A Comparison of the Performance of For-Profit and Nonprofit U.S. Psychiatric Inpatient Care Providers Since 1980
Abstract
OBJECTIVE: The authors synthesized evidence from a systematic review of the literature reporting substantiated performance differences between private for-profit and private nonprofit psychiatric inpatient care providers in the United States since 1980. They also compared reported differences in performance between nonprofit and for-profit inpatient psychiatric care providers with reported differences between nonprofit and for-profit providers of other types of health care. METHODS: Studies were located by means of computerized bibliographic searches and follow-up searches of studies cited in the articles located in the computerized search. The analysis included peer-reviewed studies that compared the performance of for-profit and nonprofit health service providers, including inpatient psychiatric services, in the areas of access, quality, cost-efficiency, and amount of charity care on the basis of quantitative data collected after 1980. The studies were classified in one of three categories according to the study conclusion: for-profit superiority, nonprofit superiority, or no difference or mixed results. RESULTS: Almost all studies (with one exception) found that the nonprofit psychiatric providers performed as well as or better than their for-profit counterparts. The proportion of studies reporting performance superiority of nonprofit versus for-profit psychiatric inpatient providers was greater than the proportion of studies reporting the same conclusion for providers of all other types of health care taken together. CONCLUSIONS: On the basis of data collected since 1980, nonprofit psychiatric inpatient care providers in the United States had superior performance on access, quality, cost-efficiency, and amount of charity care, compared with for-profit providers. Caution is warranted in pursuing public policies that permit or encourage the replacement of nonprofit psychiatric inpatient care providers with for-profit providers of these services.
Historically, psychiatric facilities in the United States were largely a charitable activity (1). But this pattern changed in the last half of the 20th century, as the entire U.S. health system moved toward for-profit provision of health care (2,3). The question of the relative role of for-profit and nonprofit providers in psychiatric inpatient care is quite controversial, driven as much by market concerns as by ideology or evidence of outcomes (4,5,6,7). Some authors have argued that market efficiency and competition favor expanding the role of the private for-profit sector (8,9,10,11,12,13,14,15,16,17). Equally convincing points, such as achieving lower costs and better quality, have been made in favor of the provision of nonprofit care (14,18,19,20,21).
Although lower overall discretionary public spending is likely in the future, public policy makers should consider the research evidence on the performance differences between for-profit and nonprofit psychiatric health care providers before reducing subsidies or rates of reimbursement. Many private-sector benefits managers require performance ratings of the providers from whom they purchase health services (22,23). This article presents a systematic review of the evidence on the comparative performance of for-profit and nonprofit inpatient psychiatric health care providers. In addition, it examines how the performance of for-profit and nonprofit providers in the psychiatric inpatient sector compares with that of providers in other health care sectors and considers the proportion of health care performance studies that is dedicated to inpatient mental health care.
Methods
Two approaches were used to obtain an exhaustive list of studies comparing for-profit and nonprofit providers across the health care sector. First, a computerized bibliographic search of databases and published indexes and abstracts was undertaken. Searches of MEDLINE (Ovid and PubMed versions), Web of Science (Social Sciences Citation Index and Science Citation Index), ABI/INFORM, and Sociological Abstracts were conducted. The following indexing terms were used to retrieve English-language-only articles restricted to human subjects: for-profit, nonprofit, not-for-profit, ownership, health services, investor status, quality, cost, charity, access, psychiatric facilities, health providers, psychiatric hospitals, dialysis centers, health maintenance organizations (HMOs), hospitals, home health care, and nursing homes. The online literature search yielded 1,428 published articles, which were then closely screened and coded. Second, the bibliographies and reference lists of these articles were searched for additional articles.
Three inclusion criteria were used to screen the published articles. First, the analysis of the original empirical data comparing for-profit and not-for-profit health care providers had to include one or more of the following four performance variables of interest: access, quality, cost-efficiency, and amount of charity care. Second, the majority of data collection had to be completed after January 1, 1980. Third, the study had to be published in a peer-reviewed journal. The peer-review status of the journals was determined from the journal's listing in Ulrich's Periodical Directory (24).
