One-Year Rehospitalization Rates of Patients Discharged on Atypical Versus Conventional Antipsychotics
Abstract
This study examined one-year rehospitalization rates for patients who were discharged from Austin State Hospital between August 1, 1997, and July 31, 1998, while taking olanzapine, risperidone, or a conventional antipsychotic. Time to readmission was measured by the product-limit formula. Although conventional antipsychotics were associated with a lower rehospitalization rate, no significant difference in the one-year rehospitalization rate was observed between the groups. At 180 days after initial discharge, the patients who received olanzapine had a higher rate of rehospitalization than patients who were taking conventional antipsychotics. Conventional antipsychotics were associated with a lower one-year rehospitalization rate than risperidone or olanzapine.
Antipsychotic medications have been shown to reduce rehospitalization rates among patients with schizophrenia. Hogarty (1) reported a one-year rehospitalization rate of 37 percent among patients who were treated with conventional antipsychotics. Decanoate antipsychotics are associated with better adherence rates than oral conventional antipsychotics and also have been associated with lower recidivism rates. Moore and colleagues (2) found that one-year rehospitalization rates among patients who were treated with fluphenazine decanoate or haloperidol decanoate were 21 percent and 36 percent, respectively. Love and colleagues (3) reported a one-year rehospitalization rate of 26 percent among patients who were taking either fluphenazine decanoate or haloperidol decanoate.
The newer, atypical antipsychotics have more favorable side effect profiles and may be associated with better compliance with medication regimens and fewer rehospitalizations. Several studies have demonstrated lower one-year rehospitalization rates among patients with schizophrenia who received clozapine, olanzapine, or risperidone (2,3,4). However, in a recent study by Rabinowitz and colleagues (5), 83 (31 percent) of 268 patients who were treated with risperidone and 88 (28 percent) of 313 patients who were treated with olanzapine were rehospitalized within a year, compared with 160 (35 percent) of 458 patients who received conventional antipsychotics.
The purpose of our study was to compare one-year rehospitalization rates among patients with schizophrenia or schizoaffective disorder who were discharged from the hospital while taking risperidone, olanzapine, or a conventional antipsychotic.
Methods
All patients between the ages of 18 and 65 years who were discharged from Austin State Hospital between August 1, 1997, and July 31, 1998, with a diagnosis of schizophrenia or schizoaffective disorder were considered for the study. Further inclusion criteria required that patients had been discharged on a regimen of risperidone, olanzapine, or a conventional antipsychotic (oral or decanoate). Excluding other antipsychotics, concurrent psychotropic and anticholinergic medications were allowed. Patients with another axis I disorder, excluding a substance use disorder, and patients who were taking clozapine at discharge were not eligible for the study. Readmission was defined as rehospitalization in Austin State Hospital for a psychiatric condition. Rehospitalization status was examined through July 31, 1999.
All data were collected from databases at Austin State Hospital and the Texas Department of Mental Health and Mental Retardation Central Office. Chart reviews were conducted to verify the data. The study was approved by the institutional review board of Austin State Hospital.
One-year rehospitalization rates of eligible patients were examined. To reduce the effects of risk factors for readmission, patients in each medication group were matched with respect to age (within ten years), sex, and race. Recidivism rates of the patients in each of the three groups were compared with each other.
Time to rehospitalization was measured by the Kaplan-Meier product-limit formula (6). The significance of differences between the three medication groups was measured by the Mantel-Cox chi square test.
Differences between the survival curves were also measured at 90-day intervals with the Mantel-Haenszel chi square test (6). The Cox proportional-hazards regression model was used to analyze continuous covariates as well as those thought to influence time to readmission, such as age and duration of hospitalization (6). Nonparametric tests were used to compare demographic variables. All tests were two-tailed, and significance was defined as an alpha of .05 or less.
