Use and Costs of Ambulatory Care Services Among Medicare Enrollees With Schizophrenia
Abstract
OBJECTIVE: The objective of this study was to identify predictors of the use and cost of ambulatory care services among Medicare recipients with schizophrenia. METHODS: The design was a cross-sectional analysis of Medicare claims in 1991. The study subjects were a 5 percent random sample of all persons in the United States who had at least one Medicare service claim in 1991 and who were diagnosed as having schizophrenia in any care setting. Outcome measures included use and cost of any ambulatory care service, individual therapy, psychiatric somatotherapy, group therapy, or family therapy. RESULTS: For nearly 25 percent of the total sample of 12,440, no claims were filed for ambulatory care services in 1991. The mean±SD number of ambulatory care visits during the year was 7.9±21. The most frequently used type of therapy was individual therapy (5±14 visits). The mean±SD yearly cost of care for persons who received ambulatory care services was $470±$1,028. Among persons under 65 years of age, Caucasians were about 1.5 times as likely as African Americans to have received an ambulatory care service and 1.3 times as likely to have received individual therapy. Persons who were 65 or older were less likely to have received any service. Among service recipients, costs of care were lower for African Americans and for older people. CONCLUSIONS: The use of Medicare-funded ambulatory care services by persons with schizophrenia varied by race and age. Further investigation is required to determine whether subgroups of individuals who do not have additional insurance coverage or access to services are receiving substandard care.
In the United States, schizophrenia affects about 1 percent of the population and costs the nation $30 billion to $40 billion annually (1). Schizophrenia accounts for 25 percent of all hospital bed days, 40 percent of all long-term-care days, and 20 percent of all Social Security benefit days (2). The vast majority of patients who have schizophrenia receive their mental health care through benefits provided by Medicaid, Medicare, or the Department of Veterans Affairs. These payment mechanisms yield large databases that can provide information to support public policy that is intended to improve the care of patients with schizophrenia.
Patients with schizophrenia accounted for 10 to 15 percent of all claimants for a mental health or substance abuse service under Medicaid in 1993 and Medicare in 1994 (3). Such macro-level statistics underscore schizophrenia's impact on the nation's health and on its government-funded health care services. However, to understand the quality and efficiency of care provided to persons with schizophrenia under these programs, it is necessary to extend analyses to the level of the individual.
Patient analyses based on medical service claims can fill the gaps between macroanalyses and detailed patient studies. A study of Medicaid recipients with schizophrenia in the state of Georgia showed that each claimant generated 3.4 medical claims per month at an average monthly cost of $425 (4). The Schizophrenia Patient Outcomes Research Team (PORT) also analyzed the Medicaid claims history of patients with schizophrenia in 1991 in Georgia. The analysis suggested an overreliance on individual therapy as the primary outpatient treatment for schizophrenia compared with PORT treatment recommendations (5,6,7). Claims-based analyses based on national data are needed to extend the generalizability of these single-state studies.
Our study used national Medicare claims data from the PORT study to assess the use of ambulatory care services by persons with schizophrenia and to link the use of services with hypotheses about quality of care for different types of services and for different subpopulations. Medicare is a federal health insurance program and the primary insurer of people aged 65 years and older—and their spouses—who have been employed for at least ten years in positions paying taxes under the Federal Insurance Contributions Act. It also provides coverage for persons with end-stage renal disease and for persons under 65 years of age who have been receiving disability benefits for at least two years (8). The proportion of Medicare beneficiaries who qualify for Medicare coverage because of disability has been on the rise, increasing from 9.7 percent in 1991 to 13.3 percent in 1999 (9); the economic status of these recipients is largely unknown (10).
For a chronic, debilitating illness such as schizophrenia, underutilization of ambulatory care services increases the risk of crisis-oriented care. Hence we focused our research on the ambulatory component of care. We identified important demographic and clinical factors associated with the use and cost of various ambulatory care services, including individual, group, and family therapy, because all these services have implications for the quality of care delivered to persons who have schizophrenia.
