Psychiatric Emergency Services and the System of Care
Abstract
OBJECTIVE: Admissions to psychiatric emergency services have frequently been cited as a gauge of how well a mental health system manages behavioral disorders. However, few measurements of the longitudinal association between psychiatric emergencies and characteristics of a mental health system have been described. The purpose of this study was to assess whether weekly admissions to psychiatric emergency services would increase when outpatient services were reduced, whether weekly admissions would increase when greater effort was made to identify and treat persons with acute mental illness, and whether weekly admissions would decrease when emergency services were enhanced to include postrelease case management. METHODS: Time-series methods were applied to approximately 29,010 admissions to three psychiatric emergency services of the San Francisco Department of Public Health over a 180-week period. RESULTS: Reduced outpatient services, efforts to identify acutely ill persons, and changes in emergency services themselves were found to affect admissions to emergency services. However, community events such as extreme weather, holidays, job loss, and the scheduling of receipt of income also affected the workload of the emergency service. CONCLUSIONS: The causes and course of mental illness inextricably tie a psychiatric emergency service to the overall mental health system and to events in the community it serves. These connections make it possible for managers to anticipate the use of emergency services and to detect disruptions in the remainder of the mental health services systems.
It has often been argued that psychiatric emergency services admit persons whose illness could have been treated with or avoided by outpatient care (1,2,3,4,5,6,7,8,9,10). The literature also suggests that the formal and informal processes by which patients reach an emergency service may impede persons who need treatment from getting it (1,2,3,10). Collectively, this literature implies that changes in admissions to psychiatric emergency services over time can be used to gauge access to and efficacy of all components of the mental health care system. Surprisingly, no empirical tests of this proposition appear in the psychiatric services literature. We aimed to fill a small part of this void by testing three hypotheses: first, that weekly admissions to psychiatric emergency services would increase when outpatient services were reduced; second, that weekly admissions to psychiatric emergency services would increase when greater effort was made to identify and treat persons with acute mental illness; and third, that weekly admissions to psychiatric emergency services would decrease when emergency services were enhanced to include postrelease case management.
Methods
Data
Admissions. Data on emergency admissions were obtained from the management information system of the San Francisco Department of Mental Health. We defined an emergency admission as the decision to provide treatment for a person aged 18 years or older at one of the department's three psychiatric emergency services during the 180 weeks beginning January 1, 1994, and ending July 6, 1997. (The system for recording unemployment claims fundamentally changed in July 1997.) Admissions did not include follow-up visits or visits to have prescriptions rewritten. Any episode during which a patient admitted to an emergency service was also admitted for inpatient psychiatric care was counted as one admission. Informed consent was not required, because the data included no client-level information.
Approximately 29,010 admissions occurred during the study period. About 64 percent of the patients were men. Approximately 54 percent of admissions were of non-Hispanic whites, 22 percent were of African Americans, 10 percent were of Asians or Pacific Islanders, and 9 percent were of Hispanics. About 53 percent were coerced, meaning that treatment was provided under California's civil commitment authority to treat persons believed to be mentally ill and a threat to themselves or others or gravely disabled (11).
Reduction of outpatient services. The San Francisco Department of Public Health identified two documented reductions in outpatient services during the study period. First, a clinic was closed for one week for repairs. We anticipated a lag in the effects of this closure on the grounds that several days would probably pass before symptoms worsened to the level that emergency care was sought. Second, budgetary constraints led to the permanent closure of a clinic that had functioned seven days a week from 9 a.m. to 9 p.m. The effect of this closure might also have been lagged. However, the lag may have been longer for those who needed services spaced at relatively long intervals. For example, patients who needed prescriptions rewritten might have suffered an acute episode up to a month or five weeks after the closure.
Efforts to detect acute mental illness. Two initiatives to identify persons in need of emergency psychiatric services were under way during the study. A mobile crisis clinic opened during the study period and functioned throughout the remainder of the study. Police or fire personnel summoned the mobile crisis clinic when they encountered a person who appeared to be mentally ill. We characterized this effort as "reactive." A second, more aggressive program started before and ended during the study. Teams of police, mental health workers, and social workers sought out homeless persons to offer them services and, if necessary, coerce those with mental illness into treatment. We characterized this program as "proactive."
