Ward Crowding and Incidents of Violence on an Acute Psychiatric Inpatient Unit
Abstract
OBJECTIVE: Violence in psychiatric wards is common, and it is on the rise. This study examined the relationship between ward occupancy level and staff-to-patient ratio and incidents of aggressive behavior, both physical and verbal, on an acute inpatient unit in rural New Zealand. METHODS: Logistic regression was used to analyze data collected from the ward's log of adverse incidents and the ward census over a 12-month period. A physical incident was defined as an unwelcome physical contact or willful damage to property. Incidents of self-harm were excluded. Verbal aggression was any threat of physical or sexual harm. RESULTS: Among 381 admissions during the study period, 58 incidents were recorded—25 incidents of verbal aggression and 33 incidents of physical violence. Logistic regression demonstrated that the occupancy level was positively associated with the occurrence of any type of violent incident. The average occupancy level when an incident occurred was 77 percent, compared with 69 percent when no incidents occurred. The average occupancy level was significantly higher when verbal incidents occurred (80 percent) than when physical incidents occurred (70 percent). No association was found between violence and staff-to-patient ratio. Incidents were significantly more likely to occur during the afternoon shifts (3 p.m. to 11 p.m.). CONCLUSIONS: Crowding was found to be significantly associated with aggressive incidents, and in particular with verbal aggression.
Violence on psychiatric wards is a growing concern because of its prevalence (1,2) and the increasing number of incidents (3,4,5,6). The problem is so severe that many mental health professionals expect to encounter violence in their work with psychiatric patients (7).
The factors identified as leading to violence on acute inpatient units can be broadly divided into four categories: patient, staff, environment, and staff-patient dynamics.
Patient factors include gender (8,9,10,11), age (5,8,9,12), history of violence (13,14), social and economic status (15,16), and diagnosis, especially schizophrenia (6,8,9,12,14,15,16,17,18,19). Staff factors include inexperience or lack of training (5), lack of a clear role (20), and low staff-to-patient ratio (21,22). Environmental factors are the time of day or day of the week (5,8,15,18,22,23,24), location within the unit (3,22,24), patient overcrowding (1,21,25,26,27), an untherapeutic ward environment (28,29), and ward turmoil (20,30). Factors related to staff-patient dynamics include lack of control by the staff (21), few or poorly organized activities (3,20); uncertainty, confusion, or fear about the staff-patient relationship (20), and poor staff-patient interaction (31,32).
Given the global trend toward reducing the number of inpatient beds (27,30,33,34) and problems with staff recruitment and retention (21,35), many mental health service providers are especially concerned about crowding and staff-to-patient ratios on psychiatric units.
Reported occupancy rates in excess of 100 percent—as happens when the beds of patients on leave from the ward are used for acute admissions—have resulted in pressure to discharge patients prematurely, leading to additional stress on both patients and staff (36,37). Lack of personal space and the disruption of everyday activities caused by crowding may exacerbate stress, which may in turn lead to violent incidents (38). In a prospective study, Palmstierna and colleagues (26) found that crowding on an acute psychiatric ward increased the likelihood of aggressive behavior among patients with schizophrenia or schizophreniform disorder; however, the authors cautioned that despite some support for a relationship between violence and crowding, "conclusions regarding the clinical importance of overcrowding remain debatable."
Owen and colleagues (39) examined patient, staff, and environmental factors and reported a significant positive relationship between large numbers of patients and violent incidents. On the other hand, an early study by Kalogerakis (40) found that most violent incidents occurred when ward densities were at their lowest. Lanza and colleagues (22) found no relationship between the proportion of occupied beds on a unit and the number of assaults, and a recent study by Hardie (41) concluded that an increase in patient density was not associated with an increase in violent incidents.
