Use of Mental Health Services in Chile
Abstract
OBJECTIVES: To address the growing burden of mental illness in Latin America, a better understanding of mental health service use and barriers to care is needed. Although many Latin American countries have nationalized health care systems that could potentially improve access to care, significant barriers to care remain. The authors report the results of a study examining mental health service utilization in the general population of Chile. METHODS: The data were drawn from the Chile Psychiatric Prevalence Study, a national household survey of 2,987 persons aged 15 years and older conducted in 1992-1999. As part of the survey, psychiatric diagnoses were obtained by using the Composite International Diagnostic Interview, and respondents were asked about their use of general and mental health care services in the past six months and about their experience of barriers to treatment. RESULTS: More than 44 percent of respondents reported use of any health care services in the past six months, and 20 percent reported use of mental health services. Of the respondents who met criteria for a psychiatric disorder, a large proportion (62 percent) did not receive mental health care. Increasing severity of the psychiatric disorder correlated with increasing frequency of overall help seeking, but only a small proportion of the respondents with a psychiatric disorder sought specialized mental health services. Regional disparities and inequities in access to care were found. In addition, indirect barriers to mental health care, such as stigma and misconceptions about the course of psychiatric disorders, were important deterrents to service utilization, particularly among persons with lower socioeconomic status. CONCLUSIONS: To reduce the burden of mental illness in Chile, additional efforts are needed to address both the direct and the indirect barriers to mental health care, including regional inequities in access to care.
The burden of mental illness is of growing concern in Latin America. By the year 2020 the proportion of disability-adjusted life years attributable to neuropsychiatric conditions is expected to be 20.6 percent in Latin America (1). To better understand the mental health needs of the population and to allow better allocation of mental health care resources in Latin America, several studies have been conducted to estimate the prevalence of psychiatric disorders in the community (2,3,4,5,6,7,8). The World Health Organization (WHO) world atlas of mental health resources compiled in 2002 showed a wide disparity between developing and developed countries in the proportions of the health care budget allocated to mental health and in the availability of mental health care resources (9). For example, the proportion of the health care budget allocated to mental health was 1.5 percent in Chile, compared with 11 percent in Canada and 6 percent in the United States. The number of psychiatric beds per 10,000 population was 1.8 in Chile, compared with 19.3 in Canada and 9.5 in the United States.
Utilization of mental health services in Latin America and other developing regions has received only limited attention from researchers. To our knowledge, only three epidemiological studies (3,5,7) using the Composite International Diagnostic Interview (CIDI) (10) have examined rates of mental health service use among persons with psychiatric disorders in Latin American countries. Two of these reports were from Mexico, one representing Mexico City (5) and the other limited to use of services by persons with affective disorders in rural Mexico (7). The third study was from a middle-class catchment area in São Paulo, Brazil (3). Each of these reports suggested a high prevalence of untreated disorders. These studies did not examine determinants of use of mental health care or barriers to care.
Health care in Chile is provided primarily through a public national health service that was established in 1952 as well as through an active private sector. The mental health care system evolved initially with a focus on inpatient care for severely mentally ill patients. More recent trends have included efforts to encourage deinstitutionalization, increase the use of general medical facilities for psychiatric treatment, and promote psychiatric treatment at the primary care level. In the past decade a formal national mental health care plan was developed to reorganize the delivery of services, and a division within the Ministry of Health was created to assume responsibility for the mental health care budget and the allocation of mental health care resources. Publicly funded inpatient and outpatient mental health services, including services provided in the primary care sector, have been established in each of the 28 health care districts in the country. Primary care facilities responsible for a geographically defined catchment area are widely distributed to provide coverage to small population centers as well as rural areas. In addition to a primary care physician, a nurse, and a social worker, each of these primary care centers has a mental health team funded through national programs, such as the National Program on Depression, that treat mild to moderate cases. Individuals with serious mental illness are managed in nearby psychiatric facilities, which have outpatient clinics. Beyond deinstitutionalization, the goal of the national mental health care plan was to address the growing burden of mental illness by providing services to a wider range of persons in the community who need psychiatric treatment, not only to those with severe mental illness.
