A Study of Long-Stay Patients Resettled in the Community After Closure of a Psychiatric Hospital in Italy
Abstract
OBJECTIVE: This study examined the outcomes of all patients who were discharged from an Italian psychiatric hospital into community residences three to four years after discharge. METHODS: The total population of Antonini Mental Hospital near Milan on January 1996 (N=337) was assessed by using the expanded Brief Psychiatric Rating Scale and the overall social behavior and social role functioning sections of the Disability Assessment Schedule. The hospital closed in 1999, and all patients who were resettled in the community were reassessed in September 2002. Residential stability, use of inpatient services, and mortality were also investigated. RESULTS: Of the 337 patients, 64 died before discharge, 110 were transferred to nursing homes, and 163 were discharged to the community. The follow-up of patients who moved to the community showed no differences in psychopathology or social role functioning. In terms of overall social behavior, a significant increase was observed in the number of patients with mild or no disability, and a corresponding decrease was observed in the number with moderate disability. Most patients showed residential stability. The rate of postdischarge mortality was low, and there were no deaths due to accident or suicide. The number of admissions to acute psychiatric wards was limited. CONCLUSIONS: A population characterized by a long history of illness and severe disability underwent a radical change in care setting and living arrangement with favorable outcomes, as indicated by the absence of adverse events or clinical deterioration and by some improvement in social behavior. The results confirm that most long-stay patients can successfully leave psychiatric hospitals and live in community residences.
Substantial changes in the delivery of mental health services over the past several decades have led to the downsizing or closure of many psychiatric hospitals in a number of western countries. In Italy this process started in the mid-1970s and was completed in 2000, when the last group of long-term patients was discharged.
Although some articles have been published on the shift to community care in Italy (1,2), empirical findings on the effects of closing psychiatric hospitals are limited. Some surveys examined specific aspects, such as patients' destination at discharge (3), mortality rates (4), and changes in service provision after hospital closure (5). However, few data are available on clinical and social outcomes of discharged long-stay inpatients.
We addressed this issue by conducting a prospective follow-up study of patients who were transferred to community care during the process of closing a large Italian psychiatric hospital. The patients received a comprehensive assessment before discharge planning and were reassessed three to four years after resettlement in a range of accommodation in the community. Patients' status before discharge was compared with their follow-up status in terms of psychopathology and social disability. A set of outcome indicators were also examined, including mortality, residential stability, and hospital admission.
Methods
This study took place in the Antonini Mental Hospital, which is located on the outskirts of the Milan metropolitan area in Northern Italy. In accordance with the provisions of the Italian Mental Health Act, the hospital discontinued admissions of new patients in 1978 and stopped acute readmissions in 1983. However, a few long-term patients were readmitted up until 1995. In 1995 the hospital was scheduled for closure and a project was set up to enable discharge of all patients by the end of 1999. In January 1996 all 337 inpatients (178 men and 159 women) underwent a comprehensive evaluation. Sociodemographic and clinical data were collected, diagnoses were revised by expert psychiatrists according to ICD-10 (6), symptoms were assessed by using the 24-item expanded Brief Psychiatric Rating Scale (BPRS) (7), and social disability was assessed by using the Disability Assessment Schedule (DAS) (8). Both instruments were administered by a multidisciplinary team of clinicians. Interrater reliability was tested in a subsample of patients; k coefficients were .69 for the BPRS and .63 for the DAS, slightly lower than those reported in field studies of the Italian versions of these two instruments (9,10).
The hospital closure plan was defined in 1996, and in 1998 the first group of patients was discharged. In December 1999 the last patients left the hospital, which was finally closed. A total of 64 patients died before discharge. Thus 273 patients were discharged, of whom 110 were placed in nursing homes or institutions for persons with mental retardation, two joined their families, and 161 entered a range of community-based residences that provided different levels of care. Such facilities, located in suburban neighborhoods within walking distance of recreational areas, shops, and public transportation, provided three different types of living arrangements: residential care units (four facilities), which are purposely built units with 18 to 20 beds and which are staffed on a 24-hour basis, for the most difficult patients; group homes (eight facilities), which provide lodging for between four and eight people, with regular staff providing eight- to 12-hour coverage during the day; and cluster block apartments (15 facilities), which provide lodging for between two and four people with higher levels of autonomy who receive flexible support on a daily basis in relation to specific treatment and rehabilitation programs. Of the patients in the sample, 62 went to residential care units, 51 to group homes, and 48 to apartments. Residents had access to local medical services, and case management and mental health care were provided by multidisciplinary teams attached to the community psychiatric services.