The relationship between the staff-to-patient ratio and number of assaults was studied prospectively by Lanza and colleagues (22), who offered some preliminary evidence supporting an inverse relationship between number of staff members and frequency of assaults. However, Kalogerakis (40) found that most violent incidents occurred when staff-to-patient ratios were high, and Depp (23) reported a similar trend. In a retrospective review, Myers and Dunner (42) concluded that the presence of more nursing staff did not necessarily lead to fewer assaults, and they speculated that other factors, such as the staff's commitment to their patients and their ability to manage such incidents, might be more important.
Owen and colleagues (39) actually found a positive relationship between violence and number of staff members. Violent patient behavior was further linked with female staff and staff members who did not have psychiatric or aggression training.
Patient-to-patient interactions, a known factor associated with ward violence, may also be intensified in crowded situations (43,44).
Definitive conclusions about the factors involved in violent patient behavior cannot be drawn from the studies cited above. Most of these studies looked broadly at risk factors for violence; issues of crowding and staff-to-patient ratios were either ignored or emerged as secondary findings. The definitions of violence were not consistent, and the distinction between physical and verbal aggression was often overlooked. Our study was designed specifically to examine the relationship between ward occupancy levels and staff-to-patient ratios and violent incidents, either physical or verbal, on an acute psychiatric ward. We hypothesized that an increase in the number of violent incidents would be positively associated with a low staff-to-patient ratio and with a high ward occupancy.
Methods
Our study was conducted at Rotorua Hospital in Rotorua, New Zealand. The hospital has one acute adult inpatient psychiatric unit with 14 general beds and two intensive-care beds. The total built-up area of the psychiatric unit is 720 square meters. Each patient has a separate room measuring nine square meters. The communal area includes a lounge, dining hall, kitchen, courtyard, activity room, and library.
Patients are admitted to the unit on a voluntary and involuntary basis. Criteria for admission include any acute psychiatric condition for which community interventions have failed, with or without risk to self or others. No child or forensic admissions are accepted. The unit caters to a catchment area population of 110,000 from two towns—Rotorua and Taupo—and the neighboring rural areas of New Zealand.
Typically when all 14 beds are occupied, six registered staff nurses work on the morning shift (7 a.m. to 3 p.m.), five on the afternoon shift (3 p.m. to 11 p.m.), and two on the night shift (11 p.m. to 7 a.m.). A maximum of two nurses or two nursing aides from an agency may be called in if regular nurses are not available or the acuity level is high; agency nurses and nursing aides may not have psychiatric training. In addition, two third-year nursing students are placed for eight weeks in a supernumerary capacity on the morning and afternoon shifts three times a year.
Data were extracted retrospectively from the unit's census records for 12 months, from December 1997 through November 1998. Data on the total number of patients with a current ward admission, the number on leave from the ward, and the number actually present on the ward are routinely collected every day on the unit. For this study, we used the data on the number of patients actually present on the ward for the occupancy and staff-to-patient ratio analyses. The corresponding number of nursing staff directly involved in patient care was noted for each of the eight-hour shifts. Hospital records of all admissions to the inpatient unit for the 12-month study period were obtained, including each patient's sex, age, diagnosis, and number of admissions.
The log of ward incidents, which contains descriptive accounts of all violent incidents that occur on the unit, was reviewed. We defined a physical incident as any unwelcome physical contact initiated by a patient against another patient or staff member or willful damage to property. Incidents of self-harm were not included. We defined verbal aggression as any threat—with or without a weapon—of physical or sexual harm. All logged incidents that fit our definitions of physical or verbal aggression were included in our study. Of 87 logged incidents, 29 did not fit our definitions or did not contain adequate information and were not included. The type, time, and location of each incident and the persons involved were recorded.
The census data and the data on violent incidents were merged and analyzed using logistic regression to model the relationship between explanatory variables and the binary outcome variables. In logistic regression the assumption is that the errors have a binomial distribution rather than a normal distribution as in linear regression. The unit of analysis was the nursing shift. Occupancy was calculated as the number of patients on the ward during the shift divided by the number of available beds, expressed as a percentage.
