Recidivism and Use of Services Among Persons With Mental Illness After Release From Prison
Abstract
OBJECTIVE: Despite large numbers of mentally ill offenders in prisons, few studies of mentally ill offenders released from prison have been conducted. This study describes such a population of mentally ill offenders, the postrelease services they received, new offenses they committed, and factors associated with recidivism. METHODS: The authors reviewed electronic files and archived medical charts from the state corrections department to identify mentally ill offenders who left Washington state prisons in 1996 and 1997. Data on the individuals identified were then provided by several public agencies. Summary statistics were computed on subjects' characteristics and postrelease outcomes, and logistic regression analysis was used to identify variables that predicted convictions of new felonies and new crimes against persons. RESULTS: A total of 337 mental ill offenders were identified. Men and women differed with regard to offenses, diagnoses, rates of drug abuse, and use of mental health resources. Although most subjects (73 percent) received postrelease social or mental health services, few received clinically meaningful levels of service during the first year after release. Charges for new crimes or supervision violations were common (70 percent of subjects), but only 10 percent committed new felonies against persons, and 2 percent committed very serious crimes. Youth, frequency of past felonies, and variables such as misbehavior in prison were associated with new offenses. CONCLUSIONS: Whether community mental health treatment affects recidivism cannot be assessed fairly in the absence of higher levels of service during the first months after release. This study also identifies actuarial risk factors that predict new offenses at a level comparable to that of published risk assessment instruments. Commission of less serious offenses that usually precede felonies may provide an early warning of risk for new felonies and an opportunity for strategic intervention. The low rate of serious violence in the community by mentally ill offenders released from prison suggests that the risk of violence may be a weak and potentially counterproductive rationale for community support and mental health treatment of mentally ill offenders.
Prevalence estimates of the number of mentally ill offenders in U.S. prisons range from 6 percent (1) to 16 percent (2,3). Regardless of the source of the estimate, the absolute number is high. In 1997, there were approximately 1,175,000 inmates in state and federal prison (4), among whom 70,000 to 190,000 had mental illness.
Despite the high numbers of mentally ill offenders, surprisingly little is known about their adjustment after release from prison to the community. Most outcome studies of persons with mental illness in institutions have focused on community outcomes for individuals adjudicated not guilty by reason of insanity (5,6,7,8,9) or on criminal recidivism by civilly committed patients after release from psychiatric hospitals (10).
In one of the few outcome studies of mentally ill offenders released from prison, Feder (11,12) reported that 64 percent of mentally ill offenders were rearrested within 18 months of release, compared with 60 percent of offenders without mental illness; 48 percent of the mentally ill offenders were hospitalized during those first 18 months, compared with 1 percent of those without mental illness. Although Feder's work was groundbreaking, it involved a relatively small sample (147 mentally ill offenders) and left open many questions about the amount and the timing of social services and other postrelease outcomes. With the exception of reports by Jacoby and Kozie-Peak (13) (N=27) and Wilson and colleagues (14) (N=59), we know of no reports of outcome studies of mentally ill offenders released from state prisons.
There is little doubt that communities, community agencies, and practitioners are concerned about the safe management of mentally ill offenders in the community. Indeed, the usual prejudices that hinder community treatment of the mentally ill (15,16,17) may be more severe for mentally ill offenders (18,19), who may be thought to pose a greater risk to public safety. In our experience, community agencies and practitioners sometimes assess mentally ill offenders' risk of violence inaccurately and overestimate their professional liability risks. Thus they may be reluctant to provide outpatient treatment for mentally ill offenders.
In this article, we report community outcomes for 337 mentally ill offenders released from Washington's state prisons in 1996 and 1997. Our study was limited to mentally ill offenders released from prison who have severe, persisting mental disorders that substantially impair cognitive or volitional functioning and require continuing treatment. Persons with schizophrenia and major affective disorders were included, but unless they suffered from other severe mental illness, persons with paraphilias or personality disorders other than borderline personality disorder were excluded. Our goal was to provide an empirical, reality-based picture of mentally ill offenders released from prison on the basis of their prerelease characteristics, the community services they typically receive in Washington State, the kinds and amounts of crime they commit when they recidivate, and the commonly available prerelease variables that best predict recidivism.