Follow-up was conducted in September 2002, six years after the baseline assessment and three to four years after discharge. All patients who were accommodated in community residences plus the two who went to their own homes were included. Twenty-two patients died after discharge and before the follow-up evaluation, and four could not be traced—three moved out of the region, and one was homeless. Thus the analysis of symptoms and social functioning was based on data for 137 patients, whereas the analyses of residential stability and service use were based on data for the entire sample of 337.
The BPRS and the DAS were administered by trained psychologists who were not directly involved in patients' care. Here we present data on BPRS total scores and on scores of sections of the DAS covering overall behavior and social role functioning. The BPRS scores were grouped into three categories for the analysis: less than 35 (absent or mild symptoms), 35 to 65 (moderate symptoms), and greater than 65 (severe symptoms). Scores on the DAS sections were collapsed into the categories of <1 (no or mild disability), 1<2 (moderate disability), and ≥2 (severe disability). BPRS and DAS scores at baseline and follow-up were compared by estimating effect sizes as a measure of difference between the means (11).
Results
The characteristics of the entire hospital population and of the cohort who moved to community accommodation are summarized in Table 1. The patients who moved to community accommodation were slightly younger and had shorter stays than the overall group of patients who were in the hospital before the closure process started. However, this subset of patients had all the features of a very chronic institutionalized population. During the follow-up period, 35 of the discharged patients (22 percent) had at least one admission to an acute psychiatric ward, with a total of 79 admissions and 700 inpatient days, corresponding to a crude admission rate of 7 percent. These patients occupied an average of .7 beds daily, or 2.3 percent of the available beds in acute inpatient services in the area. Twenty-two of the 163 patients died, with a postdischarge crude mortality rate of 4.4 percent. At follow-up 112 patients (79 percent of the living patients) were still in the same place in which they had been accommodated at discharge, and 29 (21 percent) had moved at least once. Changes of residence involved mainly a move from one community facility to another. Only six patients (4 percent) were transferred to nursing homes because of increasing physical disability.
BPRS and DAS scores are shown in Table 2. At follow-up no statistically significant differences were observed in the number of patients in the various categories of symptom severity or in the mean BPRS scores, as indicated by the very small effect size.
The reduction in mean scores on the two sections of the DAS was modest and not significant. Moreover, the data had a skewed distribution. Nevertheless, in terms of overall social behavior, the number of patients with mild or no disability increased significantly, whereas the number with moderate disability decreased significantly.
Discussion
This study has several unique features. First, it is currently the only study to provide outcome results for an entire unselected cohort of patients discharged from a single psychiatric hospital in Italy. Second, the study focused on an aged population with a very long history of illness. Third, it studied a closure process as it was carried out in a typical "real-world" service setting. Fourth, the study was conducted in a service system in which the readmission of patients to the psychiatric hospital was not possible.
The limitations of the study relate primarily to its naturalistic design and to the way in which the data were collected. The data were collected by nonindependent professionals who were not blinded to the patients' status. Moreover, information about patients' physical health, other than death rate, was not available. Finally, patients' satisfaction and quality of life were not assessed.
With these caveats in mind, our findings indicate that few changes in patients' conditions were observed: symptoms were unmodified, impairment in social role functioning remained the same, and a slight improvement in basic living skills was found only for patients with moderate levels of disability at baseline. Data were missing for only one patient, and the rate of admission to acute inpatient services was low. No death from suicide or accident was registered.
