The Association Between Decreasing Length of Stay and Readmission Rate on a Psychogeriatric Unit
Abstract
OBJECTIVE: This study investigated whether there was an association between decreasing length of stay and readmission rate on a psychogeriatric unit. METHODS: Discharge summaries were reviewed for all 1,099 admissions to a university hospital psychogeriatric unit from January 1993 through December 1997. Data were collected for all 77 patients who were readmitted within 30 days of a previous discharge and for an equal number of randomly selected patients who were not readmitted. Data included length of stay, diagnosis, disposition, and demographic information. RESULTS: Mean length of stay decreased significantly over the five-year study period for patients who were readmitted and for those who were not readmitted. The mean length of stay for the index admission of readmitted patients decreased from 33.6 days to 9.5 days. The mean length of stay of patients who were not readmitted decreased from 27.5 days to 12.7 days. Over the same period, the readmission rate doubled, rising from 5.3 percent (seven patients) to 10.8 percent (30 patients), and the proportion of patients who were discharged to the geriatric day hospital increased significantly. CONCLUSIONS: Although it is difficult to demonstrate causality, these findings indicate a temporal association between decreasing length of stay and rate of readmission to a university hospital psychogeriatric unit.
The past decade has seen significant changes in the way inpatient mental health services are provided. With the advent of managed care, the development of new medications, and more intensive outpatient treatment programs, there is constant pressure to discharge patients from the hospital sooner. Inpatient care is the most expensive component of mental health services, so inpatient episodes are now typically brief and focused on managing crises and stabilizing symptoms. As a result, length of stay on psychiatric inpatient units around the country has progressively decreased. The American Hospital Association reports that the average stay in psychiatric hospitals declined from 75 days to 56 days between 1988 and 1992. Moreover, in the period from 1988 to 1994, length of stay for psychiatric patients in general hospitals declined from 12.1 to 9.6 days (1).
The large proportion of patients who are discharged after very short stays raises questions about quality of care and the possible impact of early discharge on readmission rates. Studies of the relationship between length of stay and readmission rates have had mixed results (2,3,4,5). One study looked at the relationship between length of stay and readmission rate for all patients admitted to a university-affiliated adult psychiatric inpatient unit between 1985 and 1992 and found that in a population of privately insured patients, drastically shortening hospital stays did not result in an overall increase in recidivism (2).
Similarly, another study found that reducing the average length of stay in an acute psychiatric unit from 25 days in 1988 to 16 days in 1994 did not increase the readmission rate (5). In contrast, other authors who looked at recidivism among patients with schizophrenia have expressed concern that short hospital stays may not provide adequate preparation for discharge and may be associated with higher readmission rates, because discharged patients are now sicker (3,4,6).
Hospital stays for acute psychiatric admissions tend to be longer among older patients, partly because of concomitant physical illness and placement problems (7). We are not aware of any recent studies exploring the relationship between length of stay and readmission rate exclusively in a psychogeriatric population. The objective of this retrospective study was to examine whether there was an association between decreasing length of stay and readmission rate on a psychogeriatric inpatient unit. This question is important not only because readmission increases suffering and costs but also because it is considered preventable.
Methods
Subjects
Data were collected retrospectively from the psychogeriatric inpatient unit at the University of Maryland Medical Center in Baltimore. The unit consists of 13 beds and for the most part serves an inner-city population. Referral sources and the proportion of admissions referred by each source are the medical center's emergency department (62 percent), private-practice psychiatrists (10 percent), the psychiatry consultation-liaison service (9 percent), nonpsychiatrist outpatient physicians (8 percent), and others (11 percent). Unlike most psychogeriatric units, in which the youngest patients are aged 60 years or older, the unit admits patients aged 50 years or older. The staff in the unit works closely with the geriatric day hospital, which is located on the same unit. Any patient who was admitted to the unit between 1993 and 1997 qualified for the study.
Procedure
Discharge summaries were reviewed for all admissions to the psychogeriatric unit from January 1993 through December 1997. Data were collected for all patients who were readmitted within 30 days of a previous discharge and for the same number of randomly selected patients who were not readmitted. If a patient was readmitted more than once, data from only the first readmission were included in the analysis; this was the case for 13 (14 percent) of the 90 readmissions, so a total of 77 readmitted patients were included in the analysis. The random sample of patients who were not readmitted was selected with use of the pseudo-random number generator and the random sample selection function of SPSS. Data included age, sex, admission and discharge dates, length of stay, disposition, and psychiatric diagnosis. Information about race was not available for all patients, so it was not included. Diagnoses were made by second-year psychiatric residents in collaboration with the attending psychiatrist. For this study, an index admission was defined as the admission preceding a readmission within 30 days of discharge.
We chose the 30-day readmission interval on the basis of measurements of readmission used in previous studies (2,3,5,8) and preliminary data showing that readmission within a six-month interval bore no relationship to length of stay. None of the readmitted patients or those in the comparison group were discharged against medical advice.