This report draws on data on mental health service use and barriers to mental health care collected as part of the Chile Psychiatric Prevalence Study. The study was conducted in 1992-1999 to determine the prevalence of and risk factors for mental illness in a nationally representative sample.
Methods
Sample selection
The Chile Psychiatric Prevalence Study was based on a stratified household sample of persons aged 15 years and older. In Chile, persons aged 15 years and older are considered adults within the health service system. Four of the 13 regions of the country were sampled to obtain a sampling frame representative of the national population. Within each region the province whose population was most representative of that region of the country was selected. These four provinces represented geographically distinct regions of the country: Santiago, the capital, which is located in the north central region and includes a third of the nation's population; Concepción, the country's second largest city, which is located in the south central region; Iquique, a less populated province located in the north; and Cautin, a less populated province located in the south. As Table 1 shows, the availability of services in the public health sector varied markedly across these four provinces. In Chile, provinces are subdivided into comunas, subsequently into districts, and then into blocks. Within each province, blocks were randomly selected for inclusion in the study. The 1992 national census was used to determine the number of households in each comuna and thereby the number of blocks needed. The Kish procedure was used to select one person per household (11).
The department of psychiatry and mental health at the University of Concepción conducted the study between July 1992 and June 1999, with the four sites of Concepción, Santiago, Iquique, and Cautin each being completed sequentially as funding was secured. The response rate was 90.3 percent, and a total of 2,987 persons participated in the study.
Interview schedule
Versions 1.0 and 1.1 of the CIDI were the primary instruments used by the interviewers to conduct the diagnostic interview in the Chile Psychiatric Prevalence Study. The instruments were translated into Spanish by using the protocol outlined by WHO (12), and the translated instruments subsequently became WHO-approved Spanish versions of the CIDI. Validation studies of the Spanish versions reported kappas ranging from .52 for somatoform disorders to .94 for affective disorders (13). Similar procedures were used to develop a validated translation of the section on posttraumatic stress disorder (PTSD) of the Diagnostic Interview Schedule (14), which was also used in the diagnostic interview. The validation study for this section reported a kappa of 0.63 (15).
The psychiatric diagnoses were based on the DSM-III-R (16). This analysis focused on one-year prevalence of any psychiatric disorder. The disorders that were included were nonaffective psychosis, major depression, mania, dysthymia, panic disorder, agoraphobia, PTSD, somatoform disorder, alcohol abuse, alcohol dependence, drug abuse, and drug dependence. The severity of a psychiatric disorder was rated with an index based on the diagnosis and the extent of comorbidity (17). The severity index was modified for use in Chile to account for culturally appropriate clinical presentations and the inclusion of nonaffective psychosis, PTSD, somatoform disorders, and cognitive disorders. A severity score of .5 was assigned to substance abuse and to somatoform disorder. A score of 1 each was given to cognitive disorder, substance dependence, dysthymia, agoraphobia, and generalized anxiety disorder. Panic disorder, PTSD, mania, and depressive disorder each received a score of 2, and nonaffective psychosis received a score of 3. An additive summary score for severity was generated, with cutoff points of 0, 1, 2, and 3.
The interview schedule also included a section on health service use in the six months before the interview. Respondents were asked about their use of any health care services; any mental health care services—which included specialized mental health care and nonspecialized mental health care; and substance abuse services. Specialized mental health care included any inpatient or outpatient services provided by a psychiatrist or a psychologist or formal substance abuse services; nonspecialized mental health care focused on care provided by primary care physicians; and substance abuse services included inpatient and outpatient detoxification as well as attendance at Alcoholics Anonymous. Questions about the use of public- and private-sector services, formal and informal health care, and barriers to care for physical and psychiatric problems were included. For barriers, respondents chose from a list of reasons they might not have sought care.
The institutional review board of the University of Concepción approved the study. All interviewed respondents provided formal informed consent.