All studies in the inventory were given equal weight for purposes of this analysis. Because the inventory was comprehensive, sample-based tests of statistical significance were not relevant. Such tests are useful principally when the intent is to draw inferences about the unknown characteristics of a population from a sample with specific, known characteristics. The intent in this study was, rather, to inventory the full universe of studies and characterize the population that met the inclusion criteria without selecting a representative sample.
Unlike a quantitative meta-analysis, the analysis reported here did not aggregate statistical results across studies, because few are commensurable. We attended principally to statements of findings about relative performance and relied on the peer-review process to ensure each study's validity. The authors' conclusions about the relative performance of for-profit and nonprofit providers were coded as findings favoring the superiority of for-profit providers, findings favoring the superiority of nonprofit providers, or as mixed and inconclusive findings that showed no clear superiority between the two types of providers.
In coding the authors' conclusions, we assumed that superior performance was represented by lower costs or better cost-efficiency rather than by higher costs or lower efficiency and by higher quality rather than lower quality. Greater access to health care was considered to be better than less access (25). More charity care was assumed to be preferred to less and to represent higher performance. How these performance variables were defined and operationalized across the studies is discussed below.
Results
A total of 149 peer-reviewed journal articles qualified for inclusion in our final population of studies assessing the relative performance of for-profit and nonprofit providers across all health care provider types. Seventeen of the 149 articles assessed the performance of psychiatric care providers, and they are specifically cited in this article; a complete list of the 149 articles is available from the first author.
The 149 articles reported a total of 179 performance assessments over the past 22 years. Thirty examined access, 56 considered cost, 69 looked at quality, and 24 studied the amount of charity care provided. Eleven percent of these studies (17 studies) compared the relative performance of inpatient psychiatric care providers, offering a total of 23 comparative performance assessments (26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42) (see Table 1). Twelve compared for-profit and nonprofit psychiatric inpatient care providers on access, five examined cost, four looked at quality differences, and two compared the amount of charity care provided.
In the articles that were inventoried, the term "inpatient psychiatric care" was found to refer to a range of providers, including mental health care hospitals, freestanding psychiatric inpatient facilities, psychiatric specialty hospitals, mental health care facilities, and general hospital units specializing in acute inpatient psychiatric care. The studies that assessed inpatient mental health care providers examined performance in a variety of geographical locations. Thirteen studies were national. One study included data from 32 primarily eastern states. Three were single-state studies with California as the focus. A few studies considered special populations, for example, children, adolescents, or elderly patients.
Performance was defined and measured in several ways. Cost or efficiency referred to expenses per patient, cost per patient day, cost per case, net patient revenues, mark-up, or profitability. Measures of high-quality performance included lower adverse event rates, lower mortality rates, lower disenrollment rates, the presence of programs offering a full continuum of health care, more patient education, or a higher Health Plan Employer Data and Information Set (HEDIS) score from the National Committee for Quality Assurance. In the subset of studies that focused on psychiatric inpatient care, higher quality was reported as a lower noncompliance notification rate, a broader array of services, fewer inappropriately short stays, and lower rehospitalization rates.
Access to health care for both mental health care providers and all other provider types was typically defined as whether the provider took on a fair share of Medicaid and Medicare patients and other expensive-to-treat patients and whether the provider offered costly treatments, such as unprofitable emergency room care. Most studies considered charity care to be any treatment of bad-debt patients or provision of unpaid services or uncompensated care.
The amount of research comparing the performance of for-profit and nonprofit psychiatric inpatient health care providers increased across the past two decades. Data collection was at a peak in the late 1980s, when eight research projects whose findings were later published in peer-reviewed journals were concluded. As for actual publication dates, however, 15 articles were published on this topic since 1990, and only two were published in the 1980s. The mean time interval between data collection and publication was 5.88 years for articles comparing for-profit and nonprofit psychiatric inpatient care providers, slightly greater than the mean time of 4.74 years for all other types of providers.
