Table 1, the groups were significantly different in age, gender, marital status, education, and the number of jobs held since the age of 18 years (p<.05).
Table 1 shows that compared with the rheumatoid arthritis and control groups, the depression groups reported significantly more comorbid medical conditions and poorer mental health status. Although the rheumatoid arthritis group reported more physical health problems than the depression groups, the depression groups reported significantly more physical health problems than the control group. The three depression groups also differed significantly from one another in mental health status and depression severity. A total of 96 participants with depression (42 percent) were taking antidepressants. More participants in the depression groups had sought help for an emotional problem in the past three months.
At the six-month follow-up, 7 percent of the sample that was initially employed (38 participants) was now unemployed. Compared with the rheumatoid arthritis and control groups, the depression groups had significantly more job loss. As shown in Table 2, at follow-up unemployment rates were 14 percent for the dysthymia group, 12 percent for the major depression group, and 15 percent for the group with both dysthymia and major depression. The unemployment rate at follow-up was 3 percent for the rheumatoid arthritis group and 2 percent for patients from the control group (p<.001).
Among participants who were employed at the six-month follow-up, fewer participants in the depression groups retained their baseline jobs. Thus reported job turnover was 13 percent for the dysthymia group, 20 percent for the major depression group, and 13 percent for the group with both dysthymia and major depression, compared with only 9 percent for the rheumatoid arthritis group and 5 percent for the control group (Table 2). Within this small subgroup of participants who experienced job turnover, 33 percent of participants (11 of 33 participants) with depression took a lower paying job for health reasons, compared with 20 percent of participants in the comparison groups (three of 15 participants).
Overall, in the subgroup employed at follow-up, no significant difference was found in the change in weekly work hours. However, the percentage of participants whose incomes increased was significantly greater in the rheumatoid arthritis and control groups than in the depression groups (Table 2).
As shown in Table 3, the depression groups also had more presenteeism. At baseline, the depression groups' average productivity loss was between 6 and 10 percent, compared with mean rates between 2 and 4 percent, respectively, for the rheumatoid arthritis and control groups. Even though the data showed a trend toward improved productivity, participants with depression still had significantly more at-work productivity loss at follow-up than did participants in the comparison groups.
As shown in Table 3, at follow-up, participants who were in the depression groups were limited in their ability to perform mental and interpersonal tasks at least twice as frequently as participants who were in the comparison group (p<.001). Time management was impaired a mean of 21±3.1 to 31.7±2.8 percent of the time in the depression groups, 9.6±2.1 percent of the time in the control group, and 19.4±2.7 percent of the time in the rheumatoid arthritis group (p<.001). A similar pattern was found for the WLQ output scale (p<.001). The participants who were in the rheumatoid arthritis group was the least able of the groups to perform physical job demands (limited a mean of 18.9±2.5 percent of the time) (p<.001).
In the total sample, the mean number of work absences over a two-week period declined over time from 1.1 days to approximately .9 days (Table 3). Productivity loss at follow-up was greatest in the depression groups. Mean productivity loss related to work absences was 11.5±4.3 percent for participants in the dysthymia group, 20.7±4 percent for participants in the major depression group, 13.7±4.1 percent for participants with both dysthymia and major depression, 8.3±3.7 percent for participants in the rheumatoid arthritis group, and 5.2±3 percent for participants in the control group (p<.003; data not shown).
Discussion
This is the first study to comprehensively assess work outcomes among employees with depression who had no immediate plans to stop working. By any measure, employees with depression did worse than those in the comparison groups. Compared with employment rates in either the rheumatoid arthritis group or the control group, more employees with depression became unemployed, began a different job, were limited in their ability to perform their jobs, and missed time at work. Employees with depression had an unemployment rate approximately five times the rate among employees in the rheumatoid arthritis group or the control group. And, although turnover can sometimes lead to a better job, our data suggest that it tended to result in lower hourly earnings for employees in the depression groups.