Data analysis
The percentages reported here were weighted to account for two factors: the probability that the comuna, district, block, household, and respondent would be selected for the sample and the distribution of age groups, gender, and marital statuses in the general population according to the 1992 national census. Because of the characteristics of the sample and the need for weighting, standard errors were estimated by using the Taylor series linearization method included in the SUDAAN statistical package (18). Chi square and logistic regression analyses were used in the data analysis.
Results
More than 44 percent of the respondents used some form of health care services during the past six months. Approximately 17.7 percent of the population received nonspecialized mental health services during the past six months, and only 5.6 percent of the population received services delivered by the specialized mental health system. During this period 3.3 percent of the population had spent at least one day in a hospital as a result of a psychiatric or a general health condition.
Women were more likely than men to seek any health care services (44.2 percent compared with 39.3 percent; χ2=6.95, df=1, p<.02) and to seek nonspecialized mental health services (17.7 percent compared with 11.2 percent; χ2=10.84, df=1, p<.003). Gender differences were not found for specialized mental health services. Respondents in different age groups had different rates of service use, with respondents aged 55 to 64 years having the highest rate of use of any health care services (55.5 percent; χ2=20.52, df=5, p<.005) and respondents aged 15 to 24 years having the highest rate of use of specialized mental health care (8.6 percent; χ2= 9.70, df=5, p<.006). In the analysis of marital status, widowed respondents were found to use the most health care services overall (52.5 percent; χ2=14.39, df=4, p<.02), and those in a common-law relationship had the highest rate of use of specialized mental health services (9.5 percent; c2=3 1.76, df=4, p<.001). Education and income did not predict service use. Regional differences were found in health care use, but no differences were found between urban areas and rural areas. Respondents in Cautin had the least use of any health care in the past six months (36.1 percent; χ2= 19.26, df=3, p<.002), as well as the least use of nonspecialized mental health care (11.1 percent; χ2=13.28, df=3, p<.01). The rate of use of any mental health services was 22.5 percent in Santiago, 18.5 percent in Concepción, 26.1 percent in Iquique, and 12.1 percent in Cautin. The rates of use of specialized mental health services in the four locations were 5.2 percent, 6.8 percent, 5.6 percent, and 3.4 percent, respectively.
The one-year prevalence of mental illness in Chile was 19.3 percent. As Table 2 shows, having a psychiatric diagnosis was predictive of mental health service use but not of use of overall health care services. Although respondents with a psychiatric diagnosis had a higher rate of hospitalization in the past six months (6.4 percent) than those without a psychiatric diagnosis (2.4 percent), the difference was not statistically significant (χ2=3.94, df=1, p<.06).
The one-year prevalence of a severity index score of 0 was 74.4 percent, and the rates were 13.8 percent for a severity index score of 1, 5.8 percent for a score of 2, and 5.9 percent for a score of 3. Higher severity index scores were associated with higher rates of mental health service use (Table 2).
When asked to identify someone who could provide assistance with mental health issues, most respondents did not identify alternatives outside the formal health care system. For example, talking with a friend was endorsed by 14.3 percent of the respondents, and talking with a member of the clergy was endorsed by only 2.7 percent of the respondents. In addition, consulting a curandero, or folk healer, was endorsed by only 1.2 percent of the respondents.
More than one-fourth of the respondents (26.5 percent) who had a medical consultation in the past six months reported that emotional issues were discussed. Forty-three percent of the medical appointments had not been made to address a psychiatric issue. Of those who did not seek medical attention, 28.5 percent acknowledged that they should have done so for a physical problem and 12.7 percent acknowledged that they should have done so for a psychological problem.