Enhancements of emergency treatment. Emergency service providers began a dual diagnosis unit to reduce relapse among persons with mental illness and a co-occurring substance use disorder. The unit provided brief but intensive case management for clients on their release from the service. We hypothesized that these enhancements would reduce readmissions. Thus we expected that there could be a lag of a week or two in their effect.
We specified several control variables to avoid spurious associations between the system of care and emergency admissions. For example, data from the Epidemiologic Catchment Area survey indicate that job loss increases the risk of antisocial behavior and alcohol abuse (12,13). The data further suggest that the fear of layoff inhibits these behaviors among persons who remain employed when unemployment unexpectedly increases (12). Consistent with these findings, studies of job loss and coerced treatment due to dangerousness to others in San Francisco and Pittsburgh reported that the coerced treatment increased with unemployment until joblessness exceeded levels that would be expected from seasonal patterns. At that point, the association reversed to form an overall inverted U (11,14).
To avoid spurious associations between job loss and psychiatric emergencies, we specified two variables used in the published research: the number of initial unemployment compensation claims, and the square of this number (11,14). We hypothesized that the coefficient for claims would be positive, because it defines the upward half of the inverted U relationship. We expected the coefficient for the square of claims to be negative, because it defines the downward half.
We also controlled for extreme weather, which impedes access to prophylactic services and social support (15). San Francisco has mild weather, but heavy rain disrupts the normal functioning of the city. We created an "extreme precipitation" variable by first separating into quartiles the 31 weeks during which there was rain. We then scored all weeks with values less than the fourth quartile (3.1 inches of rain) as 0.
We controlled for holidays, which may increase social contact that could reduce the likelihood of acute illness. Moreover, service organizations often provide shelter and food for homeless persons with mental illness during holiday periods, which may also reduce the incidence of acute illness. We created a binary variable scored 1 for the weeks that included New Year's Day, Easter, Independence Day, Labor Day, Veterans' Day, Thanksgiving, and Christmas to test the holiday hypothesis.
We also controlled for phenomena that could induce cycles and trends in emergency admissions. For example, we know that persons who abuse drugs and alcohol frequently do so after receiving income (16). This phenomenon, referred to as the check effect, reportedly increases the incidence of psychiatric emergencies in the first week of each month (17,18,19).
Prescriptions often expire after 30 days. Some patients, particularly men, fail to comply with emergency therapy and experience relapse when their prescriptions expire (20). Thus persons originally admitted because of the check effect and who relapse when prescriptions expire may reinforce the four-week check effect cycle.
Data analysis
The hypothesis that changes in the system of care will affect psychiatric emergencies implies that postchange admissions will differ in the hypothesized direction from those expected under the null hypothesis of no effect. A clinical trial derives values expected under the null hypothesis from a randomly assigned control group. Quasi-experiments such as ours must derive those values through statistical assumptions. The typical assumption is that postchange values will not be outside the 95 percent confidence interval (CI) of the mean of prechange values.
However, observations collected over time often exhibit trends, cycles, and the tendency to remain elevated or depressed after high or low values. These patterns complicate quasi-experiments, because the expected value of a patterned series may not be its mean (21).
Health services researchers have methods for estimating the expected value and confidence interval for patterned time series (22). These methods "decompose" a series into its patterned and residual—or unexpected—components. The test then hinges on whether the residual components are consistent with the hypothesis. The residuals would support the hypothesis that an event will increase a phenomenon if they exceed their 95 percent CI at the times specified a priori as those in which the event should have effect.
We used software available from Scientific Computing Associates (23) to decompose the admissions series into patterned and residual components (24). We then adjusted the residuals by removing any variance shared with the control variables. We inspected the adjusted residuals to determine whether they were above or below, depending on the hypothesis, their 95 percent CI when the changes in care should have had their effects (25,26). If the residuals were outside the CI, we looked for three types of changes in them: permanent increases or decreases, brief increases or decreases that disappeared after one or two weeks, and persistent increases or decreases that decayed slowly to insignificance. A more technically detailed description of the tests is available from the first author.