Methods
Subject selection
Internal review boards at the University of Washington, the Department of Corrections, and the Department of Social and Health Services examined and approved our study proposal. Records from these agencies were used without contacting the study subjects, in accordance with federal guidelines for consent waivers, given feasibility and confidentiality guarantees. Study subjects comprised all identified mentally ill offenders released from prison in 1996 and 1997. The aim to include the total population rather than a sample of it reflected both the number of subjects that we expected to need for statistically significant analyses and comparisons and our belief that a valid sample required reliable methods of delineating the pool of subjects. The methods we used had not been developed before the study. Although the Department of Corrections had set up screening and treatment programs for prisoners with mental illness, mental health status was not an established part of its classification system until 1997. For offenders who were released in 1996 and 1997, we could not expect uniform, reliable, and comprehensive assessment of mental health status. In addition, it was not universal practice to record formal, centrally available diagnoses for all those who were treated for serious mental illness.
To circumvent these obstacles, we identified potential subjects through a combination of indicators in the computerized offender-tracking system of the Department of Corrections. Indicators included mental health bed residence, prison hospitalizations, appearance in psychotropic medication records, and intake screening flags for possible mental illness. We then reviewed archived medical charts and certified candidates as mentally ill—and therefore as study subjects—if they met two of the following three criteria: more than 30 days in a prison residential mental health treatment program; prescription of listed antipsychotic, mood stabilizing, or antidepressant medications, excluding off-label and low dosages of medications administered for sleep or stress disorders; and a recorded diagnosis of schizophrenia or other psychotic disorders, bipolar disorder, major depression, dementia, or borderline personality disorder.
Our medical chart review identified 259 study subjects. Charts were unavailable for 180 candidates who were under supervision or had returned to prison, and 78 of these were qualified as mentally ill on the basis of recently improved Department of Corrections electronic records that described the person as mentally ill or on the basis of Mental Health Division records of past community mental health treatment. A checklist of specific medications, minimum dosages, diagnoses, and decision rules is available from the corresponding author, as is the study's data dictionary with a complete list and operational definitions of the study variables.
Information available in archived medical charts did not allow an assessment of the degree to which the subject's functioning was impaired by a diagnosed, medicated qualifying disorder as opposed to other factors, such as psychosocial trauma or drug abuse. Thus our criteria inevitably introduced some slippage in the conservative definition of mental illness cited above, particularly for women who had a diagnosis of depression.
Data collection, assembly, and analysis
In Washington State, mental health care for mentally ill offenders is provided entirely by the Department of Corrections (20) rather than by a separate state mental health service agency. When offenders move from the Department of Corrections to the community, responsibility for mental health care is transferred to providers associated with the Mental Health Division of the Department of Social and Health Services. The absence of established administrative and information systems to monitor the transition from offender to consumer status hampers both collaboration between agencies and subsequent assessment of outcomes. For our study, considerable effort was required to match subject identifiers between various state and local agencies and then combine records with diverse coding and data structures. With the cooperation of participating agencies, we collected the following data: demographic variables—sex, age, and ethnicity; criminal history data—past charges, dispositions, and convictions; prison terms, mental health bed use, infractions, and segregation; postrelease monthly use of general assistance and other state-managed entitlements as well as food stamps and drug and alcohol abuse services; preincarceration and postrelease monthly data on days of inpatient service use and hours of outpatient mental health service use; and Washington State postrelease charges, dispositions, supervision violations, and felony sentence lengths. Out-of-state arrest data were retrieved from the National Crime Information Center.
Files were cross-checked for errors and inconsistencies and then combined, recompiled, and summarized. Some recoding was done for presentation purposes, and standard descriptive statistics were generated. Logistic regression analysis was used to analyze risk factors for future offenses.
