Gender Differences in Characteristics and Service Use of Public Mental Health Patients With Schizophrenia
Abstract
The study examined gender differences in sociodemographic, clinical, and mental health service use variables among patients with schizophrenia in a public mental health care system. Data from 1999 to 2000 for 4,975 adult patients were analyzed. Women were older and more likely to be married and to have Medicaid insurance and less likely to have a diagnosis of substance abuse than men. More women were living independently, whereas more men resided in assisted living facilities or were homeless. Women were significantly more likely to have had a psychiatric hospitalization than men, which may be related to differential use of services by men and women with the worst level of functioning.
It has been well documented that women with schizophrenia have less severe illness than their male counterparts (1,2). However, gender differences in the use of mental health services among persons with schizophrenia have been less well studied. Some investigations have shown no significant gender differences in the use of outpatient or inpatient mental health services among patients with severe mental illness (3,4), whereas one study showed that women with schizophrenia were more likely to use outpatient services than men (5). To our knowledge, gender differences in the use of other specific types of mental health treatment have not been reported among patients with schizophrenia.
The purpose of this study was to examine gender differences in sociodemographic and clinical characteristics and mental health service use among patients with schizophrenia in a public mental health system.
Methods
This was a retrospective analysis of management information system (MIS) data from the San Diego County Mental Health System, a public mental health system that either provides services directly or contracts with independent mental health care providers. Data originating from files covering multiple episodes of care were aggregated at the client level into a single data file that included sociodemographic and clinical measures as well as service use records for fiscal year 1999 to 2000. Use of these data was approved by the local institutional review board, and client confidentiality was maintained.
The study sample consisted of all patients aged 18 years or older who had used mental health services during the fiscal year at least once for a DSM-IV diagnosis of schizophrenia, schizoaffective disorder, or schizophreniform disorder. A hierarchical algorithm was used to determine diagnosis such that the diagnosis of schizophrenia in any setting precluded other diagnoses given during other episodes of care. Data for 4,975 of 6,872 patients were analyzed. Of the patients excluded, 450 had missing data on one or more sociodemographic variables; 1,447 patients resided in justice-related, institutional, or other or unknown settings in which mental health services were provided by systems other than the county mental health system.
Age was categorized as 18 to 44 years or 45 years and older. Ethnicity was categorized as Caucasian, African American, Latino, or other. Living situation was recorded as the most frequently occurring (the mode) among four categories: independent, with family or others, assisted living, and homeless. Insurance coverage (Medi-Cal—that is, California's Medicaid), employment, marital status, and education were coded as dichotomous variables.
Severity of illness and level of functioning were measured in terms of conservatorship status—that is, court-determined incompetence to make medical or legal decisions, measured as a dichotomous variable (by definition, patients with conservatorship are gravely ill); substance abuse, categorized as the presence or absence of any substance related diagnosis in any care setting during the fiscal year (concomitant substance abuse has been shown to increase the likelihood of mental health service use among homeless persons with psychiatric disorders [6]); and level of functioning, assessed with the Global Assessment of Functioning (GAF) scale of DSM-IV. Using the admission GAF score averaged across all episodes of care for each individual, we divided the GAF scores into tertiles: low (less than 30), middle (30 to 39), and high (40 to 99).
Mental health services were categorized as emergency psychiatric care, inpatient psychiatric hospital, crisis residential, outpatient, day treatment and rehabilitation, and case management. Service use was defined as the presence or absence of at least one billable encounter in a service category for the fiscal year. Emergency psychiatric treatment included only service in the county-operated psychiatric emergency unit. Inpatient psychiatric hospitalization included admission to any fee-for-service, county-contracted, or county-operated psychiatric hospital. Crisis residential treatment included admission to a residential program that provided short-term, acute residential treatment services as an alternative to voluntary hospitalization. Outpatient treatment consisted of a variety of individual and group services provided at county clinics and by county-contracted providers. Day treatment was defined as receipt of services in a day rehabilitation, day treatment, or partial hospitalization program. Case management included a variety of services to assist patients in obtaining access to mental health, medical, and other services.
Chi square tests were conducted for categorical variables. For the mental health services for which significant gender differences were found, we performed multiple logistic regression to assess factors that were associated with the likelihood of service use by gender, controlling for the other variables.
Results
Compared with the study sample, the patients excluded from the analysis were significantly more likely to be men, unmarried, unemployed, and uninsured and less likely to have graduated from high school, to have a diagnosis of substance abuse, to have a public conservator, or to be in the group of higher-functioning patients.
No significant gender differences were observed in ethnicity, employment status, education, or conservatorship status, as can be seen from Table 1. Women were older than men and more likely to be married and to have Medi-Cal insurance. More women were living independently, whereas more men resided in assisted living facilities or were homeless. More men than women had a concurrent diagnosis of substance abuse. The low- and high-functioning groups contained more women, whereas more men were categorized in the middle group.