Several mechanisms may be responsible for adverse depression outcomes, such as new unemployment. These include poor job performance, discrimination, low seniority, a low-status position, difficulty coping with job pressures, job accommodation barriers, and treatment quality—although the treatment rate found in this study was similar to rates reported elsewhere (24,25,26).
Impaired job performance probably explains some of the unemployment. At baseline, presenteeism scores in the depression groups were worse than those in the comparison groups, and, despite improvement, the scores were also worse at follow-up. On average, at follow-up, employees in the depression groups were having difficulty managing their time, mental and interpersonal job demands, and output demands 20 percent of the time or more—an amount equivalent to two eight-hour workdays in two weeks.
Previous research suggests that employment outcomes improve after symptoms decrease (10). In at least three depression treatment trials that were conducted in primary care settings (which did not control for baseline employment status), patients whose symptoms improved had higher employment rates. Simon and colleagues (6) reported that as depression improved or remitted, patients' employment rates increased to more than 80 percent one year after treatment. Schoenbaum and colleagues (27) reported that patients who received appropriate depression treatment achieved a six-month employment rate of 72 percent. In a randomized trial, patients who received high-quality depression treatment had a higher employment rate one year after treatment than patients who received usual care (8).
In this study, the care received may have been similar to usual care in clinical trials. Nevertheless, we found that the employment rate at follow-up was significantly higher in the subgroup of participants with depression who were taking antidepressants at both baseline and follow-up (p=.031). In that group, 95 percent of the participants were employed, which is slightly lower than the rate found among participants in the control group. Among participants who were taking an antidepressant at either baseline or follow-up or who were not taking an antidepressant at both of these time points, only 84 percent were employed, which is considerably lower than that found among participants in the control group. Although this study was not designed to evaluate treatment, these data suggest that treatment may narrow the gap between depressed employees and healthy workers.
This study has several limitations. The results may not be generalizable. Our clinic-based sample of persons with depression had a higher mean severity level than a similarly assessed community-based sample of employees with depression, drawn from a national follow-on survey to the General Social Survey (28). The patients in the control group in our study also had fewer comorbid medical conditions than the national survey sample, because our study excluded persons with certain comorbid conditions. Also, although our results suggest that depression was the underlying reason for participants' work problems, we did not assess the impact of occupation and industry on an employee's work outcome or the impact of previous job training, education level, and work history. Finally, our data were almost entirely self-reported.
Conclusions
This study adds to the literature about depression and employment and points to gaps in services. Many individuals with depression do not receive adequate diagnosis and treatment. Moreover, the available interventions that might help employees to function better at work are not geared toward this population. Employment programs for adults with mental disorders provide job entry services mainly for persons with severe and chronic mental illness. Job accommodations are generally aimed at individuals who meet criteria for disability (29). Employee assistance programs, when available, usually intervene when the employee has a severe job performance problem. Our data suggest that there is a need for programs—in addition to quality medical care—to help employees with depression cope with the substantial job upheaval that many in this population will experience.
Acknowledgments
This study was sponsored by grant R01-MH-58243-01A2 from the National Institute of Mental Health and received research support from the Tufts-New England Medical Center General Clinical Research Center, which is funded by grant M01-RR-00054 from the National Center for Research Resources.
Dr. Lerner, Dr. Adler, Dr. Chang, Ms. Lapitsky, Ms. Hood, Ms. Perissinotto, and Dr. Rogers are affiliated with the Health Institute, Institute for Clinical Research and Health Policy Studies, Tufts-New England Medical Center, 750 Washington Street, T-NEMC #345, Boston, Massachusetts 02111 (e-mail, [email protected]). Dr. Lerner and Dr. Adler are also with the department of medicine at Tufts University School of Medicine in Boston. Dr. Reed is with the department of rheumatology at the Fallon Clinic in Worcester, Massachusetts. Dr. McLaughlin is with the department of medicine, division of clinical research, at the University of Massachusetts in Worcester. Dr. Berndt is with the Sloan School of Management at the Massachusetts Institute of Technology in Cambridge and with the National Bureau of Economic Research in Cambridge.