Methods
Sample
The study population consisted of all Medicare enrollees who had at least one service claim in 1991 and who were diagnosed as having schizophrenia or schizoaffective or schizophreniform disorder, according to ICD-9-CM, in any care setting. The Health Care Financing Administration identified 402,954 such enrollees from a national Medicare enrollment of 34.9 million in 1991—about 1.2 percent of total enrollment. If we assume that the number of persons with schizophrenia in the United States is about three million—based on a prevalence of 1 percent—Medicare covers approximately 13 percent of the total number of persons with schizophrenia. Our study population was further limited to individuals aged 18 years or older who were United States residents, had part A and part B coverage during all of 1991, and survived through the end of 1991 (11).
From the final eligible study population of 331,617 enrollees, a 5 percent random sample yielded 16,480 claimants (11). To correct for the potential misclassification of persons who did not have schizophrenia, an algorithm was developed that excluded individuals who did not have a schizophrenia diagnosis for at least one of the following: an inpatient hospital or physician claim, a clinic or office visit claim, or a claim for a physician visit in a skilled nursing or custodial care facility. These exclusion criteria resulted in a sample of 14,182 Medicare enrollees with schizophrenia who used services during 1991. Finally, because PORT data and other data have suggested differences between Caucasian and African American persons in what treatments are recommended and in hospitalization for psychiatric services (6,12), we included only these two groups, for a final sample of 12,440.
Measures
The use of ambulatory care services and total mental health expenditures were identified through service codes from the fourth edition of the Physicians' Current Procedural Terminology (13) that were assigned to individual claims. Four types of ambulatory care services were investigated: individual therapy, group therapy, family therapy, and psychiatric somatotherapy. For the purposes of this study, individual therapy (codes 90842, 90843, and 90844) refers to individual medical psychotherapy by a physician, including insight-oriented, behavior-modifying, and supportive psychotherapy. Group therapy (code 90853) refers to group medical psychotherapy, other than that with multiple family groups, by a physician. Family therapy (codes 90846, 90847, and 90849) is defined as family medical psychotherapy, with or without the patient present, by a physician. Finally, psychiatric somatotherapy (code 90862) refers to pharmacologic management with minimal psychotherapy.
An additional variable was created to identify persons who used any ambulatory care service during the year. Visits and costs were calculated from total service use and expenditures for all ambulatory care mental health visits in 1991 and were not limited to visits for which the reason was a specific diagnosis of schizophrenia.
Data for the demographic variables—sex, age, race, Medicaid coverage, and geographic region—were obtained directly from the Medicare files. Age was dichotomized into less than 65 years and 65 years or older to create a proxy for the distinction between persons who qualified for coverage on the basis of disability and those who qualified on the basis of age. The identification of persons with Medicaid coverage was based on eligibility data for state buy-in. The residence of each patient was assigned to one of nine regions created by the U.S. Bureau of the Census: New England, mid-Atlantic, east north central, west north central, south Atlantic, east south central, west south central, mountain, and Pacific.
From the residence data, eight indicator variables were created; New England was used as the reference region. Four important clinical variables that we hypothesized a priori to be associated with greater use of mental health services were identified from ICD-9 codes on inpatient or outpatient claims. The first three variables were the presence or absence of alcohol abuse (codes 291, 303, and 305.0), drug abuse (codes 292, 304, and 305 excluding 305.0), and a suicide attempt (codes E950-959) and were expressed as dichotomous variables. The fourth variable was the number of comorbid psychiatric illnesses, based on the occurrence of a primary or secondary ICD-9 diagnosis, and was expressed as a continuous variable.
Data analyses
Distributions of the demographic and clinical characteristics of the total sample were examined and then stratified by age and Medicaid enrollment status to informally assess anticipated differences among subgroups. The prevalence of use, mean number of ambulatory care visits, and average cost per person were also computed for each type of service within each subgroup. A series of regression analyses were performed to assess factors associated with the likelihood of service use and to model the costs of care; all demographic and clinical variables that were examined in the descriptive analyses were entered as covariates.
First, using maximum-likelihood estimation, we determined the probabilities of the use of each type of service and use of any service with logistic models. Because we were particularly interested in differences in service use by race as affected by other demographic factors, we tested interaction effects by using product terms of race and each of the other demographic covariates.