Results
We separated admissions into four groups defined by gender and by whether treatment was coerced or voluntary. Table 1 shows the weekly mean±SE admissions for these groups. Several patterns that needed to be controlled before the tests could proceed appeared in the admissions series. All but coerced admissions of men exhibited a pattern in which higher or lower than average admissions in any week persisted, although diminished, into the following week. Coerced and voluntary admissions of men exhibited four-week cycles consistent with the check effect (18). Consistent with reports that persistently ill men often fail to comply with treatment and relapse into acute illness (20), we found an eight-week cycle among men coerced into treatment.
Admissions of men and coerced admissions of women also exhibited "echoes" at 26 weeks: relatively high or low admission rates were followed six months later by more or fewer than expected on the basis of immediately preceding weeks.
Control variables
Admissions for all groups were positively related to layoffs but, as expected, negatively related to the square of layoffs. The suspected effect of extreme precipitation on admissions appeared only for voluntarily treated men. Women were less likely to seek voluntary treatment during rainy periods. Precipitation did not predict coerced admissions.
The argument that holidays are salutary appeared consistent with coerced admissions but not voluntary admissions. Coerced admissions of both men and women were fewer than expected during holiday weeks.
Reduction of outpatient services. Tests of the first hypothesis—that reduced outpatient services would coincide with increased admissions—yielded inconsistent results. Only voluntary admissions of men after the permanent closure of a clinic were consistent with the hypothesis (Table 2). The effect was a permanent increase that began in the fifth week after the closure. Voluntary admissions of women also increased in the fifth week after the closure (Table 3). The effect persisted but was not permanent.
However, the remainder of the findings on the effect of reduced outpatient services did not support the hypothesis. In fact, fewer women than expected entered treatment voluntarily during the week of the closure, and fewer either entered or were coerced into treatment during the week after the closure.
Identifying persons in need of emergency care. The second hypothesis—that there would be a relationship between admissions and efforts to identify persons with emergent illness—was true for men but not women. Coerced admissions of men decreased after proactive detection stopped. The effect, which appeared two weeks after the program ceased, persisted. Voluntary admissions of men immediately increased when reactive detection by the mobile crisis clinic began.
The results for women were inconsistent (Table 3). More women voluntarily entered treatment when reactive detection began, but fewer were coerced. The end of proactive detection coincided with more voluntary admissions.
Enhancing emergency services. Adding short-term case management to emergency services for persons with substance abuse coincided with fewer admissions among men, consistent with the third hypothesis (Table 2). The association was immediate for men who were voluntarily admitted and lagged for those who were coerced into treatment. The effect was brief for both groups.
No relationship was observed between emergency service enhancements and the number of women who were voluntarily admitted. More women were coerced into treatment when the service was enhanced, and this effect persisted.
Discussion
Our findings imply that changes in the system of care for persons with mental illness affect admissions to psychiatric emergency services. These changes include changes in the emergency services themselves. We found, for example, that expanding crisis stabilization and postdischarge case management may reduce subsequent emergencies. This finding strengthens the argument that moving from triage to definitive treatment in the psychiatric emergency service may result in better outcomes (9,27).
We also found that the permanent closure of a clinic preceded an increase in voluntary admissions to psychiatric emergency services. Furthermore, we found that the consequences of outreach depend very much on whether the effort is reactive (responding to crises with a mobile clinic) or proactive (seeking out persons who appear to be in need of mental health services). The mobile clinic approach seemed to increase voluntary admissions, whereas outreach led to coerced treatment among male patients.