Data analysis
We used one-way analysis of variance with post hoc least-significant-difference tests to compare mean length of stay by year. Chi square analysis or Fisher's exact probability test was used to compare the two groups on diagnosis, sex, and disposition. We compared the mean length of stay and the mean age of the patients who were and were not readmitted by using Student's t test. Fisher's exact probability test was used to compare the proportion of readmitted patients in 1993 with that in 1997. Two-tailed probabilities were used for all tests except where specified for the Fisher's exact probability test. All analyses were performed with SPSS (8), VassarStats (9), or Statistical Power Analysis (10).
Results
The demographic and clinical characteristics of the 77 readmitted patients and the 77 randomly selected patients who were not readmitted are summarized in Table 1. The mean age of the readmitted patients was 64.3 years, significantly less than the 67.5 years for patients who were not readmitted. The two samples also differed significantly in type of diagnosis. The largest group of readmitted patients met criteria for a mood disorder, which included major depression, bipolar disorder, dysthymia, and other forms of depression. The next largest group of readmitted patients were diagnosed as having a psychotic disorder, which included schizophrenia, schizoaffective disorder, and other psychoses, and an organic brain disorder—either delirium or dementia secondary to various causes. By comparison, the patients who were not readmitted had more than double the rate of organic brain disorders and about 50 percent fewer psychotic disorders. For the five-year period, the mean length of stay for readmitted patients was about three days less than that for those who were not readmitted; however, this difference was not statistically significant.
Analyzed by year, data on length of stay and readmission revealed some interesting trends, as can be seen in Table 2. For readmitted patients, the mean length of stay for the index admission decreased significantly over the five years, from 33.6 days to 9.5 days, a decline of 72 percent. The mean length of stay for patients who were not readmitted also decreased significantly, from 27.5 days to 12.7 days, but the decline was less severe —54 percent. During the same period, the overall proportion of readmitted patients doubled, from 5 percent (seven patients) in 1993 to 11 percent (30 patients) in 1997. There was also a dramatic increase in the proportion of patients who were discharged to the geriatric day hospital over that period, from 10 percent to 47 percent (two-tailed Fisher's exact probability test, p=.003).
Discussion
Our findings show a temporal association between decreasing length of stay and rate of readmission to our university hospital psychogeriatric unit between 1993 and 1997. As the overall mean length of stay for all patients declined from 29.6 to 15.2 days, the readmission rate doubled, from 5 percent to 11 percent. This temporal association suggests—but does not prove—that the readmission rate doubled because length of stay declined. Over the same five years, the proportion of patients who were discharged to the geriatric day hospital more than quadrupled, which suggests a need for more intensive outpatient treatment. It is possible that readmission rates would have been higher if not for this more intensive outpatient treatment. It is also possible that the existence of the day hospital raised the inpatient treatment team's expectations that patients could tolerate shorter stays.
The trend toward shorter stays between 1993 and 1997 was probably in part a product of economic and administrative forces. Medicare began reimbursing day hospital programs in 1991 (11), making it possible to provide more intensive outpatient treatment to older patients. Meanwhile, greater internal and external review of the medical necessity of inpatient care meant that patients were discharged sooner and therefore needed the more intensive outpatient care of a day hospital to prevent relapse and readmission. Our findings indicate that discharging more patients to the geriatric day hospital did not prevent the readmission rate from increasing. As a group, the patients who were readmitted were actually more likely than those who were not readmitted to be discharged to the day hospital (40 percent compared with 29 percent), although this difference was not statistically significant.
Beyond the main focus of our research, which was to answer the question about the relationship between decreasing length of stay and readmission rate, our findings provide some insight into the characteristics of readmitted psychogeriatric inpatients. Although it can be argued that a three-day difference in length of stay is clinically significant for an individual patient, our finding of no statistically significant difference in the overall mean length of stay between patients who were readmitted and those who were not during the study period suggests that length of stay is not the only factor that determines whether a patient is readmitted.
Thus our findings are consistent with the explanation that other factors, including diagnosis, severity of illness, and disposition, in combination with length of stay determine whether a given patient is readmitted. The patients who were readmitted were significantly younger and, accordingly, had lower rates of organic brain disorders, such as dementia and delirium, and were less likely to be discharged to a nursing home. These findings suggest that elderly persons who have organic brain disorders and are therefore often incapable of independent living are less likely to be readmitted because they are discharged to supervised settings, such as nursing homes and assisted living facilities, where medication monitoring, behavioral interventions, and in-house psychiatric consultation are readily available to prevent relapse.
It is also possible that older patients had a higher rate of death within 30 days of discharge and therefore were not readmitted. Given that we do not have follow-up information on patients who were not readmitted, we cannot determine the extent to which mortality played a role in the rate of readmission of the older patients.
This study had several important limitations. First, we do not know whether any of the patients were readmitted to one of the other inpatient psychiatric units in the area within 30 days of discharge from our unit. Thus it is possible that we significantly underestimated the readmission rate and that some of the patients whom we included in the comparison group were actually readmitted to other hospitals. We considered that obtaining this information would be prohibitively laborious and time-consuming.