The analyses of service costs included only data from persons who had used ambulatory care services. Skewness in the cost data led to the use of a variance-stabilizing logarithmic transformation; log cost for persons in each service category was the dependent variable in the regression analyses. Under these conditions, the data did not violate assumptions for the least-squares regression procedures. All demographic and clinical variables were entered as covariates in models of the log cost for each type of service. In regressions in which log cost was the dependent variable, each geographic region was included to control for regional differences in Medicare reimbursement rates. Hypothesized interactions between race and the remaining covariates were tested in these models; the level of significance was set at .05 or less. Data analyses were performed with use of SAS, version 6.12 (14).
Results
Characteristics of the sample
The study sample of 12,440 persons was predominantly Caucasian and included a slightly higher proportion of men than women—54 percent and 46 percent, respectively—although women were a majority in the group aged 65 years or older (Table 1). The study subjects' mean±SD age was 50.7±16.4 years. The rates of alcohol abuse (5.4 percent) and drug abuse (5 percent) were comparable. Just over half of the sample (54 percent) had Medicaid coverage.
Patterns of ambulatory care service use and costs varied by type of service and across subgroups, as shown in Table 2. For nearly 25 percent of the entire sample, no claim had been filed for an ambulatory care service. The mean±SD number of visits during the year was 7.9±21. The most frequently used type of therapy was individual therapy (5±14 visits), followed by somatotherapy, group therapy, and family therapy. The mean± SD yearly cost of care for those who received an ambulatory care service was $470±$1,045.
Use of ambulatory care services
Type of service received. Being male, being African American, being 65 years of age or older, and having a diagnosis of substance abuse were associated with a lower likelihood of receiving any ambulatory care service, as shown in Table 3. Recipients of individual therapy tended to be under 65, to be female, to have more comorbid psychiatric illnesses, and to be covered by Medicare only. For African Americans, the likelihood of receiving individual therapy was 74 percent that of Caucasians.
Introduction of the interaction between race and age into the model resulted in a better fit of the statistical model for receipt of any ambulatory care service and for individual therapy. The adjusted parameter estimate indicated that among persons under 65, Caucasians were about 1.5 times as likely as African Americans to have received any ambulatory care service (95 percent CI=1.17 to 1.84) and 1.3 times as likely to have received individual therapy (CI=1.05 to 1.6). The log-likelihood ratio of the improvement in the overall fit of the model for individual therapy that resulted from the inclusion of the race-by-age interaction was statistically significant (χ2=11.76, df=7, 564, p<.001).
A slightly stronger parallel race-by-age interaction was observed for the use of any ambulatory care service (OR=1.46, p<.001). Similarly, the expanded model for use of any service fit reasonably well (χ2=8.52, df=9, 406, p<.01). Persons who had Medicaid coverage were significantly more likely than persons who did not have Medicaid coverage to have received group therapy. Persons under 65 were more likely than older persons to have received group therapy. The use of family therapy was significantly related only to age: persons who were 65 or older were less likely to have received family therapy. Psychiatric somatotherapy was more likely to have been used by persons younger than 65, persons with Medicaid coverage, and persons with fewer comorbid psychiatric illnesses.
Demographic factors. Being under the age of 65 was consistently associated with a greater likelihood of using services. Persons who were 65 or older were about half as likely to have received any service, as well as individual, group, or family therapy. African Americans under the age of 65 were significantly less likely to have received any service or individual therapy than Caucasians in the same age group. Women were more likely than men to have received any service, particularly individual therapy.
Medicaid enrollment was associated with a lower likelihood of receiving individual therapy but a greater likelihood of receiving group therapy or psychiatric somatotherapy. In contrast, persons with more comorbid psychiatric illnesses were more likely to have received individual therapy and less likely to have received psychiatric somatotherapy. Finally, a diagnosis of substance abuse was associated with a lower likelihood of use of any service.