The duration of follow-up depended on subjects' release dates. Social services data were collected through late 1999, yielding a follow-up period ranging from 19 to 47 months, averaging 31 months; for recidivism data, collected through mid-2000, follow-up ranged from 27 to 55 months and averaged 39 months.
Results
Profile of subjects
Compared with all offenders released during a 12-month period within our two-year study period (21), slightly more study subjects were white (72 percent versus 67 percent) and fewer were black (23 percent versus 27 percent). In both groups, Native Americans (4 percent versus 3 percent) accounted for most of the remainder of the subjects, but Hispanic origin was attributed to fewer subjects (9 percent versus 17 percent). Subjects had a lower rate of drug offenses and a higher rate of sex offenses than all released offenders did and had served more time in prison for their index offense. The biggest difference between subjects and all offenders, however, lay in the number of women in the study. Their proportion (30 percent) was more than three times their representation in the population leaving prison (9 percent). As Table 1 shows, men differed both from women and from all released offenders in index offenses and length of stay. As Table 2 shows, we also found substantial differences between men and women in diagnoses, medications, use of residential mental health beds, levels of drug abuse, and postrelease community mental health services.
Compared with men, women were three times as likely to be diagnosed as having depression and almost twice as likely to have reported a history of serious drug abuse. They spent half as much time in prison residential mental health treatment and received less community mental health service during the first year after release. These differences may have been due to differences in issues that bring women into contact with prison mental health providers (22,23). For example, women inmates may seek and obtain prison mental health services because of traumatic or stressful events more than men do. Such triggering events may be linked to drug abuse and expressed in depressive symptoms. Differences between male and female subjects in community mental health treatment rates may have been due to the high number of women with depression who qualified as subjects because they sought outpatient treatment in prison but did not require prison residential treatment and may not have met eligibility criteria for community mental health treatment. Additional underlying issues may include definitions of mental illness in prison settings (24), which, like sex differences, deserve further investigation in their own right.
Postrelease community services
The vast majority of study subjects received some social services or financial assistance after leaving prison, as Table 3 shows. In addition to community mental health services, almost a quarter of the subjects were hospitalized for mental health reasons, usually for only a few days, although 19 (6 percent) of them were hospitalized for more than three months, and four were excluded from the criminal recidivism analysis because they spent the entire study period hospitalized.
Because the vast majority (77 percent) of new offenses occurred during the first year after release, we looked closely at services received during this critical period. The statistics for social services provided during this period were not impressive. Fifty-two percent of the study subjects received cash assistance, and 50 percent received community mental health services in the first year, but only 25 percent received steady cash assistance—that is, during nine or more of the first 12 months after release—and 16 percent received steady community mental health services. Only 5 percent received steady drug and alcohol services during this period.
In addition to delays or interruptions, the intensity of community mental health treatment was low for most subjects during the first year after release from prison. Among 166 subjects who received first-year community mental health services, 15 received more than ten hours of service per month, not during the entire first year but only in months in which they were actually served, and on one occasion, 332 hours were counted for one subject in a single month. Typically, however, subjects received only two to five hours per service month (58 cases). This level of community mental health service may not suffice for people who face the multiple challenges of mental illness, substance abuse, and recent incarceration. As the study continues, we hope to shed more light on these issues by examining the service coordination narratives of community corrections and mental health staff.
Recidivism
The period of exposure for new offenses ranged from 27 to 55 months, depending on when subjects were released, and averaged 39 months. Renewed involvement with the criminal justice system was the norm, but, as Table 4 shows, the vast majority of subjects had been convicted for relatively less serious offenses such as supervision violations, misdemeanors, and property crimes. In addition to 232 subjects (70 percent) convicted of new offenses or supervision violations, 26 (8 percent) were arrested, 22 with unknown and four with not guilty dispositions. Only 32 subjects (10 percent) were convicted of felony crimes against persons, which were usually second-degree assault or robbery. Six subjects (2 percent) were convicted of very serious crimes, including one murder, two rapes, one first-degree assault, and two first-degree robberies.