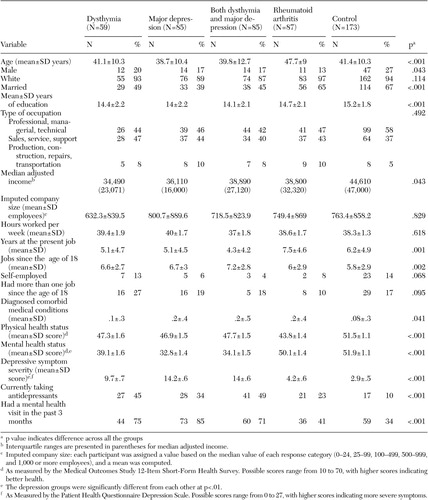 |
Table 1. Baseline characteristics of 489 participants in a study of work outcomes of employees with depression, by condition
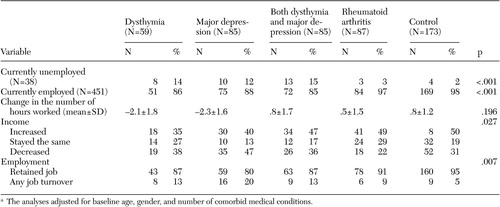 |
Table 2. Employment at the six-month follow-up among 489 participants in a study of work outcomes of employees with depression,by conditiona
a The analyses adjusted for baseline age, gender, and number of comorbid medical conditions.
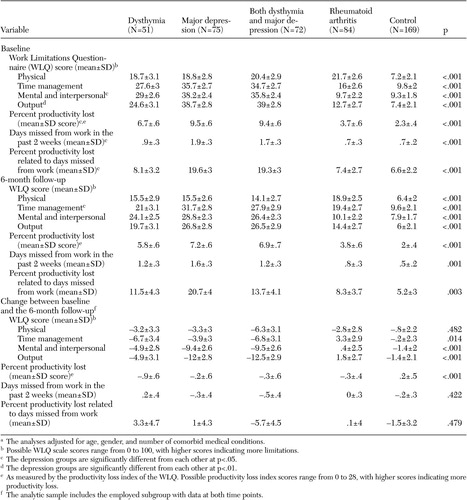 |
Table 3. Comparison of baseline and follow-up measurements among 451 participants who were employed at follow-up in a study ofwork outcomes of employees with depression, by conditiona
a The analyses adjusted for age, gender, and number of comorbid medical conditions.
1. Murray CJL, Lopez AD: The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Geneva, Switzerland, World Health Organization, 1996Google Scholar
2. Kessler RC, Greenberg P, Mickelson K, et al: The effects of chronic medical conditions on work loss and work cutback. Journal of Occupational and Environmental Medicine 43:218–225, 2001Crossref, Medline, Google Scholar
3. Stewart WF, Ricci JA, Chee E, et al: Cost of lost productive work time among US workers with depression. JAMA 289:3135–3144, 2003Crossref, Medline, Google Scholar
4. Greenberg PE, Kessler RC, Birnbaum HG, et al: The economic burden of depression in the United States: how did it change between 1990 and 2000? Journal of Clinical Psychiatry 64:1465–1475, 2003Google Scholar
5. Zhang M, Rost KM, Fortney JC, et al: A community study of depression treatment and employment earnings. Psychiatric Services 50:1209–1213, 1999Link, Google Scholar
6. Simon GE, Revicki D, Heiligenstein J, et al: Recovery from depression, work productivity, and health care costs among primary care patients. General Hospital Psychiatry 22:153–162, 2000Crossref, Medline, Google Scholar
7. Schoenbaum M, Unutzer J, Sherbourne C, et al: Cost-effectiveness of practice-initiated quality improvement for depression: results of a randomized controlled trial. JAMA 286:1325–1330, 2001Crossref, Medline, Google Scholar
8. Kroenke K, West SL, Swindle R, et al: Similar effectiveness of paroxetine, fluoxetine, and sertraline in primary care: a randomized trial. JAMA 286:2947–2955, 2001Crossref, Medline, Google Scholar
9. Employment, Hours, and Earnings From the Current Employment Statistics Survey (State and Metro Area). US Department of Labor, Bureau of Labor Statistics. Available at http://www.bls.govGoogle Scholar
10. Lerner D, Adler DA, Chang H, et al: The clinical and occupational correlates of work productivity loss among employed patients with depression. Journal of Occupational and Environmental Medicine 46:S46-S55, 2004Google Scholar
11. Yelin E, Meenan R, Nevitt M, et al: Work disability in rheumatoid arthritis: effects of disease, social, and work factors. Annals of Internal Medicine 93:551–556, 1980Crossref, Medline, Google Scholar
12. Bush B, Shaw S, Cleary P, et al: Screening for alcohol abuse using the CAGE questionnaire. American Journal of Medicine 82:231–235, 1987Crossref, Medline, Google Scholar