The remarkable differences in results between men and women deserve consideration in the management of emergency services. Admissions of men supported all our system hypotheses. The permanent closure of an outpatient clinic was associated with a shift upward in the number of men who were voluntarily admitted to emergency treatment. Proactive detection coincided with increased coerced admissions among men. Enhancing emergency treatment for persons with substance abuse coincided with a persistent reduction in voluntary and coerced admissions of men. In combination with findings that assaults in the community decrease when more men are coerced into treatment (28), our findings suggest that mental health services affect the quality of life for people other than clients.
All tests yielded counterhypothetical results for women, with the exception of the association between reactive detection and increased voluntary admissions. Two circumstances suggest a post hoc explanation of the unexpected findings on closure of outpatient facilities. First, the staff of these facilities made great efforts to prepare clients to cope with the closures. Second, women apparently comply more faithfully with treatment plans than men (20). In combination, these two factors may have briefly reduced the use of emergency services by these women.
The literature did not lead us to anticipate that enhanced emergency services for persons who abuse drugs and alcohol coincided with a persistent increase in coerced admissions among women. Persons who live with or support women who have such disorders may have learned of the improved services and become more inclined to bring acutely ill family members and friends to the emergency department.
The finding that community dynamics affect emergency admissions suggests strategies for secondary prevention and program planning. For example, the possible effects of unemployment, holidays, extreme precipitation, or the check effect may initially seem of little interest to service providers. However, further consideration suggests that these findings may be useful. For example, the finding on the check effect suggests that postemergency care might include money management services (29). Case managers might also increase contact with men who have substance use disorders during the early days of the month to further reduce the check effect. The findings on unemployment suggest that service providers could target prevention efforts toward persons who have experienced job loss (30,31)
The findings on holidays and precipitation may shed further light on the community phenomena that affect emergency admissions. The theory that social intercourse reduces the likelihood of psychiatric emergencies is not consistent with the finding that holidays coincided with reductions in coerced but not voluntary admissions. The finding more likely reflects the efforts of service organizations to shelter and care for homeless persons during holidays. The population served by these organizations may be less likely to approach or be brought to the attention of the mental health system.
The finding that voluntary, but not coerced, admissions of men increased with extreme precipitation is consistent with the possibility that men with mental illness seek shelter in clinical facilities during extreme weather. However, we cannot offer a post hoc explanation of the finding that women are less likely to voluntarily enter treatment during such weather.
Our tests had all the shortcomings inherent in quasi-experiments. Chief among these is that discovered associations are only as compelling as the control strategies. Because of the control strategies we used, the associations could not have spuriously arisen from trends, cycles, or other patterns in admissions that happen to coincide with any of our system-of-care variables. Nor were they spuriously induced by labor market conditions, extreme precipitation, or holidays.
Our findings must be replicated elsewhere before they can be taken as strong evidence for or against theory or policy. San Francisco is not necessarily representative of other communities, so the external validity of our findings is unknown. On the other hand, we know of no circumstance that would make our findings peculiar to San Francisco.
Conclusions
The causes and course of mental illness inextricably tie psychiatric emergency services to the overall mental health system and to events in the community. However, the nature of those ties is not always intuitive. Ties between system-of-care variables and emergency admissions appeared to be weaker in San Francisco than we expected on the basis of the literature. The findings suggest to us that the system of care is more plastic, less hydraulic, and perhaps more difficult to manage than the literature implies. For example, the gender differences in the associations we measured were so marked as to suggest that managers should design services that engage men and women differently or risk having countervailing effects.
The associations between emergency admissions and events in the community strike us as useful for practical as well as academic reasons. The results support the general theory that communal disruption affects the use of mental health services if not mental health itself. The results also suggest that managers can anticipate admissions to emergency services and perhaps improve the scheduling of preventive services and other programming.
Acknowledgments
The analyses were supported by grant R01-MH-43579 from the National Institute of Mental Health and by the Center for Mental Health Services Research at the Berkeley and San Francisco campuses of the University of California.
Dr. Catalano and Dr. Thornton are affiliated with the School of Public Health at the University of California, Berkeley, 320 Warren Hall, Berkeley, California 94720 (e-mail, [email protected]). Dr. McConnell is with the San Francisco Department of Public Health. Dr. Forster is with the psychiatry department of the University of California, San Francisco. Dr. McFarland is with the psychiatry department of the Oregon Health and Science University in Portland.