We obtained Washington State recidivism data for all offenders who were released from Washington's state prisons during the same two-year period and followed for the same length of time. In this group, the felony recidivism rate was 37 percent—slightly less than the 41 percent rate among our study subjects, although our data included seven subjects (2 percent) whose only felonies had occurred in other states. Bearing in mind this limitation on comparability, the general population of former inmates committed serious offenses after release at the same rate as our study subjects. Ten percent committed felonies against persons, including 2 percent with serious violent offenses, including homicide, rape, and first-degree robbery or assault. Thus the most serious offenses were rare in both groups of released offenders.
In terms of incidence of offenses, supervision violations and misdemeanors by study subjects accounted for 628 (72 percent) of the 868 new incidents, and felony crimes against persons accounted for only 38 incidents (4.4 percent). Multiple new felonies by an individual subject were less common than multiple misdemeanors or violations, because felonies typically resulted in long terms of incarceration that limited further recidivism during the study period.
As Figure 1 shows, the rate of new felony commission was greatest during the first year or so after release and gradually decreased afterward, beginning to level off between two and three years after release. In most cases (86 persons, 63 percent), the first felony was preceded by other criminal justice encounters ("harbinger offenses"). In these cases, subjects averaged 3.4 previous arrests before committing their first felony offense. A similar pattern of harbinger offenses was observed before the index incarceration. Among 219 subjects serving their first Washington State prison term, 164 subjects (75 percent) had previous offenses, with a median of 3.5 and an average of 5.5 offenses, ranging up to 28 offenses.
Risk factors for recidivism
This section describes factors associated with two types of recidivism: new felonies and new crimes against persons. Felonies are more serious than misdemeanors, are more reliably documented on a statewide basis, and among released felons are more clearly cases of recidivism—that is, the commission of a new felony. We also focused specifically on crimes against persons because of interest among legislators and scholars in the question of violence by mentally ill offenders (25,26,27,28,29). Because violent felonies were rare, conviction for misdemeanor assaults was added to this category, yielding 77 cases (23 percent), a number sufficient for statistical analysis.
The 20 variables that showed significant correlations with these types of recidivism were also substantially correlated with one another, suggesting considerable redundancy in predicting recidivism. Hence we used stepwise logistic regression analysis to identify variables with the strongest independent, or nonoverlapping, association with recidivism. A comprehensive technical description of the various statistical procedures used in the analyses (logistic regression, negative binomial regression, and receiver operating characteristic [ROC] analyses) is in preparation as a separate report focused on the actuarial prediction of recidivism among mentally ill offenders. Logistic regression findings are reported here because of the binary nature of the dependent variables and the skewed distribution of some of the independent variables. One statistically significant predictor of new felonies—racial group (white versus other ethnic groups)—was omitted from the regression model because race can be used in an unfair, socially discriminatory manner and because research has shown that race per se has no unique predictive validity and tends to be merely a "social marker" for placement in neighborhoods with high degrees of concentrated poverty, an aspect of the community that has a strong association with criminal recidivism (30).
Forward logistic regression analysis was applied to surviving variables to generate predictive accuracy and other model statistics. Table 5 lists the predictor sets found for each type of recidivism.
Many of the variables we found to be associated with recidivism have been reported by others in previous studies. For example, being male, being young, and having committed previous violent felonies increase the likelihood of violence. One unexpected finding was the negative association between felony recidivism and being a first-time sex offender. This group includes first-time familial offenders who rarely recidivate; lower rates of felony recidivism could also reflect the more intensive levels of postrelease community supervision among sex offenders.
Discussion
We have reported the study's principal findings about the prerelease characteristics of study subjects, the kinds and amounts of community services they received in Washington State, their new offenses during the study period, and some common risk factors for recidivism. In each area are findings that merit further research as well as fuller discussion, including the role of sex differences, the factors that complicate psychiatric diagnosis in prison, and lower felony recidivism by first-time sex offenders.