The major—and unexpected—finding of this synthesis of studies was the performance superiority of the nonprofit psychiatric inpatient care providers compared with the for-profit providers (Table 2). Sixteen of the 17 studies (96 percent) found that the performance of the nonprofit psychiatric inpatient care providers was better than or equal to that of their for-profit counterparts across all four performance criteria. The nonprofit care providers were found to have performed best in 70 percent of the comparisons. Twenty-six percent of the comparisons indicated no difference between the for-profit and nonprofit providers.
For all other health care provider types—hospitals, nursing homes, HMOs, home health care organizations, and dialysis centers—the results were much the same, although less pronounced, than for the psychiatric inpatient care providers. Most of the 132 studies failed to demonstrate that for-profit providers maintained a level of performance equal to or better than the nonprofit providers (Table 2).
Discussion
The number of for-profit psychiatric inpatient providers appears to have declined substantially in recent years (43), and the lower-than-expected level of performance of these providers found in this synthesis of studies may provide an explanation. Although about half of inpatient mental health care providers in 1997 were for-profit entities, that proportion declined to about one-third by 1999 (3,44,45). Besides providers that were affected by performance issues, some for-profit enterprises may have simply concluded that the financial payoff was too low to warrant further investment. Some for-profit providers were also subject to criminal investigation because of fraud charges in the 1990s, and the bad publicity did not help the bottom line (46). Patient lawsuits, oversupply, and capitation fee structures similarly reduced profit margins (43).
Economists typically expect the cost performance of for-profit providers to be superior to that of nonprofit providers, and the hope is that for-profit providers can maintain quality while also being cost-effective (47). On the other hand, one early study was a forewarning that this expectation was unrealistic; it reported that for-profit outpatient clinics were "highly motivated by commercial concerns" and billed more per patient than nonprofit clinics (48). However, the path to quality improvement in psychiatric inpatient care, while known, is expensive. Some examples illustrate this point. Case management has been found to improve outcomes (49), as has follow-up care after an initial inpatient mental health episode (50). Both may add to costs and reduce profit margins. Higher-quality psychiatric inpatient care includes reducing the use of restraints, but often the trade-off is that staffing must be increased or video monitoring equipment installed to ensure safety (51). Several studies in this inventory suggested that reducing costs may also reduce quality, something unanticipated and left undiscussed by formal economic models.
Management experts have hypothesized that nonprofit organizations in general may be better at "the motivation and productivity of knowledge workers" than private for-profit businesses (52). Psychiatric inpatient care may be an important example of this type of knowledge-based enterprise. Private nonprofit organizations have long been known to produce public goods of great value to society. They save taxpayers scarce resources by caring for poor patients who might otherwise be cared for only at public inpatient facilities (53). Authorities in the business field have considered nonprofit managers to be especially creative and innovative (54). A 2000 Wall Street Journal article (55) presented the opinion that "people who run charities and other nonprofits have a long history of managing under uncertain conditions, satisfying multiple stakeholders, building passionate work forces and developing non-financial measurements of goals—the kind of issues that are becoming hot topics in corporate management." Our research supports these views.
Our study had several limitations that should be noted. Perhaps the most serious limitation is our acceptance of the authors' judgment of relative performance in each of the studies we reviewed. Some authors may have exaggerated or overgeneralized their empirical findings. Of course, unless such a bias is slanted toward one type of provider, this kind of error would not dramatically alter our results. If the recent political climate creates any bias, it would tend to support a presumption against the superiority of nonprofit provision of care. In addition, conclusions from the available research cannot be taken as indicative of national trends. Several of the studies drew on state-level rather than provider-level data; others were case studies. Finally, the results reflect only published studies from the last 22 years and do not support extrapolation to the future.