Results
A total of 305 patients met inclusion criteria for the study: 95 who were taking olanzapine, 73 who were taking risperidone, and 137 who were taking a conventional antipsychotic. After the patients were matched for age, sex, and race, a total of 195 were included in the study—65 in each drug group. Of the 65 patients in each group, 41 (63 percent) were male and 42 (65 percent) were Caucasian. The mean±SD age of the patients in the olanzapine group was 39.1±9 years; in the risperidone group, 37.4±9.7 years; and in the conventional group, 38.6±8.9 years. The mean length of stay for the olanzapine group was 59±98.9 days; for the risperidone group, 75±127 days; and for the conventional group, 56±50.5 days. The differences between the three groups were not significant. Of the patients who were taking a conventional antipsychotic, 41 (63 percent) were taking an oral agent and 24 (37 percent) were receiving decanoates.
Time to rehospitalization for the patients in the three groups is shown in Figure 1. Thirty-five percent of the patients who were taking risperidone, 34 percent of the patients who were taking olanzapine, and 20 percent of the patients who were taking a conventional antipsychotic were readmitted within one year after discharge. These differences were not significant. At 180 days, the patients who were taking olanzapine had a significantly higher rate of rehospitalization than those who were taking conventional antipsychotics (Mantel-Haenszel χ2=3.981, df=1, p=.046).
Of the 24 patients who were receiving decanoates, three (13 percent) were rehospitalized; ten (24 percent) of the 41 patients who were taking oral conventional antipsychotics were rehospitalized within one year. This difference was not significant. A significant difference in readmission rates at 90 days was observed, as patients who were taking oral dosages had more readmissions (Mantel-Haenszel χ2=4.521, df=1, p=.033).
In all three groups, age or duration of hospitalization was not associated with the risk of rehospitalization.
Discussion and conclusions
Patients who were taking olanzapine were more likely to be readmitted to the hospital during the first 180 days after discharge than patients who were taking a conventional antipsychotic. Patients who were taking an oral conventional antipsychotic when discharged from the hospital were more likely to be readmitted than patients who were receiving decanoates, especially during the first 90 days. In all groups, the risk of rehospitalization was highest during the first three months after discharge.
Conventional antipsychotics were associated with lower one-year rehospitalization rates than atypical antipsychotics. The one-year rehospitalization rate of 20 percent with conventional antipsychotics is lower than the rate of 35 percent reported by Rabinowitz and colleagues (5) and the rate of 37 percent reported by Hogarty (1). The rate of 13 percent among the patients in our study who were receiving decanoates is also less than the rates reported by Moore and colleagues (2) and by Love and colleagues (3). Patients who were treated with olanzapine or risperidone had similar one-year rehospitalization rates—34 percent and 35 percent, respectively. These rates are higher than those found in some previous studies (2,3,4) but are comparable to the findings of Rabinowitz and colleagues (5).
There are several possible explanations for the considerable difference in rehospitalization rates between patients who were treated with conventional and atypical antipsychotics. First, a period of two years may be necessary to clearly demonstrate the advantages of atypical antipsychotics and the disadvantages of conventional antipsychotics, as illustrated in the study by Rabinowitz and colleagues. We used a one-year period, which may not have been enough time in which to see the possible long-term reduction in rehospitalization rates with olanzapine or risperidone. Second, it is possible that the duration of hospitalization is correlated with the severity of the mental illness—for example, patients who received conventional antipsychotics may have been less ill and easier to stabilize. Third, being discharged from the hospital does not necessarily imply that the medication was continued in the outpatient sector. We did not have access to outpatient prescription records, so we were unable to determine whether these medications were continued by the patient or the outpatient provider.
Rehospitalization rates and relapse rates are not synonymous. Relapse denotes a clinically significant exacerbation of psychotic symptoms. Patients who experience relapse may not be hospitalized, which is increasingly the case in today's managed care environment. To be admitted to a Texas state hospital, persons with mental illness must be a danger to themselves or others or experience significant deterioration. Rehospitalization rates provide no information about control of symptoms or functional status among patients who remain in the community.
This study had several limitations. Side effects, noncompliance with medication regimens, and comorbid substance use disorders have been associated with increased rehospitalization rates among patients with schizophrenia (7). We did not address these factors and do not know what influence they may have had on our results. Furthermore, we did not evaluate the duration of treatment with antipsychotics before discharge. Patients who were discharged early after beginning a trial of an antipsychotic drug may not have been stabilized or may not have tolerated the medication as well as patients who had longer trials.