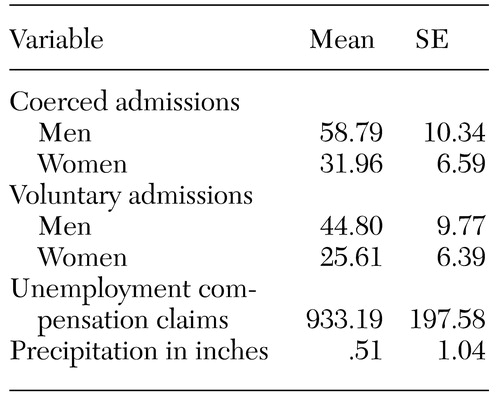 |
Table 1. Means of the 180 weekly values for each continuous variable used in the study for 29,010 admissions to emergency services
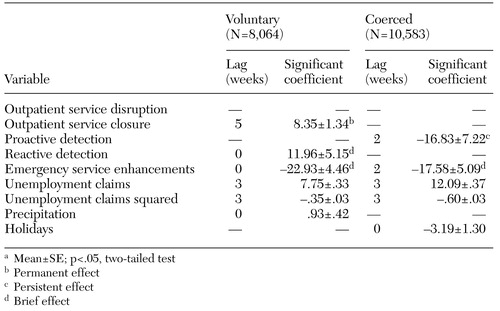 |
Table 2. Significant coefficientsa for models predicting voluntary and coerced emergency admissions of men to an emergency service during a 180-week period
a Mean±SE; p<.05, two-tailed test
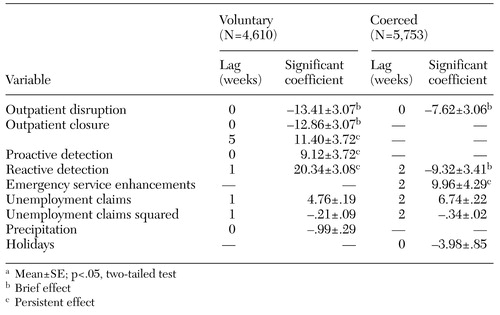 |
Table 3. Significant coefficientsa for models predicting voluntary and coerced emergency admissions of women to an emergency service during a 180-week period
a Mean±SE; p<.05, two-tailed test
1. Allen M (ed): The Growth and Specialization of Emergency Psychiatry. New Directions for Mental Health Services, no 67, 1995Google Scholar
2. Wellin E, Schlesinger D, Hollister C: Psychiatric emergency services: evolution, adaptation, and proliferation. Social Science and Medicine 24:475-482, 1987Crossref, Medline, Google Scholar
3. Forster P: Definitive treatment of patients with serious mental disorders in an emergency service: part 1. Psychiatric Services 45:1177-1178, 1994Link, Google Scholar
4. Bassuk E: The impact of deinstitutionalization on the general hospital psychiatric emergency ward. Psychiatric Services 31:623-627, 1980Link, Google Scholar
5. Elliot R: Patient dumping, COBRA, and the public psychiatric hospital. Psychiatric Services 44:155-158, 1993Link, Google Scholar
6. Hughes D: Trends and treatment models in emergency psychiatry. Psychiatric Services 44:927-928, 1993Link, Google Scholar
7. Surles R, McGurrin M: Increased use of psychiatric emergency services by young chronic mentally ill patients. Psychiatric Services 38:401-405, 1987Link, Google Scholar
8. Oldham J, Lin A, Breslin L: Comprehensive psychiatric emergency services. Psychiatric Quarterly 60:57-60, 1990Crossref, Google Scholar
9. Allen MH: Level I psychiatric emergency services: tools of the crisis sector. Psychiatric Clinics of North America 22:713-734, 1999Crossref, Medline, Google Scholar
10. Fisher W, Geller J, Wirth-Cauchon J: Empirically assessing the impact of mobile crisis capacity on state hospital admissions. Community Mental Health Journal 26:245-253, 1990Crossref, Medline, Google Scholar
11. Catalano R, Novaco R, McConnell W: A model of the net effect of job loss on violence. Journal of Personality and Social Psychology 72:1440-1447, 1977Crossref, Google Scholar
12. Catalano R, Dooley D, Novaco R, et al: Using the ECA data to examine the effect of job layoff on violent behavior. Psychiatric Services 44:874-878, 1993Link, Google Scholar
13. Catalano R, Dooley D, Wilson G, et al: Job loss and alcohol abuse: a test using data from the Epidemiologic Catchment Area project. Journal of Health and Social Behavior 34:215-226, 1993Crossref, Medline, Google Scholar
14. Catalano R, Novaco R, McConnell W: Layoffs and violence revisited. Aggressive Behavior 28:233-247, 2002Crossref, Google Scholar