Conclusions
This article summarized the results of studies that compared the performance of for-profit and nonprofit psychiatric inpatient care providers in the United States on the basis of data collected since 1980. On the whole, the data did not reveal any special performance advantage in the for-profit provision of inpatient psychiatric care. The proportion of studies that reported superior performance of nonprofit providers was greater for psychiatric inpatient mental health providers than for all other health care providers. The review found little evidence that for-profit inpatient health care in general has achieved superiority on any of the four basic performance variables considered. The overwhelming majority of the studies undermine a performance rationale for public policy decisions to expand for-profit inpatient health care.
Acknowledgments
The authors thank Jennifer Bennett, B.A., and Malorie Gist, J.D., for help in searching the databases, managing the archives of articles, and preparing the manuscript. This research was supported by the Center for Society and Population Health, School of Public Health, University Texas-Houston Health Science Center.
Dr. Rosenau is professor and Dr. Linder is associate professor in the department of management and policy sciences in the School of Public Health of the University of Texas-Houston Health Science Center, 1200 Herman Pressler Drive, P.O. Box 20186, Houston, Texas 77225 (e-mail, [email protected]).
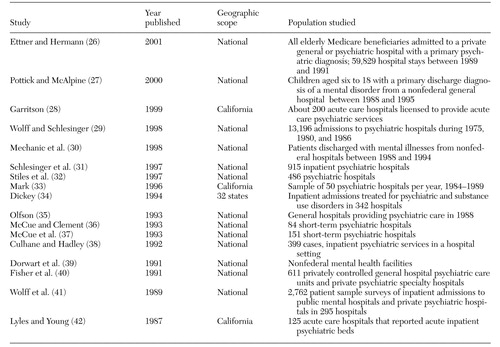 |
Table 1. Peer-reviewed studies based on data collected since 1980 comparing the relative performance of for-profit and nonprofit inpatient psychiatric health care providers in the United States
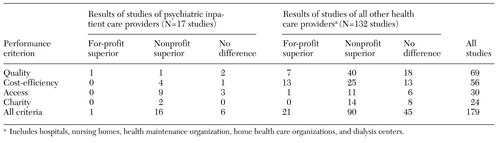 |
Table 2. Results of studies based on data collected since 1980 comparing the relative performance of for-profit and nonprofit health care providers in the United States, by number of studies reporting the indicated result
1. Starr P: The Social Transformation of American Medicine. New York, Basic Books, 1982Google Scholar
2. Goodrick E, Meindl JR, Flood AB: Business as usual: the adoption of managerial ideology by U.S. hospitals. Research in the Sociology of Health Care 14:27-50, 1997Google Scholar
3. US Census Bureau:1997 Economic Census: Health Care and Social Assistance. Washington, DC, US Department of Commerce, 1999Google Scholar
4. Martin DV: Institutionalization. Lancet 2:1188-1190, 1955Crossref, Google Scholar
5. Mendel WM, Green GA: Aftercare. New York, Basic Books, 1967Google Scholar
6. Gordon HL, Groth C: Mental patients wanting to stay in the hospital. Archives of General Psychiatry 4:124-130, 1961Crossref, Medline, Google Scholar
7. Wirt GL: Institutionalism revisited: prevalence of the institutionalized person. Psychiatric Rehabilitation Journal 22:302-304, 1999Crossref, Google Scholar
8. Jaspen B: Entrpreneur's dream: healthcare venture capital funding keeps record pace. Modern Healthcare 28(10):40, 1998Google Scholar
9. Robinson JC: Capital finance and ownership conversion in health care. Health Affairs 19(1):56-71, 2000Google Scholar
10. Clark R: Does the nonprofit form fit the hospital industry? Harvard Law Review 93:1417-1489, 1980Google Scholar
11. Cutler DM, Horwitz JR: Converting hospitals from not-for-profit to for-profit status: why and what effects? in The Changing Hospital Industry: Comparing Not-For-Profit and For-Profit Institutions. Edited by Cutler DM. Chicago, University of Chicago Press, 2000Google Scholar