Logistic regressions were performed to determine whether frequency of incidents or type of incident was associated with ward occupancy, staff-to-patient ratio, shift time, or day of the week.
Results
During the 12-month study period, 268 patients were admitted to the unit a total of 381 times; 192 patients had one admission, 55 had two admissions, 12 had three admissions, six had four admissions, and three had five or more admissions. Women accounted for 55 percent of admissions. The mean±SD age of admitted patients was 34±12.5 years, with a median age of 32 years and a range of 12 to 84 years. The mean±SD duration of admission was 10.8±16 days, with a median of seven days and a range of one to 124 days. The majority of patients were diagnosed as having psychotic disorders, including drug-induced psychoses, schizophrenia or schizoaffective disorder, depression, bipolar disorder, and adjustment disorder.
A total of 58 incidents were recorded during the one-year study period: 25 incidents of verbal aggression and 33 incidents of physical violence.
The study period contained 1,092 shifts. One incident of some type occurred on 54 shifts, and four shifts had more than one incident. Twenty-four verbal incidents and 32 physical incidents occurred during the morning and afternoon shifts. Night shifts were excluded from the second type of analysis because only two incidents, one verbal and one physical, were reported. The characteristics of the incidents, the victims, and the perpetrators are summarized in Table 1.
Ward occupancy was found to be related to whether or not an incident of either type occurred (χ2=7.9, df=1, p=.005). The average occupancy when an incident occurred was 77 percent, compared with 69 percent at other times. Occupancy rate was also found to be associated with the type of incident (χ2=8.5, df=1, p=.003); the occupancy rate was higher when verbal incidents occurred (80 percent) than when physical incidents occurred (70 percent).
Shift time was found to be related to whether or not an incident occurred (χ2=12.3, df=2, p=.002). Incidents occurred on 29 afternoon shifts (8 percent), compared with 23 morning shifts (6.3 percent) and two night shifts (.6 percent). Shift time was not significantly associated with type of incident, and the day of the week was not associated with whether incidents occurred. No significant associations were found between staff-to-patient ratios and either type or occurrence of incidents.
Generalized additive models (45) were used to examine whether the relationship between occupancy and the probability of a violent episode was linear. These models are nonparametric regressions that allow the data to determine the shape of the relationship between binary outcomes and independent continuous variables. No significant difference was found between the fit of the model with occupancy as a linear term compared with a smooth term. Hence occupancy was fitted as a linear term in the logistic model.
Discussion
Several studies have reported an association between crowding on acute psychiatric units and incidents of violence (26,39), but none have reported on the association between crowding and type of incident, that is, physical violence or verbal aggression. The findings of our study suggest that crowding is significantly associated with violent incidents, and in particular with verbal aggression.
It is difficult to offer any definitive explanation for the association between violence and crowding. Stress has been proposed as an explanation in a number of animal models (46,47) and studies of urban settings (48,49,50). Admission to a psychiatric unit is itself stressful for most patients. Crowding can worsen the effect through intrusion in body buffer zones (51,52), interference and interruptions from other patients and staff, and frustration from forced socialization in a confined space (49). Friis (28) has proposed that different types of patients need different ward environments. However, global reductions of inpatient beds may lead to the crowding of patients who have a variety of diagnoses, making the ward environment countertherapeutic (36,37).
From a strictly phylogenetic point of view, violence has been proposed as an instinctive function that serves to disperse animals over a wide area in order to conserve food resources (53). Violence may therefore be seen as a natural reaction to crowding. It has also been postulated that most fights "are no more than trials of strength followed by disengagement and rapid withdrawal by the weaker" (54), and that death and serious injury are avoided through ritualized threat and submission gestures (55). Anthropological studies have suggested that our primitive forebears did not desire serious or continuous combat with their neighbors (56).