Cost factors
In most cases, the factors associated with higher costs of care were also associated with a greater likelihood of service use, as shown in Table 4. Higher costs were observed among Caucasians, younger persons, Medicaid recipients, persons with a drug abuse disorder, and persons with comorbid psychiatric conditions. The higher costs may be explained by the fact that these groups were more likely to have received individual therapy.
Significant interactions were also observed between race and age in the cost of care for persons who received individual therapy and for persons who received any ambulatory care service. The mean cost difference for any service between African Americans and Caucasians was significantly greater in the younger group than the older group. However, the difference by race and the age-race interaction were not observed for costs of group therapy, family therapy, or psychiatric somatotherapy. All fitted models included indicator variables to adjust for regional cost differences. Given the conservative selection strategy, the models fit modestly well (adjusted R2=.11 to .13), excluding the model for group therapy.
Discussion and conclusions
The results of this study suggest that the types and costs of Medicare-covered ambulatory care services provided to persons with schizophrenia vary nationally according to specific clinical and demographic characteristics. Overall, one cause for concern is that for about one-fourth of persons with Medicare coverage and a claims-based diagnosis of schizophrenia, the claims data contained no evidence that any ambulatory care service had been provided by a physician in 1991. It is possible that these individuals received care from nonphysician providers or received care that was covered by Medicaid, the Department of Veterans Affairs, or some other payer. However, Medicare, as the primary insurer, would have been expected to play a role in the care of these patients. A troubling implication is that these individuals may have received only acute care.
Schizophrenia is a severe, chronic, and disabling illness. That a person would receive no medical ambulatory care services in an entire calendar year is incompatible with any standard for quality or continuity of care. In our sample, the mean number of visits for any service during the year was approximately eight, or about one visit every 1.5 months. Although there are no widely accepted specific standards for assessing the optimal frequency of visits, eight visits a year for stable outpatients may be a reasonable number. However, given that a substantial minority of patients—around 25 percent—are likely to be in an acute or subacute phase of illness during any given year, eight visits appears to be insufficient for the provision of high-quality care (15).
Again, it is possible that some of these patients received nonreimbursed services or services paid for by a non-Medicare insurer. Fifty-three percent of the patients in our sample were also covered by Medicaid, which typically covers some of the services not covered by Medicare, such as rehabilitation or assertive community treatment and case management. Medicare does not cover many services that are frequently needed by persons with schizophrenia, and their care in the absence of such services may be inadequate. Because we did not assess specific patterns or episodes of care, comments about the appropriateness of care are speculative.
The prevalent psychiatric practice mode in the United States is individually based therapy. The 60 percent rate of participation in individual therapy in our sample was almost nine times greater than the rate of participation in group therapy. The use of psychiatric somatotherapy—an individually determined treatment—also exceeded the use of family and group therapy. Although family therapy is effective, it was rarely used. The Medicare claims we examined suggest that the potential cost-efficiencies and clinical benefits of group and family therapy that are articulated in best-practice standards are not realized in the current U.S. health care system (5,7,16). Medicare applies the same limits and copayments to psychiatric somatotherapy as to other medical outpatient services but covers psychotherapies with a copayment of 50 percent. Thus there might be an inherent incentive to provide somatotherapy as an alternative to psychotherapy.
In this sample, race was strongly associated with the likelihood of receiving care and with the costs of care. This finding is cause for concern because it implies underprovision of care to African Americans. Younger African Americans were less likely to have received any ambulatory care service under Medicare, largely because of their lower use of individual therapy. The odds ratio of .74 (CI=.67 to .82) in the comparison by race of those receiving individual therapy is noteworthy on a population basis, both statistically and clinically. Furthermore, among persons who received any service, African Americans incurred lower overall costs for ambulatory care in general and for individual therapy and family therapy in particular.
However, use of psychiatric somatotherapy and group therapy was not associated with race. The misconception that African Americans are not appropriate candidates for psychotherapy has been discussed elsewhere (17). Undertreatment of African Americans has been found for other illnesses (18,19,20). The exclusion of services covered by Medicaid does not appear to account for this finding, because there were no racial differences in rates of Medicaid coverage. African Americans may have received more inpatient care, which would be cause for even greater concern, because it could mean that inadequate community treatment led to a greater use of inpatient services.