12. Hassan MM: Let's end the nonprofit charade. New England Journal of Medicine 334:1055-1057, 1996Crossref, Medline, Google Scholar
13. Wilder T: Non-Profit Conversions: Conversion of Not-For-Profit Hospitals to For-Profit Status Stirs up Concerns. Health Care Policy Report 4(34). Washington, DC, Bureau of National Affairs, 1996Google Scholar
14. Gray BH: Why nonprofits? Hospitals and the future of American health care. Frontiers of Health Services Management 8:3-32, 1991Medline, Google Scholar
15. Jensen MC, Ruback RS: The market for corporate control. Journal of Financial Economics 11:5-50, 1983Crossref, Google Scholar
16. Manne H: Mergers and the market for corporate control. Journal of Political Economy 73:110-120, 1965Crossref, Google Scholar
17. Kuttner R: Must good HMOs go bad? Part one. New England Journal of Medicine 338:1558-1639, 1998Crossref, Medline, Google Scholar
18. Woolhandler S, Himmelstein DU: Costs of care and administration at for-profit and other hospitals in the United States. New England Journal of Medicine 336:769-774, 1997Crossref, Medline, Google Scholar
19. Reinhardt UE: The economics of for-profit and not-for-profit hospitals. Health Affairs 19(6):178-186, 2000Google Scholar
20. Lawrence D: Why we want to remain a nonprofit health care organization. Health Affairs 16(2):121-124, 1997Google Scholar
21. Lawrence DM, Mattingly PH, Ludden JM: Trusting in the future: the distinct advantage of nonprofit HMOs. Milbank Quarterly 75:5-10, 1997Crossref, Medline, Google Scholar
22. Winslow R: Making the grade: improvements in quality of care suggest hospitals are taking report cards to heart. Wall Street Journal, Oct 19, 1998, pp R16,R18Google Scholar
23. Burton TM: HMO rates hospitals: many don't like it, but they get better. Wall Street Journal, April 22, 1999, pp A1, A13Google Scholar
24. RR Bowker/Ulrich's Periodicals Directory, 2001. Available at www.ulrichsweb.com/ulrichsweb/Google Scholar
25. Daniels N, Light DW, Caplan RL: Benchmarks of Fairness for Health Care Reform. New York, Oxford University Press, 1996Google Scholar
26. Ettner SL, Hermann RC: The role of profit status under imperfect information: evidence from the treatment patterns of elderly medicare beneficiaries hospitalized for psychiatric diagnoses. Journal of Health Economics 20:23-49, 2001Crossref, Medline, Google Scholar
27. Pottick KJ, McAlpine DD: Changing patterns of psychiatric inpatient care for children and adolescents in general hospitals, 1988-1995. American Journal of Psychiatry 157:1267-1274, 2000Link, Google Scholar
28. Garritson SH: Availability and performance of psychiatric acute care facilities in California from 1992 to 1996. Psychiatric Services 50:1453-1460, 1999Link, Google Scholar
29. Wolff N, Schlesinger M: Access, hospital ownership, and competition between for-profit and nonprofit institutions. Nonprofit and Voluntary Sector Quarterly 27:203-236, 1998Crossref, Google Scholar
30. Mechanic D, McAlpine DD, Olfson M: Changing patterns of psychiatric inpatient care in the United States, 1988-1994. Archives of General Psychiatry 55:785-791, 1998Crossref, Medline, Google Scholar
31. Schlesinger M, Dorwart R, Hoover C, et al: Competition ownership, and access to hospital services: evidence from psychiatric hospitals. Medical Care 35:974-992, 1997Crossref, Medline, Google Scholar
32. Stiles PG, Culhane DP, Hadley TR: For-profit versus non-profit freestanding psychiatric inpatient facilities: an update. Administration and Policy in Mental Health 24:191-204, 1997Crossref, Medline, Google Scholar