Table 3 lists reasons endorsed by respondents for not seeking treatment for physical or emotional problems. A forward logistic regression was conducted by using the data on each barrier to care to determine which sociodemographic factors were associated with lower rates of help seeking for emotional disorders. Gender and presence of a diagnosis did not predict endorsement of any of the barriers to care. Respondents with the lowest level of education were more likely to believe that their problems would resolve on their own. Concern about financial barriers to care was highest in the groups with the lowest levels of education and income. Not knowing where one should go for assistance was noted most frequently among the lowest-income group. Married persons and those with lower incomes were more likely to believe that treatment would not be helpful. Lack of transportation was more frequently endorsed as a barrier to care by married persons. Being preoccupied about what others might think was of greatest concern among those who were married as well as among those with the least education. Low levels of income and education were associated with the belief that consulting a mental health professional was too time-consuming. Concern about others' learning about the consultation was greatest among those with a lower level of education and those who were married. Persons who were younger were more likely to believe that they could solve their problems on their own. Fear of receiving a diagnosis was highest among the lowest-income group. No predictors were found for lack of trust in mental health care professionals.
Discussion
This study represents the only examination of mental health care service use and barriers to care in a nationally representative sample of the population of a Latin American country. Despite its scope, the study has some limitations that must be considered in interpreting the findings. The psychiatric diagnoses were obtained by using a structured diagnostic instrument administered by lay interviewers. Reporting bias and the lack of a clinical assessment by a mental health care professional may have resulted in misclassification of persons who received treatment as not having a psychiatric diagnosis. The time lag in collecting data from each site could account for regional differences. However, we believed that this interpretation was unlikely because one of the sites in the southern part of the country was the first to participate and the other southern site was the last, yet the results for the two sites were similar. In addition, the limited availability of services in these regions corresponded with the increased rates of untreated illness found for those regions. The interview schedule did not include questions on lifetime use of services or on the use of pharmacologic and psychotherapeutic interventions.
Although utilization of overall health care services in Chile was high, most people with psychiatric disorders did not receive treatment. Approximately 61.5 percent of the respondents who met criteria for a psychiatric disorder in the past year did not receive mental health care. Even among those with the most severe disorders, such as nonaffective psychosis or comorbid disorders, 35 percent did not receive care. Only 13 percent of the respondents with a psychiatric disorder received specialized mental health services, and more than 70 percent of those with severe mental illness, as defined by the severity scale, did not receive care from mental health specialists. These findings are consistent with the results of regional surveys in Mexico (5) and Brazil (3) that suggested a large gap between the need for treatment and treatment received. Despite the popular belief that alternative sources of health care, such as curanderos or the clergy, are frequently consulted in place of or in conjunction with the formal health care system in Latin America, the study findings suggest that, at least in Chile, such alternatives are not commonly used.
The sociodemographic predictors of mental health service use included female gender, being in the age group at risk of the onset of mental illness, and having a common-law relationship. The regional differences in health care use were consistent with the limited availability of both specialized and nonspecialized health care in the poorer southern half of the country (Table 1). These marked differences across the country are consistent with the profound inequities frequently found within developing nations, where services are generally centralized in the capital region and wealthier areas.
The primary direct barrier to mental health care in Chile was the lack of available services. The lack of services was further highlighted by the finding that 29 percent of the respondents reported not knowing where to go to receive assistance. In addition, despite the presence of a national health care plan in Chile, financial barriers precluded many respondents from seeking assistance. To a lesser degree, time constraints and lack of transportation were direct barriers to care. Indirect barriers that discourage treatment were prominent. Most respondents—more than two-thirds of the sample—had the misconceptions that psychiatric illnesses are self-limiting disorders that resolve on their own and that one can deal with these illnesses on one's own. A sizable proportion did not believe that psychiatric treatment could be helpful. Stigma was an important indirect barrier to treatment, as shown by the findings that one-third of the respondents were fearful of receiving a diagnosis of a mental illness and that nearly one-quarter reported concern about what others might think or that someone would learn about their mental health consultation. Lower socioeconomic status, as evidenced by lower levels of education and income, was highly predictive of endorsement of indirect barriers that reduce the likelihood of seeking help. Although the findings for barriers to care were similar to those of other studies (17), gender was not associated with particular reasons for not seeking professional help.