The greater use and cost of services among younger persons is consistent with the severity of schizophrenia among younger persons and the attenuation of symptoms with age (21,22). However, undertreatment of schizophrenia among elderly persons is also possible. The finding that women were more likely than men to have received any service or individual therapy suggests that men may have experienced undertreatment at the point of engagement in services. For example, there is some evidence that men with schizophrenia have poorer outcomes and are more likely to have a greater severity of illness than women, which could imply that men require more service use and more costly care (23,24). In fact, men may use more inpatient services. It is also possible that better treatment compliance among women explains the greater likelihood of their using ambulatory care services. The costs for women and men, once in treatment, were the same.
The association of a greater number of comorbid psychiatric illnesses with greater costs and with a greater probability of receiving individual therapy was not surprising. Comorbid psychiatric illnesses may be a proxy for complexity of illness and thus may indicate a greater need for services. A greater number of care visits also increases the chances that additional diagnoses will be made, which is a form of detection bias. Interestingly, having more comorbid psychiatric illnesses was associated with less use of psychiatric somatotherapy, which can be seen as consistent with good care. Patients with multiple comorbid psychiatric illnesses need more than a medication check. In general, drug abuse was associated with greater costs of care but a lower probability of any service use. This finding suggests a higher cost per episode and increasingly erratic care, which is compatible with the results of previous research on service use by persons with substance abuse problems (25,26).
The variations we observed in patterns of service use that were related to Medicaid and Medicare dual eligibility may be explained by the fact that better services are often available under Medicaid than under Medicare. Many states have taken advantage of Medicaid options to offer a broader range of community-based supports and psychosocial services, especially expanded case management, patient and family psychosocial services, rehabilitation, and assertive community treatment. Capitation approaches used in mental health carve-outs under Section 1115 also may promote more service options.
Medicare does not have a pharmacy benefit and does not offer the community-based options available under Medicaid to pay for case management, family psychoeducation, rehabilitation, supported employment, and assertive community treatment. The lower rates of individual psychotherapy among persons with dual eligibility may reflect the substitution of other Medicaid-eligible services for individual therapy—for example, case management and rehabilitation. The fact that Medicaid has a pharmacy benefit may account for the greater use of psychiatric somatotherapy among patients covered by Medicaid. Hence it is not surprising that dually eligible patients received more services overall.
As with all claims-based studies, our study relied on diagnoses that may have been of questionable validity. However, diagnoses of schizophrenia on Medicaid claims have been found to be reliable when verified by a structured clinical interview (Lehman A, unpublished data, 2001). The results of other studies also support claims-based identification of persons with schizophrenia (27). The extent to which billing patterns were influenced by local practices—for example, individual medical psychotherapy compared with psychiatric somatotherapy—is unknown.
The results of this study affirm that more attention needs to be given to the quiet periods of schizophrenia, when patients are not acutely psychotic but are living with a chronic disability. Many of these patients receive very little care because they are considered to be stable by caregivers at the available mental health services, which focus on acute care. However, these patients often endure persistent negative symptoms, low-grade positive symptoms, depression, social isolation, passivity, unemployment, and poverty. It is important to link these service-delivery patterns to quality-of-care standards. Care of acceptable quality should involve a range of interventions to address these continuing problems (28). Such care should include careful adjustment of medications, counseling to help individuals to cope with schizophrenia, family education and support, vocational and educational services, skills training, and assertive community treatment.
Acknowledgments
The Schizophrenia Patient Outcomes Research Team (PORT) was funded by the Agency for Health Care Policy and Research and the National Institute of Mental Health (contract 282-92-0054).