15. Carney P, Fitzgerald C, Monaghan C: Influence of climate on the incidence of mania. British Journal of Psychiatry 152:820-823, 1988Crossref, Medline, Google Scholar
16. Shaner A, Echman T, Roberts L, et al: Disability income, cocaine use, and repeated hospitalization among schizophrenic cocaine abusers. New England Journal of Medicine 333:777-784, 1995Crossref, Medline, Google Scholar
17. Catalano R, McConnell W: Psychiatric emergencies: the check effect revisited. Journal of Health and Social Behavior 40:79-86, 1999Crossref, Medline, Google Scholar
18. Catalano R, McConnell W, Forster P, et al: Does the disbursement of income increase psychiatric emergencies involving drugs and alcohol? Health Services Research 35:813-823, 2000Google Scholar
19. Maynard C, Cox G: Association between week of the month and hospitalization for substance abuse. Psychiatric Services 51:31, 2000Link, Google Scholar
20. Miner C, Rosenthal R, Hellerstein D, et al: Prediction of compliance with outpatient referral in patients with schizophrenia and psychoactive substance use disorders. Archives of General Psychiatry 54:706-712, 1997Crossref, Medline, Google Scholar
21. Hamilton J: Time Series Analysis. Princeton, NJ, Princeton University Press, 1994Google Scholar
22. Catalano R, Frank J: Detecting the effect of medical care on mortality. Journal of Clinical Epidemiology 54:830-836, 2001Crossref, Medline, Google Scholar
23. Liu L, Hudak G: Forecasting and Time Series Analysis Using the SCA Statistical System. Oak Brook, Ill, Scientific Computing Associates, 1992Google Scholar
24. Box E, Jenkins G, Reinsel G: Time-Series Analysis: Forecasting and Control. Englewood Cliffs, NJ, Prentice Hall, 1994Google Scholar
25. Tsay R: Outliers, level shifts, and variance changes in time series. Journal of Forecasting 7:1-20, 1988Crossref, Google Scholar
26. Hillmer S: Monitoring and adjusting forecasts in the presence of additive outliers. Journal of Forecasting 3:205-215, 1984Crossref, Google Scholar
27. Brooks M, Sanguineti V, Schwartz S: Providing short-term intensive treatment in public psychiatry. Hospital and Community Psychiatry 43:74-76, 1992Abstract, Google Scholar
28. Catalano R, McConnell W: A test of the quarantine theory of civil commitment. Journal of Health and Social Behavior 37:381-387, 1996Crossref, Medline, Google Scholar
29. Rosenheck R, Lam J, Randolph F: Impact of representative payees on substance use by homeless persons with serious mental illness. Psychiatric Services 48:800-806, 1997Link, Google Scholar
30. Price R, von Ryn M, Vinokur A: Impact of a preventive job search intervention on the likelihood of depression among the unemployed. Journal of Health and Social Behavior 33:158-167, 1992Crossref, Medline, Google Scholar
31. Proudfoot J, Guest D, Carson J, et al: Effect of cognitive-behavioral training on job-finding among long-term unemployed people. Lancet 350:96-100, 1997Crossref, Medline, Google Scholar