This study showed that patients who were discharged while taking conventional antipsychotics were less likely to be rehospitalized within one year than patients who were taking olanzapine or risperidone. Although the patients who received oral medications and those who received decanoates had different rehospitalization rates, the difference was not statistically significant. However, the small number of patients who were receiving decanoates made it difficult to establish significance. Many factors—both patient-specific and external—can affect rehospitalization rates among patients with schizophrenia. Rehospitalization rates and other disorder-related outcomes must be examined in many different mental health systems before generalized comments can be made about specific effects of antipsychotic medications on outcomes.
Dr. Patel and Dr. Dorson are affiliated with Austin State Hospital, Texas Department of Mental Health and Mental Retardation, and the College of Pharmacy of the University of Texas at Austin. Dr. Edwards is with the Fort Defiance Indian Hospital in Fort Defiance, Arizona. Dr. Mendelson is with Pharmaceutical Informatics, e-MDs, in Austin. Dr. Crismon is with the College of Pharmacy of the University of Texas at Austin and with the office of the medical director of the Texas Department of Mental Health and Retardation. Send correspondence to Dr. Crismon at the College of Pharmacy, University of Texas, Austin, Texas 78712 (e-mail, crismonlmail.utexas.edu). A version of this paper was presented at the midyear clinical meeting of the American Society of Health-System Pharmacists, held December 3-7, 2000, in Las Vegas and at the annual meeting of the New Clinical Drug Evaluation Unit of the National Institute of Mental Health, held May 28, 2001, in Phoenix.
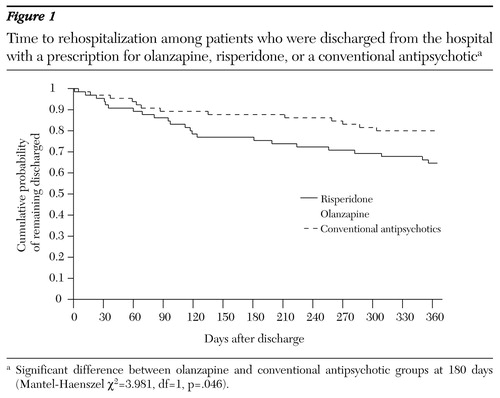
Figure 1. Time to rehospitalization among patients who were discharged from the hospital with a prescription for olanzapine, risperidone, or a conventional antipsychotica
a Significant difference between olanzapine and conventional antipsychotic groups at 180 days (Mantel-Haenszel χ2=3.981, df=1, p=.046).
1. Hogarty GE: Prevention of relapse in chronic schizophrenic patients. Journal of Clinical Psychiatry 54(Mar suppl):18-23, 1993Google Scholar
2. Moore DB, Kelly DL, Sherr JD, et al: Rehospitalization rates for decanoate antipsychotics and pharmacoeconomic implications: comparison with risperidone. American Journal of Health-System Pharmacy 55(suppl 4):17-19, 1998Google Scholar
3. Love RC, Conley RR, Kelly DL, et al: Rehospitalization rates with the atypical antipsychotics in the Maryland mental health system. Schizophrenia Research 36:345, 1999Google Scholar
4. Conley RR, Love RC, Kelly DL, et al: Rehospitalization rates of patients recently discharged on a regimen of risperidone or clozapine. American Journal of Psychiatry 156:863-868, 1999Link, Google Scholar
5. Rabinowitz J, Lichtenberg P, Kaplan Z, et al: Rehospitalization rates of chronically ill schizophrenic patients discharged on a regimen of risperidone, olanzapine, or conventional antipsychotics. American Journal of Psychiatry 158:266-269, 2001Link, Google Scholar
6. Friedman LM, Furberg CD, DeMets DL: Fundamentals of Clinical Trials, 2nd ed. Littleton, Mass, PSG, 1985Google Scholar
7. Olfson M, Mechanic D, Hansell S, et al: Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiatric Services 51:216-222, 2000Link, Google Scholar