Certainly, the factors that govern the quantity and quality of community mental health services that a person with mental illness receives after release from prison and their relationship to recidivism deserve intensive investigation. Subjects who committed new felonies tended to receive community mental health services later and in smaller amounts than did those who did not commit new felonies, but any causal relationships between these variables cannot be determined. The differences were substantial (felons averaged 60 percent as many monthly service hours as nonfelons during the first year in the community or until their first felony commission, and their first community mental health contact occurred two months later) but were not statistically significant. We report this trend as an observed difference in a total population, not as a basis for inference from our sample. Even if the relationships were statistically significant, the issue of confounding variables would prevent any attribution of causality to community mental health services.
First, being arrested and incarcerated for prefelony harbinger offenses may have kept some subjects from receiving services. Second, other plausible factors, such as a subject's lack of interest in working with counselors and community corrections officers, could have influenced both service use and recidivism. Although analytical techniques are available for addressing complex causality issues, such as Cox regression analysis, path analysis, and structural equation modeling, the low base rate of community mental health service received by study subjects in the early months after release and the absence of information about confounding factors, such as attitude toward treatment, make further analysis of whether increased community mental health services reduce mentally ill offender recidivism unpromising.
Another topic of concern for both policymakers and researchers is assessment of the risk of future offenses and future violence. According to one measure of predictive power, the area under the ROC curve (31), our simple predictor sets, based on ordinary correctional records, compare surprisingly well with widely accepted risk assessment instruments (32,33,34). Prospective cross-validation is required to determine how well these predictors forecast recidivism among new cohorts of mentally ill offenders leaving prison.
The nonclinical nature of the actuarial risk assessment measures we used should not be taken to imply that mental health plays no role in explaining or causing recidivism. Because routine clinical information such as diagnosis was often missing, clinical variables were disadvantaged as predictors. Furthermore, without recorded clinical assessments made at the time of release from prison, we were not able to investigate dynamic factors such as violent thinking, attitude toward treatment, level of functioning, and social support. In addition, because so little is known about risk-protective factors (35), it would be rash to conclude that potentially protective factors such as positive therapeutic change or community support play no role in how mentally ill offenders fare after release from prison.
Our finding that mentally ill offenders rarely commit serious violent offenses deserves special emphasis. Restricted public agency budgets and habits of public discourse that emphasize the fear of crime, abetted by the occasional spectacular crime by a person with mental illness, may lead well-meaning advocates to argue for more extensive social services mainly on the grounds of public safety—that is, unless better services are provided, mentally ill offenders will put the rest of society at risk. A hidden danger of this reasoning is that it presumes that mentally ill offenders are high-risk consumers. This supposition may only reinforce public fear and, ironically, discourage efforts to reach out to mentally ill offenders and keep them engaged in community mental health and other social services. This report provides strong evidence that even mentally ill offenders who have been convicted of serious felonies resulting in prison sentences rarely commit serious violent crimes after release.
Another important discovery is the pattern of arrests for minor offenses that often presage a major felony. Such harbinger arrests may result in jail time, because mentally ill offenders often cannot post bail and gain release. Although jail time is not generally regarded as conducive to high-quality mental health treatment, it may nevertheless constitute a good opportunity for timely, strategic mental health intervention or diversion to the mental health system, especially for mentally ill offenders who have been arrested on less serious criminal charges.
Persons with mental illness who are incarcerated are often without housing, family, or friends. Stable connections with treatment providers may also be uncommon. For many, life on the street or in shelters is punctuated by arrests and jail stays, and imprisonment is little more than an extended break in this pattern. The vast majority of their offenses, such as public intoxication, trespassing, possession of drugs, and aggressive panhandling, are more a reflection of a marginal urban existence than a violation of the basic rights of other citizens. In the end, the principal victims of mentally ill offenders are the mentally ill offenders themselves. This by itself is sufficient reason for committing more resources to supporting and treating mentally ill offenders while they are incarcerated and when they leave jails or prisons.