13. Composite International Diagnostic Interview (CIDI). World Health Organization. Available at http://www3.WHO.int/cidi/index.htmGoogle Scholar
14. Rogers WH, Wilson IB, Bungay KM, et al: Assessing the performance of a new depression screener for primary care (PC-SAD). Journal of Clinical Epidemiology 55:164–175, 2002Crossref, Medline, Google Scholar
15. Spitzer RL, Kroenke K, Williams JB: Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study: Primary Care Evaluation of Mental Disorders: Patient Health Questionnaire. JAMA 282:1737–1744, 1999Crossref, Medline, Google Scholar
16. Lerner D, Amick BC III, Rogers WH, et al: The Work Limitations Questionnaire. Medical Care 39:72–85, 2001Crossref, Medline, Google Scholar
17. Loeppke R, Hymel PA, Lofland JH, et al: Health-related workplace productivity measurement: general and migraine-specific recommendations from the ACOEM Expert Panel. Journal of Occupational and Environmental Medicine 45:349–359, 2003Crossref, Medline, Google Scholar
18. Lerner D, Amick BC III, Lee JC, et al: Relationship of employee-reported work limitations to work productivity. Medical Care 41:649–659, 2003Medline, Google Scholar
19. Kroenke K, Spitzer RL, Williams JB: The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine 16:606–613, 2001Crossref, Medline, Google Scholar
20. Stewart AL, Ware JE Jr: Measuring Functioning and Well-Being: The Medical Outcomes Study Approach. Durham and London, Duke University Press, 1992Google Scholar
21. Ware JE Jr, Kosinski M, Keller SD: SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. Boston, Health Institute, New England Medical Center, 1995Google Scholar
22. 2001 National Occupational Employment and Wage Estimates. US Department of Labor, Bureau of Labor Statistics. Available at www.bls.gov/oes/2001/oes_nat.htmGoogle Scholar
23. Stata Reference Manual. College Station, Tex, Stata Press, 2001Google Scholar
24. Depression Guidelines Panel: Depression in Primary Care: Volume 1. Detection and Diagnosis: Clinical Practice Guidelines Number 5. Rockville, Md, Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, 1993Google Scholar
25. Depression Guidelines Panel: Depression in Primary Care: Volume 2. Treatment of Major Depression: Clinical Practice Guidelines Number 5. Rockville, Md, Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, 1993Google Scholar
26. Mental Health: A Report of the Surgeon General. Rockville, Md, US Center for Mental Health Services, National Institute of Mental Health, 1999Google Scholar
27. Schoenbaum M, Unutzer J, McCaffrey D, et al: The effects of primary care depression treatment on patients' clinical status and employment. Health Services Research 37:1145–1158, 2002Crossref, Medline, Google Scholar
28. Davis JA, Smith TW: The NORC General Social Survey: A User's Guide. Newbury Park, Calif, Sage Publications, 1992Google Scholar
29. MacDonald-Wilson K, Rogers ES, Anthony WA: Unique issues in assessing work function among individuals with psychiatric disabilities. Journal of Occupational Rehabilitation 11:217–232, 2001Crossref, Medline, Google Scholar