No significant gender differences were noted in the use of day treatment, rehabilitation, or case management services. However, men were more likely to use crisis residential and emergency services, and women were more likely to use inpatient and outpatient services. However, when sociodemographic and clinical variables were controlled for, only the gender difference in the use of inpatient services was significant: women were 51 percent as likely as men to be hospitalized (95 percent confidence interval=1.24 to 1.84, p<.001).
Discussion and conclusions
The gender differences in sociodemographic and clinical variables we observed in this sample of patients with schizophrenia who were enrolled in a publicly funded mental health system were similar to those reported in other studies of patients with schizophrenia (1,2,7). These differences in sociodemographic and clinical variables seemed to account for most of the gender differences observed in mental health service use, because men and women were equally likely to use crisis residential, emergency psychiatric, and outpatient services when these factors were controlled for.
The lack of gender differences in the use of outpatient mental health services is consistent with some studies (3,4), but not all (5), that have examined outpatient service use among patients with schizophrenia. The increased likelihood of inpatient hospitalization found in this study, which differs from results reported by McAlpine and Mechanic (4), may have been associated with gender differences in the interaction among severity of illness and residential and treatment settings. We excluded persons who resided in justice and institutional facilities, who were more likely to be men and lower functioning. Lower-functioning women may be more likely to receive care in a public mental health system and to require hospitalization.
This study had several limitations. Data on the use of emergency services were restricted to those from the county-run emergency clinic; data on services received in the emergency departments of private-sector hospitals were not available. Persons who resided in a justice-related, institutional, or other or unknown setting were excluded. Nonetheless, these results suggest that some of the gender differences in the use of mental health services among patients with schizophrenia receiving care from a publicly funded health care system may have been due to gender differences in other sociodemographic and clinical variables, whereas some of these may have been related to gender differences in the interaction among severity of illness and residential and treatment settings.
Dr. Lindamer, Ms. Bailey, Dr. Hawthorne, Dr. Hough, and Dr. Jeste are affiliated with the department of psychiatry at the University of California, San Diego. Dr. Lindamer is also with Veterans Integrated Service Network (VISN) 22 in San Diego, Dr. Hawthorne is also with the Community Research Foundation in San Diego, and Dr. Hough is also with the department of sociology of San Diego State University. Dr. Folsom and Dr. Gilmer are with the department of family and preventive medicine of the University of California, La Jolla; Dr. Folsom is also with VISN 22 in San Diego. Dr. Garcia is with the San Diego County Mental Health System. Send correspondence to Dr. Lindamer at VA San Diego Healthcare System, 116A, 3350 La Jolla Village Drive, San Diego, California 92161 (e-mail, [email protected]).
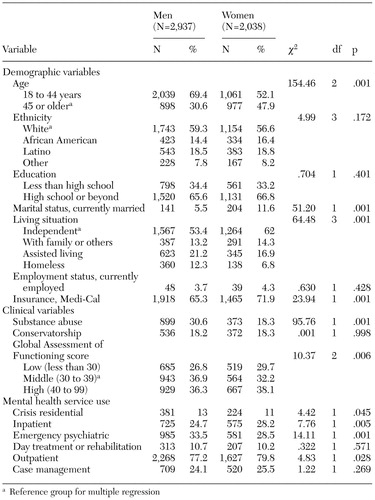 |
Table 1. Gender differences in demographic, clinical, and service use variables among patients with schizophrenia in a public mental health system
1. Tamminga CA: Gender and schizophrenia. Journal of Clinical Psychiatry 58(suppl 15):33–37, 1997Medline, Google Scholar
2. Lindamer LA, Harris MJ, Gladsjo JA, et al: Gender and schizophrenia, in Sex Hormones, Aging, and Mental Disorders. Edited by Morrison M. Washington, DC, National Institute of Mental Health, 2000Google Scholar
3. Yanos PT: Proactive coping among persons diagnosed with severe mental illness: an exploratory study. Journal of Nervous and Mental Disease 189:121–123, 2001Crossref, Medline, Google Scholar
4. McAlpine D, Mechanic D: Utilization of specialty mental health care among persons with severe mental illness: the roles of demographics, need, insurance, and risk. Health Services Research 35:277–292, 2000Medline, Google Scholar
5. Dixon L, Lyles A, Smith C, et al: Use and costs of ambulatory care services among Medicare enrollees with schizophrenia. Psychiatric Services 52:786–792, 2001Link, Google Scholar
6. Wu L, Kouzis A, Leaf P: Influence of comorbid alcohol and psychiatric disorders on utilization of mental health services in the National Comorbidity Survey. American Journal of Psychiatry 156:1230–1236, 1999Abstract, Google Scholar
7. Lindamer LA, Lohr JB, Harris MJ, et al: Gender-related clinical differences in older patients with schizophrenia. Journal of Clinical Psychiatry 60:61–67, 1999Crossref, Medline, Google Scholar