Acknowledgments
This study was funded by the Mental Health Division of the Washington Department of Social and Health Services and by the Department of Corrections. The authors are indebted to Ron Jemelka and Bruce Gage for their leadership and technical assistance in early phases of the study. The authors thank Polly Phipps, Laura Harmon, Robert Barnoski, Peggy Smith, Jutta Duncan, Diann Hare, Bruce Stegner, Fred Fiedler, and Katrina Moore for supplying, compiling, or providing access to data.
Dr. Lovell is affiliated with the department of psychosocial and community health at the University of Washington in Seattle. Dr. Gagliardi and Dr. Peterson are affiliated with the department of psychiatry and behavioral sciences at the University of Washington and the Washington Institute for Mental Illness Research and Training in Tacoma. Send correspondence to Dr. Lovell, University of Washington, Box 357263, Seattle, Washington 98195-7263 (e-mail, [email protected]).
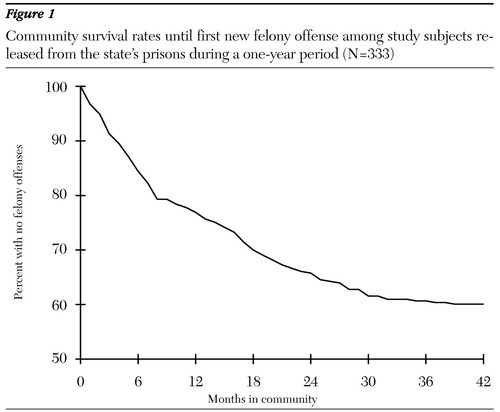
Figure 1. Community survival rates until first new felony offense among study subjects released from the state's prisons during a one-year period (N=333)
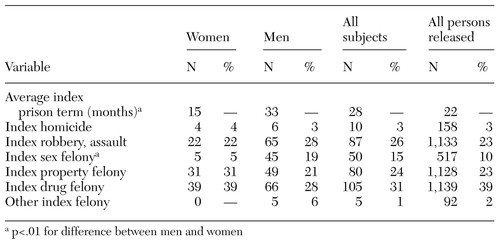 |
Table 1. Index offenses and prison terms of male (N=236) and female (N=101) subjects and a comparison group of all persons released (N=4,967) from the state's prisons during a one-year period
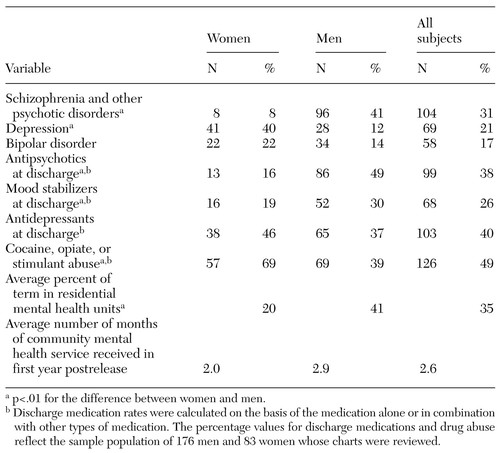 |
Table 2. Clinical characteristics of male and female subjects and a comparison group of all persons released from the state's prisons during a one-year period
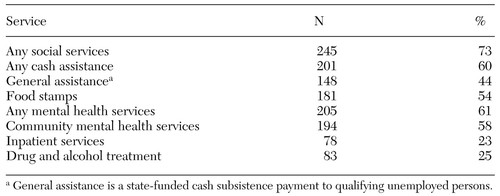 |
Table 3. Types of postrelease social services received during the follow-up period by study subjects released from the state's prisons during a one-year period
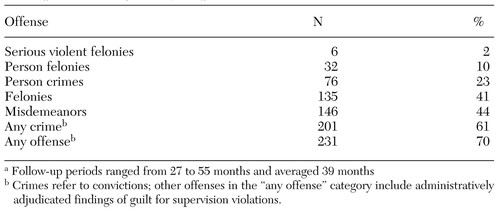 |
Table 4. Measures of recidivism during follow-up among study subjects released from the state's prisons during a one-year period (N=333)a
a Follow-up periods ranged from 27 to 55 months and averaged 39 months
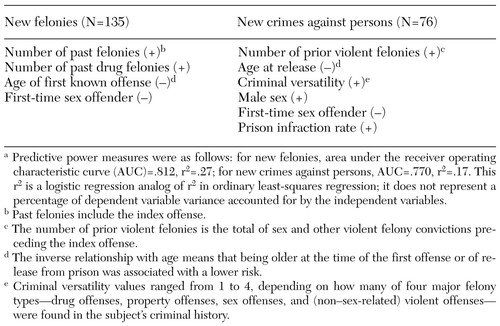 |
Table 5. Risk factors for new felonies and new crimes against persons among study subjects after release from prison, by whether the relationship was positive (+) or negative (−)a
a Predictive power measures were as follows: for new felonies, area under the receiver operating characteristic curve (AUC)=.812, r2=.27; for new crimes against persons, AUC=.770, r2=.17. This r2 is a logistic regression analog of r2 in ordinary least-squares regression; it does not represent a percentage of dependent variable variance accounted for by the independent variables.