The improvement in overall behavior, although small, should not be overlooked. The lack of any improvement in social role functioning was largely expected, because most patients had no opportunity to fulfill any work or family role. The benefits of community care were more evident for the subgroup with intermediate-level functioning, whereas no effect was observed for the most seriously disabled patients. As a result, at follow-up the heterogeneity of the sample in terms of social disability was markedly increased.
Although a host of articles about the closure of psychiatric hospitals have been published, few studies have assessed the outcome of an entire long-stay population discharged to the community from a single hospital by using a prospective longitudinal design (12). McGrew and colleagues (13) examined the functioning of long-stay patients after the closure of the Central State Hospital in Indiana. Leff and the TAPS group (14), in a series of articles, provided comprehensive data on patients who were discharged from Friern and Claybury hospitals in London, England. Rothbard and colleagues (15) investigated the outcomes of community care for patients who left the Philadelphia State Hospital. However, the latter study was concerned mainly with service use and costs.
On the whole, our data confirm the findings of the above-mentioned studies, despite some differences in patients' characteristics and assessment methods—that is, even persons who have been hospitalized for extremely long periods can do well in community settings. Although the clinical picture of these patients is not substantially modified, some improvement in their functioning can be expected.
However, a striking difference between our findings and those of previous studies concerns service use data. The annual admission rate to inpatient services of 7 percent in our sample is low compared with the 27 percent found by McGrew and colleagues (13), the 15 percent found in the TAPS project (16), and the 30 percent reported by Rothbard and colleagues (15). Although the difference can be partly accounted for by some features of our patient population, which comprised patients with very chronic illness and a relatively stable symptom profile, the difference can also be considered a result of a care system characterized by housing opportunities suitable for persons with mental illness and the integration of the residential care team within the local mental health services, with easy access to the various service components.
The feasibility of care for patients with severe mental disorders in noninstitutional settings can no longer be questioned. The provision of residential care in Italy is now considerable (5), and new issues need to be addressed, such as the therapeutic and rehabilitative function of such facilities for younger patients who do not have institutional experience, integration with other community services and agencies, costs, and process and outcome quality indicators. Last, but not least, the possibility that residential facilities, although community based, reproduce institutional styles of care and functioning should not be overlooked, particularly in facilities with more patients and a greater intensity of care.
Conclusions
In summary, this patient group underwent a radical change of care and environment—from an old-fashioned large institution to small homelike residences in the community—and demonstrated good stability in the new accommodations and fairly good outcomes, as indicated by the absence of unfavorable events. It is worth noting that more than 60 percent of this population was resettled in facilities with low levels of supervision, and thus many patients lived in conditions of considerable independence and autonomy.
Dr. Barbato and Dr. D'Avanzo are affiliated with the epidemiology and social psychiatry unit of Mario Negri Institute for Pharmacological Research, Via Eritrea 62, 20157 Milan, Italy (e-mail, [email protected]). Dr. Rocca, Dr. Amatulli, and Dr. Lampugnani are with the department of mental health at Azienda Ospedaliera Salvini in Garbagnate, Italy.