33. Mark TL: Psychiatric hospital ownership and performance: do nonprofit organizations offer advantages in markets characterized by asymmetric information? Journal of Human Resources 31:631-649, 1996Google Scholar
34. Dickey B: A comparison of for-profit and not-for-profit hospitals on the cost of mental health admissions. Harvard Review of Psychiatry 2:97-103, 1994Crossref, Medline, Google Scholar
35. Olfson M: The array of psychiatric services in general hospitals. General Hospital Psychiatry, 15:277-283, 1993Crossref, Medline, Google Scholar
36. McCue MJ, Clement JP: Relative performance of for-profit psychiatric hospitals in investor-owned systems and nonprofit psychiatric hospitals. American Journal of Psychiatry, 150:77-82, 1993Link, Google Scholar
37. McCue MJ, Clement JP, Hoerger TJ: The association of ownership and system affiliation with the financial performance of inpatient psychiatric hospitals. Inquiry 30:306-317, 1993Medline, Google Scholar
38. Culhane DP, Hadley TR: The discriminating characteristics of for-profit versus not-for-profit freestanding psychiatric inpatient facilities. Health Services Research, 27:177-194, 1992Medline, Google Scholar
39. Dorwart RA, Schlesinger M, Davidson H, et al: A national study of psychiatric hospital care. American Journal of Psychiatry 148:204-210, 1991Abstract, Google Scholar
40. Fisher WH, Dorwart RA, Schlesinger M, et al: Contracting between public agencies and private psychiatric inpatient facilities. Medical Care 29:766-774, 1991Crossref, Medline, Google Scholar
41. Wolff N, Henderson PR, MacAskill RL, et al: Treatment patterns for schizophrenia in psychiatric hospitals. Social Science and Medicine, 28:323-331, 1989Crossref, Medline, Google Scholar
42. Lyles CA, Young JP: Hospital ownership and psychiatric services. Journal of Medical Systems 11:45-57, 1987Crossref, Medline, Google Scholar
43. Gimmy AE, Baumbach CR: Psychiatric hospitals. Appraisal Journal 69:52-67, 2001Google Scholar
44. Woolhandler S, Himmelstein DU: The National Health Program Slideshow Guide. Chicago, Physicians for a National Health Program, 2000Google Scholar
45. Universal to acquire 11 charter facilities through auction. Alcoholism & Drug Abuse Weekly 12(23):1-3, 2000Google Scholar
46. Saphir A: Psychiatric sector sees slight changes. Modern Healthcare 29(21):44-45, 1999Google Scholar
47. Flower J: Is the war between investor-owned institutions and not-for-profits over? Healthcare Forum Journal 40:59-64, 1997Google Scholar
48. Hall S, McGuire TG: Ownership and performance: the case of outpatient mental health clinics. Medical Care 25:1179-1183, 1987Crossref, Medline, Google Scholar
49. Ziguras SJ, Stuart GW: A meta-analysis of the effectiveness of mental health case management over 20 years. Psychiatric Services 51:1410-1421, 2000Link, Google Scholar
50. Huff ED: Outpatient utilization patterns and quality outcomes after first acute episode of mental health hospitalization. Evaluation and the Health Professions 23:441-456, 2000Crossref, Medline, Google Scholar
51. Two efforts to reduce restraint use win national awards. Mental Health Weekly 10 (40):1-4, 2000Google Scholar
52. Drucker PF: What business can learn from nonprofits. Harvard Business Review 67:88-93, 1989Medline, Google Scholar
53. Lowry RC: Nonprofit organizations and public policy. Policy Studies Review 14:107-114, 1995Crossref, Google Scholar
54. Nelson SJ: What can managers learn from nonprofits? Harvard Management Update 4:3-4, 1999Google Scholar
55. Nonprofit managers. Wall Street Journal, Jan 6, 2000, p 1Google Scholar