We propose that the stress of admission to a psychiatric unit is more likely to trigger primitive patterns of aggression in human beings for the purposes of self-preservation or trials of strength, as opposed to more severe fights that may be intended for destruction. However, a distinction must be made between the aggression caused by minor deviations of healthy, adaptive human behavior and that driven by psychotic processes. The latter may have a weaker association with the use of aggression for self-preservation.
The effect of staff-to-patient ratio on aggressive incidents is controversial, with studies demonstrating a relationship between violence and both low (22) and high (23,39,40) ratios. Our study found no association between staff-to-patient ratio and the occurrence of violent incidents.
In our study, incidents were most likely to occur during the afternoon shifts, which run from 3 p.m. to 11 p.m. Aggressive incidents may occur more often during this period because of the lack of structured interaction and socialization such as ward outings, therapeutic groups, and interviews (3,6,15). Furthermore, this period would be more likely to be unsupervised, and the effects of morning medication could be waning.
The study of violence in psychiatric wards presents several problems. The underreporting of violence, the reporting of only incidents of a serious or repetitive nature, and inadequate documentation make it difficult to draw definitive conclusions (3,5,12,42). Lion and colleagues (57) have suggested that the number of unreported assaults may exceed that of reported assaults by a factor of five. Even prospective studies of ward violence have encountered problems with underreporting (32,39). Furthermore, results may be contaminated because patients and staff may become aware that they are being studied and consequently alter their behavior. Haller and Deluty (1) have suggested that most incidents are of a minor nature, and therefore reporting them was perceived as a time-consuming and unnecessary exercise; furthermore, a fear of "accusations of suboptimal care" made the problem worse.
In this study, data were drawn solely from the documentation of incidents by staff, who were already busy with patient care and paperwork. We believe that underreporting affected the number of incidents included in this study. A total number of 58 incidents—about one a week on average—would appear to be low. However, a sizable number of reported incidents were not included in our study because they did not fit our definition of an act of verbal aggression or physical violence.
The difference between the reported number of verbal incidents (25, or 43 percent) and physical incidents (33, or 57 percent) was not significant. Verbal aggression may have been reported less frequently because it can be easily missed or simply disregarded. Using structured instruments such as the Overt Aggression Scale (58) or the Staff Observation Aggression Scale (59) can minimize this underreporting. Because of the retrospective nature of our study, we were unable to use such instruments. An additional review of clinical notes may uncover incidents that were missed in the log review.
Prospective studies may further improve the reliability of the reported number of violent incidents. Such studies may also be able to collect additional data related to staffing variables and acuity levels of the ward, which may be associated with the incidence of aggression. Staffing variables may include, for example, length of experience, gender, and training in control and restraint procedures. Again, because of the retrospective nature of our study, we were unable to collect such information with any degree of accuracy. Further studies with larger samples are needed, particularly studies that investigate whether even a small increase in the number of patients on a ward influences the perception of crowding.
A lack of consensus on the definition of violence has been repeatedly reported as a major problem in studies of this subject. We attempted to avoid this problem by standardizing the definition of aggression. By adopting an operationalized definition of violence and extracting data from a descriptive log, we attempted to minimize the difficulties related to the quality of documentation of violence reported in other retrospective studies.
One issue not investigated in this study was placing patients on leave from the unit when their beds were needed for acute admissions. These patients return for regular reviews and stay for some time, driving official occupancy rates over 100 percent and further crowding an already full unit. It is difficult to study what effect, if any, this practice may have on violent incidents on the unit.
Conclusions
Our study suggests that crowding on an acute psychiatric unit is associated with aggressive incidents of a mostly verbal nature, and particularly during the afternoon shifts. Further prospective studies are needed to confirm these findings. Providers and planners of mental health services need to be constantly aware of the association between crowding and aggressive incidents. In future studies it may be worth examining whether dispersing patients, either by placing some on leave or by engaging them in activities off the unit, reduces the occurrence of aggressive incidents.