1. Steadman HJ, Monahan J, Hartstone E, et al: Mentally disordered offenders: a national survey of patients and facilities. Law and Human Behavior 6:31-38, 1982Crossref, Google Scholar
2. Monahan J, Steadman HJ: Mentally Disordered Offenders. New York, Plenum, 1983Google Scholar
3. Bureau of Justice Statistics Special Report: Mental Health and Treatment of Inmates and Probationers. Monograph NCJ 174463. Washington, DC, US Department of Justice, Office of Justice Programs, 1999Google Scholar
4. Bureau of Justice Statistics Report: Correctional Populations in the United States, 1997. Monograph NCJ 177613). Washington, DC, US Department of Justice, Office of Justice Programs, 2000Google Scholar
5. Wiederanders MR, Choate PA: Beyond recidivism: measuring community adjustments of conditionally released insanity acquittees. Psychological Assessment 6:61-66, 1994Crossref, Google Scholar
6. Wiederanders MR: Recidivism of disordered offenders who were conditionally vs unconditionally released. Behavioral Sciences and the Law 10:141-148, 1992Crossref, Google Scholar
7. Rice MF, Harris GT: A comparison of criminal recidivism and among schizophrenic and non-schizophrenic offenders. International Journal of Law and Psychiatry 15:397-408, 1992Crossref, Medline, Google Scholar
8. Russo G: Follow-up of 91 mentally ill criminals discharged from the maximum security hospital in Barcelona PG. International Journal of Law and Psychiatry 17:279-301, 1994Crossref, Medline, Google Scholar
9. Harris VL: Insanity acquittees and re-arrest: the past 24 years. Journal of the American Academy of Psychiatry and Law 28:225-231, 2000Medline, Google Scholar
10. Steadman HJ, Mulvey EP, Monahan J, et al: Violence by people discharged from acute psychiatric facilities and by others in the same neighborhoods. Archives of General Psychiatry 55:393-401, 1998Crossref, Medline, Google Scholar
11. Feder L: A comparison of the community adjustment of mentally ill offenders with those from general population: an 18-month follow-up. Law and Human Behavior 15:477-493, 1991Crossref, Google Scholar
12. Feder L: A profile of mentally ill offenders and their adjustment in the community. Journal of Psychiatry and the Law 19:79-98, 1991Crossref, Google Scholar
13. Jacoby JE, Kozie-Peak B: The benefits of social support for mentally ill offenders: prison-to-community transitions. Behavioral Sciences and the Law 15:483-501, 1997Crossref, Medline, Google Scholar
14. Wilson D, Tien G, Eaves D: Increasing community tenure of mentally disordered offenders: an assertive case management program. International Journal of Law and Psychiatry 18:61-69, 1995Crossref, Medline, Google Scholar
15. Wolff G, Pathare S, Craig T, et al: Community attitudes to mental illness. British Journal of Psychiatry 168:183-190, 1996Crossref, Medline, Google Scholar
16. Wolff G, Pathare S, Craig T, et al: Community knowledge of mental illness and reaction to mentally ill people. British Journal of Psychiatry 168:191-198, 1996Crossref, Medline, Google Scholar
17. Wolff G, Pathare S, Craig T, et al: Public education for community care: a new approach. British Journal of Psychiatry 168:441-447, 1996Crossref, Medline, Google Scholar
18. Lamb HR, Weinberger LE: Persons with severe mental illness in jails and prisons: a review. Psychiatric Services 49:483-492, 1998Link, Google Scholar