Dr. Dixon, Dr. Postrado, Dr. Lucksted, and Dr. Lehman are affiliated with the Center for Mental Health Services Research at the University of Maryland School of Medicine in Baltimore and with the Department of Veterans Affairs Capitol Health Care Network Mental Illness Research, Education, and Clinical Care Center, 701 West Pratt Street, Floor 4, Baltimore, Maryland 21201 (e-mail, [email protected]). Dr. Lyles is affiliated with the University of Baltimore. Mr. Smith and Ms. Fahey are affiliated with the Johns Hopkins School of Public Health in Baltimore. Dr. Hoch is affiliated with the University of Western Ontario in London, Ontario, Canada
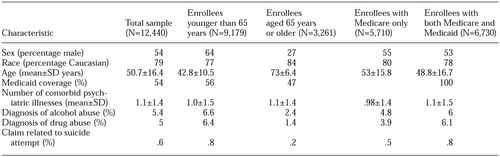 |
Table 1. Characteristics of Medicare enrollees with schizophrenia, by age group and Medicaid and Medicare coverage
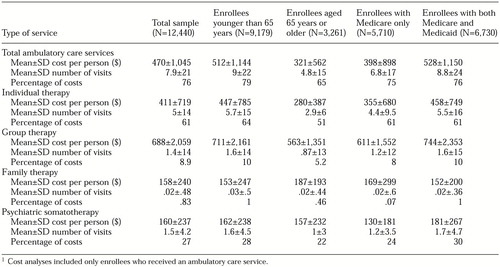 |
Table 2. Costs and use of ambulatory care services among Medicare enrollees with schizophrenia, by age group and Medicaid and Medicare coverage11
Cost analyses included only enrollees who received an ambulatory care service
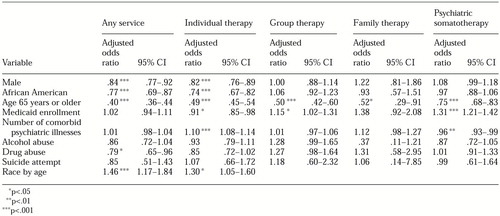 |
Table 3. Logistic regression analysis of selected factors associated with type of ambulatory care service in a random sample of 12,440 Medicare enrollees with schizophrenia
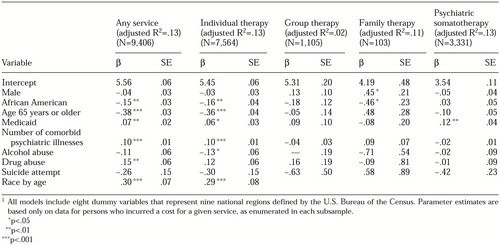 |
Table 4. Regression models of factors associated with mean log cost per person per year, in dollars, by type of ambulatory care service in a random sample of 12,440 Medicare enrollees with schizophrenia11
All models include eight dummy variables that represent nine national regions defined by the US. Bureau of the Census. Parameter estimates are based only on data for persons who incurred a cost for a given service, as enumerated in each subsample.
1. Norquist GS, Regier DA, Rupp A: Estimates of the cost of treating people with schizophrenia: contributions of data from epidemiologic surveys, in Handbook of Mental Health Economics and Health Policy: Schizophrenia, vol 1. Edited by Moscarelli M, Rupp A, Sartorius N. New York, Wiley, 1996Google Scholar
2. Rupp A, Keith S: The costs of schizophrenia: assessing the burden. Psychiatric Clinics of North America 16:413-431, 1993Crossref, Medline, Google Scholar
3. Larson MJ, Farrelly MC, Hodgkin D, et al: Payments and use of services for mental health, alcohol, and other drug abuse disorders: estimates from Medicare, Medicaid, and private health plans, in Center for Mental Health Services Mental Health, United States, 1998. Edited by Manderscheid RW, Henderson MJ. DHHS pub (SMA)99-3285. Washington, DC, US Government Printing Office, 1998Google Scholar
4. Martin BC, Miller LS: Expenditures for treating schizophrenia: a population-based study of Georgia Medicaid recipients. Schizophrenia Bulletin 24:479-488, 1998Crossref, Medline, Google Scholar
5. Lehman AF, Steinwachs D: Translating research into practice: the Schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophrenia Bulletin 24:1-10, 1998Crossref, Medline, Google Scholar
6. Lehman AF, Steinwachs DM, Dixon LB, et al: Initial results from the Schizophrenia PORT client survey. Schizophrenia Bulletin 24:11-19, 1998Crossref, Medline, Google Scholar
7. Dixon L, Lyles A, Scott J, et al: Services to families of adults with schizophrenia: from treatment recommendations to dissemination. Psychiatric Services 50:233-238, 1999Link, Google Scholar