Similar to findings for other countries (19), use of mental health services was reported by a large percentage of the respondents who did not meet criteria for a psychiatric disorder according to the CIDI. Respondents without a disorder constituted 56.9 percent of those who used mental health services. In comparison, 33.9 percent of the respondents in the U.S. National Comorbidity Study who did not have a disorder received care (20). Such persons could have subthreshold psychiatric disorders that do not meet diagnostic criteria but need to be treated, or they could have met diagnostic criteria at some point but, as a result of successful treatment, no longer do so. In addition, it may be argued that the presence of a national health care service and the reorganization of mental health services to emphasize treatment in the primary care system may have reduced barriers to care for those who have mild conditions that do not warrant attention in specialty care.
If developing countries are to successfully reduce the disability associated with mental disorders, much more emphasis needs to be placed on addressing both the direct and the indirect barriers that persist. WHO (21) has outlined ten recommendations for developing countries to implement in order to reduce the treatment gap in mental health: make mental health treatment accessible in primary care; make psychotropic drugs readily available; shift care away from institutions toward community care; educate the public; involve family, communities, and consumers; establish national mental health programs; increase and improve the training of mental health professionals; increase links with other governmental and nongovernmental institutions; provide monitoring of the mental health system with quality indicators; and provide additional support for research.
Acknowledgment
This work was supported by grants 90-229, 92-233, 1971315, and 1990325 from Fondo Nacional de Desarrollo Científico y Tecnológico (Chile) and grant 201.087.027-1.0 from the Dirección de Investigación de la Universidad de Concepción (Chile). The authors thank the Pan American Health Organization/ World Health Organization for additional technical and financial support.
Dr. Saldivia, Dr. Vincente, Dr. Rioseco, and Mr. Torres are with the department of psychiatry and mental health at the University of Concepción in Concepción, Chile. Dr. Kohn is with the department of psychiatry and human behavior at Brown University in Providence, Rhode Island. Send correspondence to Dr. Saldivia at Universidad de Concepción, Departamento de Psiquiatria y Salud Mental, Casilla 60-C, Concepción, Chile (e-mail, [email protected]).
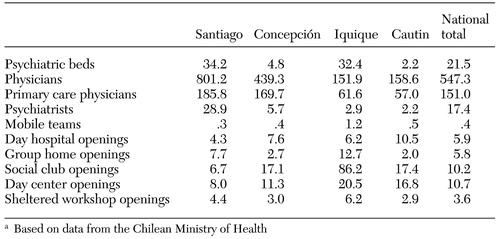 |
Table 1. Public-sector mental health service resources per 100,000 population in four Chilean provinces and nationwide in Chile, 2001a
a Based on data from the Chilean Ministry of Health
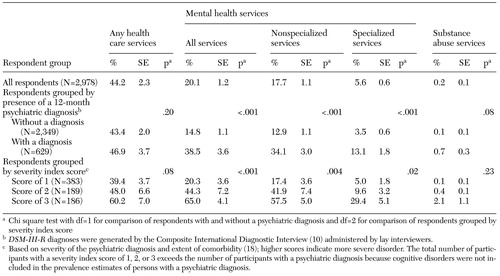 |
Table 2. Use of services in a representative sample of the general population of Chile who participated in a household survey on the prevalence of psychiatric disorders, 1992–1999
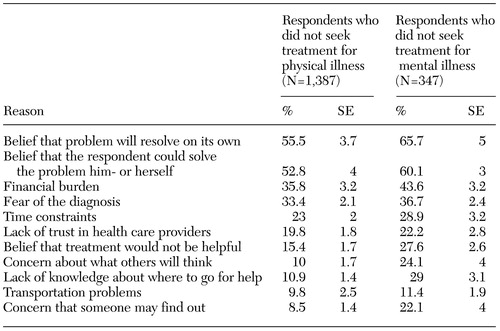 |
Table 3. Reasons for not seeking treatment for physical and mental illness among respondents who acknowledged the need for treatment in a representative sample of the general population of Chile who participated in a household survey on the prevalence of psychiatric disorders, 1992–1999
1. Murray CJL, Lopez AD (eds): The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, Mass, Harvard School of Public Health, 1996Google Scholar