Acknowledgments
The authors thank Frances Ellery for providing some of the data on patient admissions and Rhea Liang, M.B.Ch.B., William Hell, M.B.Ch.B., and Thomas Dickey, M.D., for their comments.
Dr. Ng, Dr. Kumar, and Ms. Ranclaud are associated with the department of psychiatry at Rotorua Hospital in Rotorua, New Zealand. Ms. Robinson is with the department of community medicine at the Auckland School of Medicine in Auckland, New Zealand. Address correspondence to Dr. Kumar, Rotorua Hospital, corner Arawa and Ranolf Streets, Private Bag 3023, Rotorua, New Zealand (e-mail, [email protected]).
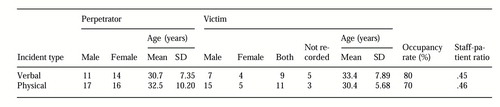 |
Table 1. Number and characteristics of incidents of verbal aggression and physical violence on an acute inpatient psychiatric ward
1. Haller RM, Deluty RH: Assaults on staff by psychiatric inpatients: a critical review. British Journal of Psychiatry 152:174-179, 1988Crossref, Medline, Google Scholar
2. Hubschmidt T: The prosecution of violent psychiatric inpatients: one respectable intervention. Psychiatrische Praxis 23:26-28, 1996Medline, Google Scholar
3. Drinkwater J: Violence in psychiatric hospitals, in Developments in the Study of Clinical Behavior, vol 2: Violence. Edited by Feldman P. Chichester, Wiley, 1982Google Scholar
4. Haffke EA, Reid WH: Violence against mental health personnel in Nebraska, in Assaults Within Psychiatric Facilities. Edited by Lion JR, Reid WH. New York, Grune & Stratton, 1983Google Scholar
5. Hodgkinson PE, Mclvor L, Phillips M: Patient assaults on staff in a psychiatric hospital: a two-year retrospective study. Medicine, Science, and Law 25:288-294, 1985Crossref, Medline, Google Scholar
6. Rice ME, Harris GT, Varney GW, et al: Violence in Institutions. Toronto, Hogrefe & Huber, 1989Google Scholar
7. Poster EC: A multinational study of psychiatric nursing staffs' beliefs and concerns about work safety and patient assault. Archives of Psychiatric Nursing 10:365- 373, 1996Crossref, Medline, Google Scholar
8. Fottrell E: A study of violent behaviour among patients in psychiatric hospitals. British Journal of Psychiatry 136:216-221, 1980Crossref, Medline, Google Scholar
9. Pearson M, Wilmot E, Padi M: A study of violent behaviour among inpatients in a psychiatric hospital. British Journal of Psychiatry 149:232-235, 1986Crossref, Medline, Google Scholar
10. Larkin E, Murtagh S, Jones S: A preliminary study of violent incidents in a special hospital (Rampton). British Journal of Psychiatry 153:226-231, 1988Crossref, Medline, Google Scholar
11. Lee HK, Villar O, Juthani N, et al: Characteristics and behavior of patients involved in psychiatric ward incidents. Hospital and Community Psychiatry 40:1295-1297, 1989Abstract, Google Scholar
12. Tardiff K: A survey of assault by chronic patients in a state hospital, in Assaults Within Psychiatric Facilities. Edited by Lion JR, Reid WH. New York, Grune & Stratton, 1983Google Scholar
13. Convit A, Jaeger J, Lin SP, et al: Predicting assaultiveness in psychiatric inpatients: a pilot study. Hospital and Community Psychiatry 39:429-434, 1988Abstract, Google Scholar
14. Blomhoff S, Seim S, Friis S: Can prediction of violence among psychiatric inpatients be improved? Hospital and Community Psychiatry 41:771-775, 1990Google Scholar
15. Edwards JG, Jones D, Reid WH, et al: Physical assaults in a psychiatric unit of a general hospital. American Journal of Psychiatry 145:1568-1571, 1988Link, Google Scholar