8. Health Care Financing Administration: Medicare Basics. Washington, DC, 2001. Available at http://www.medicare.gov/basics/overview.aspGoogle Scholar
9. Health Care Financing Administration: Medicare Enrollment Trends:1966-1999. Washington, DC, 2001. Available at http://www.hcfa.gov/stats/enrltrnd.htm#t1Google Scholar
10. Moon M: Medicare Now and in the Future. Washington, DC, Urban Institute, 1996Google Scholar
11. Lehman AF, Steinwachs DM: Secondary Data Analysis: Schizophrenia Patient Outcomes Research Team (PORT). Contract 282-92-0054. Rockville, Md, Agency for Health Care Policy and Research, 1994Google Scholar
12. Cano C, Hennessy KD, Warren JL, et al: Medicare part A: utilization and expenditure for psychiatric services. Health Care Financing Review 18(3):177-193, 1997Google Scholar
13. American Medical Association: Physicians' Current Procedural Terminology, 4th ed. Chicago, Ill, 1995Google Scholar
14. SAS/STAT User's Guide. Version 6. Cary, NC, SAS Institute, Inc, 1990Google Scholar
15. Weiden PJ, Olfson M: Cost of relapse in schizophrenia. Schizophrenia Bulletin 21:419-429, 1995Crossref, Medline, Google Scholar
16. Scott JE, Dixon LB: Psychological interventions for schizophrenia. Schizophrenia Bulletin 21:621-630, 1995Crossref, Medline, Google Scholar
17. Baker FM, Bell CC: Issues in the psychiatric treatment of African Americans. Psychiatric Services 50:362-368, 1999Link, Google Scholar
18. Kasiske BL, London W, Ellison MD: Race and socioeconomic factors influencing early placement on kidney transplant waiting list. Journal of the American Society of Nephrology 9(21):42-47, 1998Google Scholar
19. Ferguson JA, Tierney WM, Westmoreland GR, et al: Examination of racial differences in management of cardiovascular disease. Journal of the American College of Cardiologists 30:1707-1713, 1997Crossref, Medline, Google Scholar
20. Ford ES, Cooper RS: Racial/ethnic differences in health care utilization of cardiovascular procedures: a review of the evidence. Health Services Research 30:237-252, 1996Google Scholar
21. Mason P, Harrison G, Glazebrook C, et al: Characteristics of outcome in schizophrenia at 13 years. British Journal of Psychiatry 167:596-603, 1995Crossref, Medline, Google Scholar
22. Carpenter W, Strauss J: The prediction of outcome in schizophrenia: IV. eleven-year follow-up of the Washington IPSS cohort. Journal of Nervous and Mental Disease 179:517-525, 1991Crossref, Medline, Google Scholar
23. Childers SE, Harding CM: Gender, premorbid functioning, and long-term outcome in DSM-III schizophrenia. Schizophrenia Bulletin 16:309-318, 1990Crossref, Medline, Google Scholar
24. Angermeyer MC, Kuhn L, Goldstein JM: Gender and the course of schizophrenia: differences in treated outcomes. Schizophrenia Bulletin 16:293-307, 1990Crossref, Medline, Google Scholar
25. Dixon L: Dual diagnosis of substance use in schizophrenia: prevalence and impact on outcomes. Schizophrenia Research 35: S93-S100, 1999Google Scholar
26. Dickey B, Azeni H: Persons with dual diagnoses of substance abuse and major mental illness: their excess costs of psychiatric care. American Journal of Public Health 86:973-977, 1996Crossref, Medline, Google Scholar
27. Lurie N, Popkin M, Dysken M, et al: Accuracy of diagnoses of schizophrenia in Medicaid claims. Hospital and Community Psychiatry 43:69-71, 1992Abstract, Google Scholar
28. Lehman AF: Quality of care in mental health: the case of schizophrenia. Health Affairs 18(5):52-65, 1999Google Scholar