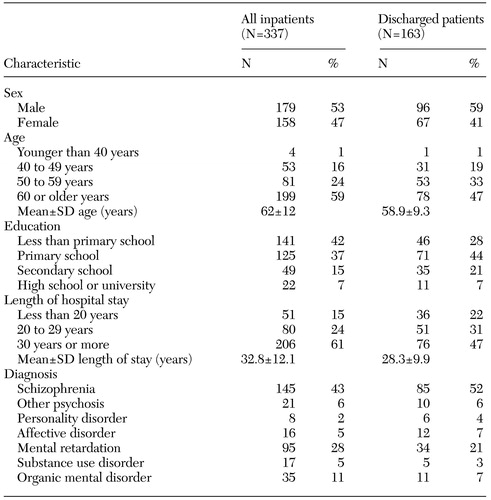 |
Table 1. Baseline characteristics of all inpatients at a psychiatric hospital in Italy and of a subset of patients who were discharged to community settings
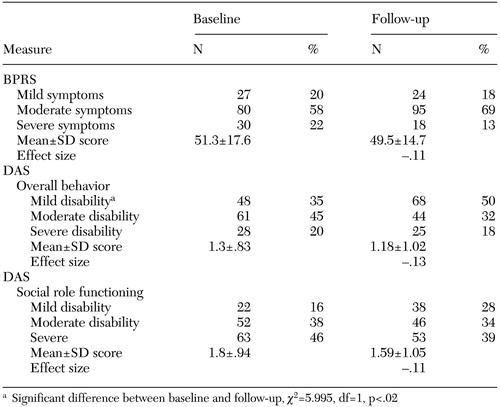 |
Table 2. Scores on the Brief Psychiatric Rating Scale (BPRS) and the Disability Assessment Schedule (DAS) at baseline and follow-up in a sample of 137 psychiatric inpatients in Italy who were discharged to community settings
1. Barbato A: Psychiatry in transition: outcomes of mental health policy shift in Italy. Australian and New Zealand Journal of Psychiatry 32:673–679, 1998Crossref, Medline, Google Scholar
2. Piccinelli M, Politi P, Barale F: Focus on psychiatry in Italy. British Journal of Psychiatry 181:538–544, 2002Crossref, Medline, Google Scholar
3. D'Avanzo B, Barbato A, Barbui C, et al: Discharges of patients from public psychiatric hospitals in Italy between 1994 and 2000. International Journal of Social Psychiatry 49:27–34, 2003Crossref, Medline, Google Scholar
4. D'Avanzo B, Negri E, La Vecchia C: Mortality in long-stay patients from psychiatric hospitals in Italy: results from the Qualyop Project. Social Psychiatry Psychiatric Epidemiology 38:385–389, 2003Crossref, Medline, Google Scholar
5. De Girolamo G, Picardi A, Micciolo R, et al: Residential care in Italy: national survey of non-hospital facilities. British Journal of Psychiatry 181:220–225, 2002Crossref, Medline, Google Scholar
6. The ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research (DCR-10). Geneva, World Health Organization, 1992Google Scholar
7. Ventura J, Green M, Shaner A, et al: Training and quality assurance with the Brief Psychiatric Rating Scale: "the drift busters." International Journal of Methods in Psychiatric Research 3:221–244, 1993Google Scholar
8. WHO Psychiatric Disability Assessment Schedule (WHO/DAS) With a Guide to Its Use. Geneva, World Health Organization, 1988Google Scholar
9. Ardoin MP, Faccincani C, Galati M, et al: Inter-rater reliability of the Disability Assessment Schedule (DAS, version II). Social Psychiatry and Psychiatric Epidemiology 26:147–150, 1991Medline, Google Scholar
10. Roncone R, Morosini P, Casacchia M: The Brief Psychiatric Rating Scale, in How to Assess Outcome in Departments of Mental Health [in Italian]. Edited by Ruggeri M, Dall'Agnola RB. Rome, Italy, Pensiero Scientifico Editore, 2000Google Scholar
11. Cohen J: Statistical Power Analysis for the Behavioral Sciences, 2nd ed. Hillside, NJ, Erlbaum, 1988Google Scholar
12. Rothbard AB, Kuno E: The success of deinstitutionalization: empirical findings from case studies on state hospital closures. International Journal of Law and Psychiatry 23:329–344, 2000Crossref, Medline, Google Scholar
13. McGrew J, Wright ER, Pescosolido BA, et al: The closing of Central State Hospital: long-term outcomes for persons with severe mental illness. Journal of Behavioural Health Services and Research 26:246–260, 1999Crossref, Medline, Google Scholar
14. Leff J, Trieman N: Long-stay patients discharged from psychiatric hospitals: social and clinical outcomes after five years in the community: the TAPS Project 46. British Journal of Psychiatry 176:217–223, 2000Crossref, Medline, Google Scholar
15. Rothbard AB, Kuno E, Schinnar AP, et al: Service utilization and cost of community care for discharged state hospital patients: a 3-year follow-up study. American Journal of Psychiatry 156:920–927, 1999Link, Google Scholar
16. Gooch C, Leff J: Factors affecting the success of community placement: the TAPS Project 26. Psychological Medicine 26:511–520, 1996Crossref, Medline, Google Scholar