Second, the study sample was relatively small, which limited the power of our statistical analyses. For example, the difference of almost three days in overall mean length of stay for patients who were and those who were not readmitted would have reached statistical significance with a sample of 268 readmitted patients (alpha=.05, beta=.2, power=.8). Third, ours is a mostly middle- and lower-income, inner-city geriatric population. We must be careful when extrapolating these results to psychogeriatric inpatient units that serve different—and possibly more resourceful—populations.
Fourth, the age cutoff for the inpatient unit is 50 years, which is younger than that for most other psychogeriatric units. Fifth, the data were retrospective, and the scope of the study was confined to the type of data available from the patients' discharge forms. For example, we could not determine the relationship between readmission rate and severity of illness, because we did not have a measure of severity. Thus this study can serve as a pilot study for a more extensive, prospective study that would include ratings of severity of illness at admission and discharge as well as follow-up of patients after discharge to determine whether they were admitted to other area hospitals.
Conclusions
This retrospective pilot study found a temporal association between decreasing length of stay and rate of readmission to a university hospital psychogeriatric inpatient unit between 1993 and 1997, which suggests that, at least in our population, there is a limit past which reducing length of stay may not be prudent. A more extensive, prospective study would help determine the extent to which this temporal association reflected a causal relationship between decreasing length of stay and readmission rate and help better characterize patients who are at the highest risk of readmission.
Acknowledgments
The authors thank Anthony F. Lehman, M.D., and Jeanne Geiger Brown, Ph.D., R.N., for their comments.
The authors are affiliated with the department of psychiatry of the University of Maryland in Baltimore. Send correspondence to Dr. Regenold at the Department of Psychiatry, University of Maryland Medical Center, Box 351, Room S12A09, 22 South Greene Street, Baltimore, Maryland 21201 (e-mail, [email protected]). A version of this paper was presented as a poster at the annual meeting of the American Psychiatric Association held May 15-20, 1999, in Washington, D.C.
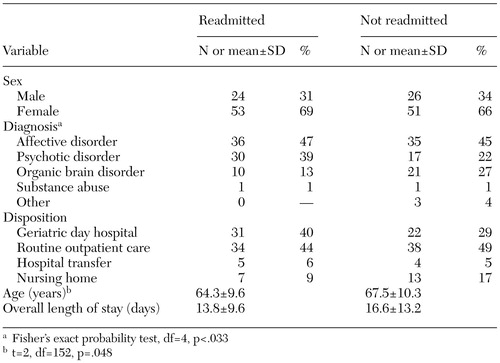 |
Table 1. Demographic and clinical characteristics of 77 patients who were readmitted to a psychogeriatric unit and a random sample of 77 who were not readmitted
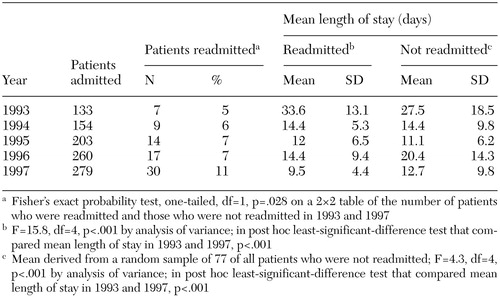 |
Table 2. Readmission rates and lengths of stay for a university hospital psychogeriatric inpatient unit, 1993 to 1997
1. Mechanic D, McAlpine DD, Olfson M: Changing patterns of psychiatric inpatient care in the United States, 1988-1994. Archives of General Psychiatry 55:785-791, 1998Crossref, Medline, Google Scholar
2. Thomas MR, Rosenberg SA, Giese AA, et al: Shortening length of stay without increasing recidivism on a university-affiliated inpatient unit. Psychiatric Services 47:996-998, 1996Link, Google Scholar
3. Appleby L, Desai PN, Luchins DJ, et al: Length of stay and recidivism in schizophrenia: a study of public psychiatric hospital patients. American Journal of Psychiatry 150:72-76, 1993Link, Google Scholar
4. Appleby L, Luchins DJ, Desai PN, et al: Length of inpatient stay and recidivism among patients with schizophrenia. Psychiatric Services 47:985-990, 1996Link, Google Scholar
5. Edward-Chandran T, Malcolm DE, Bowen RC: Reduction of length of stay in an acute care psychiatric unit. Canadian Journal of Psychiatry 41:49-51, 1996Crossref, Medline, Google Scholar
6. Lieberman PB, Wiitala SA, Elliott B, et al: Decreasing length of stay: are there effects on outcomes of psychiatric hospitalization? American Journal of Psychiatry 155:905-909, 1998Google Scholar
7. Draper B, Luscombe G: Quantification of factors contributing to length of stay in an acute psychogeriatric ward. International Journal of Geriatric Psychiatry 13:1-7, 1998Crossref, Medline, Google Scholar
8. SPSS Base System Syntax Reference Guide, release 6.0. Chicago, SPSS, 1993Google Scholar
9. Lowry R: VassarStats, 2001. Available at http://vassun.vassar.edu/~lowry/vassarstats. htmGoogle Scholar
10. Borenstein M, Cohen J: Statistical Power Analysis software. Hillsdale, NJ, Erlbaum, 1988Google Scholar
11. Federal reviews hit partial hospitalization's bottom line. Mental Health Weekly 4:2, 1994Google Scholar