2. Almeida-Filho N, Mari JJ, Coutinho E, et al: Brazilian multicentric study of psychiatric morbidity: methodological features and prevalence estimates. British Journal Psychiatry 171:524–529, 1997Crossref, Medline, Google Scholar
3. Andrade LH, Walters EE, Gentil V, et al: Prevalence of ICD-10 mental disorders in a catchment area in the city of São Paulo, Brazil. Social Psychiatry and Psychiatric Epidemiology 37:316–325, 2002Crossref, Medline, Google Scholar
4. Araya R, Rojas G, Fritsch R, et al: Common mental disorders in Santiago, Chile: prevalence and socio-demographic correlates. British Journal of Psychiatry 178:228–233, 2001Crossref, Medline, Google Scholar
5. Carveo-Anduaga JJ, Martinez NA, Rivera BE, et al: Prevalencia en la vida de episodios depresivos y utilización de servicios especializados [Lifetime prevalence of depressive episodes and specialized service utilization]. Salud Mental 20(2):15–23, 1997Google Scholar
6. Hayashi S, Perales A, Sogi C, et al: Prevalencia de vida de trastornos mentales en Independencia (Lima, Peru) [Lifetime prevalence of psychiatric disorders in Independencia]. Anales de Salud Mental 1:206–222, 1985Google Scholar
7. Salgado de Snyder VN, Diaz-Pérez M: Los trastornos afectivos en la población rural [Affective disorders in a rural population]. Salud Mental 22(número especial):68–74, 1999Google Scholar
8. Vicente B, Rioseco P, Saldivia S, et al: Estudio Chileno de prevalencia de patología psiquiátrica (DSM-III-R/CIDI) (ECPP) [Prevalence of psychiatric disorder in Chile]. Revista Médica de Chile 130:527–536, 2002Medline, Google Scholar
9. Atlas: Mental Health Resources in the World. Geneva, World Health Organization, 2002 (www.cvdinfobase.ca/mh-atlas/)Google Scholar
10. Robins LN, Wing J, Wittchen HU, et al: The Composite International Diagnostic Interview: an epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry 45:1069–1077, 1988Crossref, Medline, Google Scholar
11. Kish L: Survey Sampling. New York, Wiley, 1965Google Scholar
12. Sartorius N, Kuyken W: Translation of health status instruments, in Quality of Life Assessment in Health Care Settings, Vol 1. Edited by Orley J, Kuyken W. Berlin, Springer, 1994Google Scholar
13. Vielma M, Vicente B, Rioseco P, et al: Validación en Chile de la entrevista diagnóstica estandarizada para estudios epidemiológicos CIDI [Chilean validation of a standardized diagnostic instrument for epidemiological studies]. Revista de Psiquiatría 9:1039–1049, 1992Google Scholar
14. Robins LN, Helzer JE, Croughan J, et al: National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Archives of General Psychiatry 38:381–389, 1981Crossref, Medline, Google Scholar
15. Rioseco P, Vicente B, Uribe M, et al: El DIS-III-R: una validación en Chile [The DIS-III-R: a validation in Chile]. Revista de Psiquiatría 9:1034–1038, 1992Google Scholar
16. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 3rd ed., rev. Washington DC, American Psychiatric Association, 1987Google Scholar
17. Bjil RV, de Graff R, Hiripi E, et al: The prevalence of treated and untreated mental disorders in five countries. Health Affairs 22(3):122–133, 2003Google Scholar
18. Shah BV, Barnwell BG, Bieler GS: SUDAAN User's Manual. Release 7.5. Research Triangle Park, NC, Research Triangle Institute, 1997Google Scholar
19. Meltzer H, Bebbington P, Brugha T, et al: The reluctance to seek treatment for neurotic disorders. International Review of Psychiatry 15:123–128, 2003Crossref, Medline, Google Scholar
20. Kessler RC, Zhao S, Katz SJ, et al: Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. American Journal of Psychiatry 156:115–123, 1999Link, Google Scholar
21. The World Health Report 2001: Mental Health: New Understanding, New Hope. Geneva, World Health Organization, 2001Google Scholar