16. Estroff SE, Zimmer C, Lachicotte WS, et al: The influence of social networks and social support on violence by persons with serious mental illness. Hospital and Community Psychiatry 45:669-678, 1994Abstract, Google Scholar
17. Craig TJ: An epidemiologic study of problems associated with violence among psychiatric inpatients. American Journal of Psychiatry 139:1262-1266, 1982Link, Google Scholar
18. Cooper AJ, Mendonca JD: A prospective study of patient assaults on nurses in a provincial psychiatric hospital in Canada. Acta Psychiatrica Scandinavica 84:163-166, 1991Crossref, Medline, Google Scholar
19. Cooper SJ, Browne FW, McClean KJ, et al: Aggressive behavior in a psychiatric observation ward. Acta Psychiatrica Scandinavica 68:386-393, 1983Crossref, Medline, Google Scholar
20. Katz P, Kirkland FR: Violence and social structure on mental hospital wards. Psychiatry 53:262-277, 1990Crossref, Medline, Google Scholar
21. Lanza ML: The reactions of nursing staff to physical assault by a patient. Hospital and Community Psychiatry 34:44-47, 1983Abstract, Google Scholar
22. Lanza ML, Kayne HL, Hicks CJ, et al: Environmental characteristics related to patient assault. Issues in Mental Health Nursing 15:319-325, 1994Crossref, Medline, Google Scholar
23. Depp FC: Assaults in a public mental hospital, in Assaults Within Psychiatric Facilities. Edited by Lion JR, Reid WH. New York, Grune & Stratton, 1983Google Scholar
24. Dietz PE, Rada RT: Interpersonal violence in forensic facilities, in Assaults Within Psychiatric Facilities. Edited by Lion JR, Reid WH. New York, Grune & Stratton, 1983Google Scholar
25. Durivage A: Assaultive behaviour: before it happens. Canadian Journal of Psychiatry 34:393-397, 1989Crossref, Medline, Google Scholar
26. Palmstierna T, Huitfeldt B, Wistedt B: The relationship of crowding and aggressive behavior on a psychiatric intensive care unit. Hospital and Community Psychiatry 42:1237-1240, 1991Abstract, Google Scholar
27. MILMIS Project Group: Monitoring inner London mental illness services. Psychiatric Bulletin 19:276-280, 1995Crossref, Google Scholar
28. Friis S: Characteristics of a good ward environment. Acta Psychiatrica Scandinavica 74:469-473, 1986Crossref, Medline, Google Scholar
29. Atakan Z: Violence on psychiatric inpatient units: what can be done? Psychiatric Bulletin 19:593-596, 1995Google Scholar
30. Deahl M, Turner T: General psychiatry in no man's land. British Journal of Psychiatry 171:6-8, 1997Crossref, Medline, Google Scholar
31. Sheridan M, Henrion R, Robinson L, et al: Precipitants of violence in a psychiatric inpatient setting. Hospital and Community Psychiatry 41:776-780, 1990Abstract, Google Scholar
32. Cheung P, Scheitzer I, Tuckwell V, et al: A prospective study of assaults on staff by psychiatric patients. Medicine, Science, and Law 37:46-52, 1997Crossref, Medline, Google Scholar
33. Davis S: Violence by psychiatric inpatients: a review. Hospital and Community Psychiatry 42:585-590,1991Abstract, Google Scholar
34. Stroch DD: Crowding and the fiscal crisis. Hospital and Community Psychiatry 43:514, 1992Medline, Google Scholar
35. Bensley L, Nelson N, Kaufman J, et al: Patient and staff views of factors influencing assaults on psychiatric hospital employees. Issues in Mental Health Nursing 16:443- 446,1995Crossref, Google Scholar
36. Hollander D, Slater MS: Sorry, no beds: a problem for acute psychiatric admissions. Psychiatric Bulletin 18:532-534, 1994Crossref, Google Scholar
37. Watson JP: Too few beds. Psychiatric Bulletin 18:531, 1994Crossref, Google Scholar