19. Lamb RH, Weinberger LE, Gross BH: Community treatment of severely mentally ill offenders under the jurisdiction of the criminal justice system: a review. Psychiatric Services 50:907-913, 1999Link, Google Scholar
20. Swanson JW, Morrissey JP, Goldstrom I, et al: Funding, expenditures, and staffing of mental health services in state adult correctional facilities: United States, 1988. Mental Health Statistical Note no 208. Washington, DC, US Department of Health and Human Services, 1993Google Scholar
21. Client Characteristics, Population Movement, and Custody Report for Fiscal Year 1998. Olympia, Wash, Department of Corrections, Planning and Research Section, 1998Google Scholar
22. Henderson D, Schaeffer J, Brown L: Gender-appropriate mental health services for incarcerated women: issues and challenges. Family and Community Health 21:42-53, 1998Crossref, Google Scholar
23. Baskin D, Sommers I, Tessler R, et al: Role incongruence and gender variation in the provision of prison mental health services. Journal of Health and Social Behavior 30:305-314, 1989Crossref, Medline, Google Scholar
24. Toch H, Adams K, Grant D: Coping: Maladaptation in Prisons. New Brunswick, NJ, Transaction Publishers, 1989Google Scholar
25. Link B, Andrews H, Cullen F: The violent and illegal behavior of mental patients reconsidered. American Sociological Review 57:277-292, 1992Google Scholar
26. Monahan J: Mental disorder and violent behavior: perceptions and evidence. American Psychologist 47:511-521, 1992Crossref, Medline, Google Scholar
27. Rice M, Harris G: A comparison of criminal recidivism among schizophrenic and nonschizophrenic offenders. International Journal of Law and Psychiatry 15:397-408, 1992Crossref, Medline, Google Scholar
28. Hodgins S (ed): Mental Disorder and Crime. Newbury Park, Calif, Sage, 1993Google Scholar
29. Link B, Stueve A: Psychotic symptoms and the violent/illegal behavior of mental patients compared to community controls, in Violence and Mental Disorder: Developments in Risk Assessment. Edited by Monahan J, Steadman H. Chicago, University of Chicago Press, 1994Google Scholar
30. Silver E, Mulvey EP, Monahan J: Assessing violence risk among discharged psychiatric patients: toward an ecological approach. Law and Human Behavior 23:237-255, 1999Crossref, Medline, Google Scholar
31. Swets J, Dawes RM, Monahan J: Psychological science can improve diagnostic decisions. Psychological Science in the Public Interest 1:1-26, 2000Crossref, Medline, Google Scholar
32. Rice ME, Harris GT: Violent recidivism: assessing predictive validity. Journal of Consulting and Clinical Psychology 63:737-748, 1995Crossref, Medline, Google Scholar
33. Douglas KS, Ogloff JRP, Grant I, et al: Assessing risk for violence among psychiatric patients: the HCR-20 violence risk scheme and the Psychopathy Checklist, Screening Version. Journal of Consulting and Clinical Psychology 67:917-930, 1999Crossref, Medline, Google Scholar
34. Steadman HJ, Silver E, Monahan J, et al: A classification tree approach to the development of actuarial violence risk assessment tools. Law and Human Behavior 24:83-100, 2000Crossref, Medline, Google Scholar
35. Rogers R: The uncritical acceptance of risk assessment in forensic practice. Law and Human Behavior 24:595-605, 2000Crossref, Medline, Google Scholar