38. Kumar S, Ng B, Robinson E: The crowded ward. Psychiatric Services 50:1499, 1999Link, Google Scholar
39. Owen C, Tarantello C, Jones M, et al: Violence and aggression in psychiatric units. Psychiatric Services 49:1452-1457, 1998Link, Google Scholar
40. Kalogerakis MG: The assaultive psychiatric patient. Psychiatric Quarterly 45:372-381, 1973Crossref, Google Scholar
41. Hardie TJ: Crowding and violent behaviour: the influence of patient density on violent and self-harming behavior at a medium secure unit. Medicine, Science, and Law 39:161-166, 1999Crossref, Medline, Google Scholar
42. Myers KM, Dunmer DL: Self- and other-directed violence on a closed acute-care ward. Psychiatric Quarterly 56:178-188, 1984Crossref, Medline, Google Scholar
43. Crowner M, Peric G, Stepcic F, et al: Psychiatric patients' explanations for assaults. Psychiatric Services 46:614-615, 1995Link, Google Scholar
44. Lanza ML, Kayne HL: Patient assault: a comparison of patient and staff perceptions. Issues in Mental Health Nursing 16:129-141, 1995Crossref, Medline, Google Scholar
45. Hastie TJ, Tibshirani RJ: Generalised Additive Models. London, Chapman & Hall, 1990Google Scholar
46. Freeman D: Aggression: instinct or symptom? Australian and New Zealand Journal of Psychiatry 5:66-77, 1971Crossref, Google Scholar
47. Boyce WT, O'Neill-Wagner P, Price CS, et al: Crowding stress and violent injuries among behaviorally inhibited rhesus macaques. Health Psychology 17:285-289, 1998Crossref, Medline, Google Scholar
48. Centerwall BS: Race, socioeconomic status, and domestic homicide. JAMA 273:1755- 1758, 1995Crossref, Medline, Google Scholar
49. Fuller TD, Edwards JN, Vorakitphokatorn S, et al: Chronic stress and psychological well-being: evidence from Thailand on household crowding. Social Science and Medicine 42:265-280, 1996Crossref, Medline, Google Scholar
50. Wallace D, Wallace R: Scales of geography, time, and population: the study of violence as a public health problem. American Journal of Public Health 88:1853-1858, 1988Crossref, Google Scholar
51. Kinzel AF: Body buffer zone in violent prisoners. American Journal of Psychiatry 127:59-64, 1970Link, Google Scholar
52. Hildreth AM, Derogatis LR, McCusker K: Body buffer zone and violence: a reassessment and confirmation. American Journal of Psychiatry 127:1641-1645, 1971Link, Google Scholar
53. Zegans LS: Towards a unified theory of human aggression. British Journal of Medical Psychology 44:355-365, 1971Crossref, Medline, Google Scholar
54. Lorenz K: Ritualized fighting, in The Natural History of Aggression. Edited by Carthy JD, Ebling FJ. New York, Academic Press, 1964Google Scholar
55. Roth M: Human violence as a viewed from the psychiatric clinic. American Journal of Psychiatry 128:1043-1056,1972Link, Google Scholar
56. Malinowski B: An anthropological analysis of war. American Journal of Sociology 46:521-550, 1941Crossref, Google Scholar
57. Lion JR, Snyder W, Merrill GL: Underreporting of assaults on staff in a state hospital. Hospital and Community Psychiatry 32:497-498, 1981Abstract, Google Scholar
58. Yudofsky SC, Silver JM, Jackson W, et al: The Overt Aggression Scale for the objective rating of verbal and physical aggression. American Journal of Psychiatry 143:35-39, 1986Link, Google Scholar
59. Palmstierna T, Wistedt B: Staff Observation Aggression Scale: presentation and evaluation. Acta Psychiatrica Scandinavica 76:657-663, 1987Crossref, Medline, Google Scholar



