Factors in the Use of Coercive Retention in Civil Commitment Evaluations in Psychiatric Emergency Services
Abstract
OBJECTIVE: The authors examined whether factors other than civil commitment criteria influence the involuntary retention of patients who are evaluated for civil commitment in psychiatric emergency services in California general hospitals. METHODS: Logistic regression analysis was used to determine whether admission criteria, institutional constraints, social biases, and procedural justice indicators contributed to the use of coercive retention in the evaluations of 583 patients in the psychiatric emergency services of nine California county general hospitals. RESULTS:Of the 583 patients, 109 (18.7 percent) were retained against their wishes. Clinicians relied primarily on admission criteria in making the decision to retain a patient, which suggests that patients were generally afforded procedural due process during the evaluation in the psychiatric emergency service. Staff workload was a possible factor in violations of due process. CONCLUSIONS: Psychiatric emergency services need additional resources to ensure procedural due process protection for patients who are being evaluated for civil commitment.
The general hospital psychiatric emergency service is the critical entry point to the mental health system and the setting where most civil commitment evaluations are completed and a considerable number of involuntary inpatient stays are approved. The involuntary hospitalization debate has moved from a narrow focus on formal legal procedures and status to a broader concern with actual coercive practices and the factors that lead to the inappropriate use of coercive powers in civil commitment (1). Evidence suggests that patients' dangerousness—the civil commitment criterion in California—is evaluated reliably in psychiatric emergency services, that dangerousness and mental disorder are related in the population served in psychiatric emergency services, and that patients who are retained are both dangerous and mentally disordered, not simply dangerous (2,3,4).
Civil commitment, which involves restraint by force of law, is an inherently coercive process that may abridge rights guaranteed by the Fourteenth Amendment. It is coercive in order to protect the individual and the community. The Fourteenth Amendment forbids any state to "deprive any person of life, liberty, or property without due process of law; nor [may it] deny . . . the equal protection of the laws."
The U.S. Supreme Court has repeatedly held that the civil commitment process is subject to the restraints of the Fourteenth Amendment. In Vitek v. Jones (5), the court held that "[w]e have recognized that for the ordinary citizen, commitment to a mental hospital produces a massive curtailment of liberty . . . and in consequence requires due process protection." This protection includes the requirement that a person be both mentally ill and dangerous before that person may be involuntarily committed and that the state produce at least clear and convincing evidence to prove that the person is both mentally ill and dangerous (6,7). Even negligent failure by hospital staff to comply with these guarantees and ascertain that an individual is constitutionally eligible for involuntary commitment may render a commitment illegal (8).
California's 1969 Lanterman-Petris-Short Act (9) is the model statute that codifies the dangerousness standard and procedural protections. Commitment procedures conducted before the implementation of this act required an assessment that the patient was in need of treatment. Investigations of these assessments found that "medical examinations and recommendations to the court were . . . perfunctory . . . and . . . based on vague criteria" (10). The Lanterman-Petris-Short Act placed severe restrictions on the discretion of evaluators in decisions about civil commitment (11) and set a standard for the nation. As Appelbaum (12) noted, "By the end of the 1970s every state either had changed its statute to restrict hospitalization to persons who were dangerous to themselves or others (including dangerous by virtue of 'grave disability,' defined as an inability to meet one's basic needs) or had reinterpreted its pre-existing statue in this way so as to 'save' it from being found unconstitutional." Only recently have some states, under increasing advocacy pressure, changed their laws to expand the discretionary powers of evaluating professionals in civil commitment decisions (13).
The California civil commitment process is like a funnel: evidence for retention is increasingly more demanding as the process moves toward the later stages, in which longer periods of detention may be ordered. As the process moves forward, different evaluators become involved, first credentialed laypersons, then psychiatric emergency service clinicians under the supervision of a psychiatrist, then administrative advocates, and finally a judge.
Initially the widest net is cast to ensure that individuals who meet the commitment standards can be brought to the initial evaluating facility. They may be brought to the psychiatric emergency service by the police, other designated professionals, or a physician—who may have limited psychiatric experience—or they may come on their own. Although people who come to the psychiatric emergency service may be kept there on an involuntary hold, this arrangement is temporary and occurs concurrently with a submission of an application for psychiatric evaluation (14,15).
The evaluation in the psychiatric emergency service is the first stage in the system where the patient's dangerousness and mental disturbance are independently assessed by trained and experienced professionals under psychiatric supervision and where a decision is made to release or retain the patient. Psychiatric emergency service clinicians can retain the patient on the basis of the facts of the case (exclusive of hearsay evidence) for 72 hours for observation and treatment with probable cause to believe that the patient meets the standard of being dangerous to self or others or is gravely disabled because of a mental disorder (14) in the absence of a less restrictive alternative (15). Usually the patient is committed to the hospital's own inpatient facility or to a private hospital inpatient facility in the county. Less frequently the patient is referred to a state facility. Retention beyond 72 hours requires additional administrative and judicial proceedings at which the evidence must be at least clear and convincing that the patient continues to meet the standard for involuntary detention.
Coercive actions in civil commitment evaluations and the factors likely to be involved in abridging a patient's due process or equal protection rights should be better understood. Assuming that all "involuntary" detentions are not necessarily unwanted (16), the attempt to study coercion in civil commitment evaluations in the psychiatric emergency service must focus on actions that the patient is not seeking. The coercive character of the evaluation disposition most clearly applies to the evaluation of patients who are not seeking hospitalization but who are involuntarily detained.
Given the serious abridgment of individual rights in coercive detentions, it seems necessary to ensure that such actions are taken on behalf of the individual and the community without the influence of inappropriate or confounding issues unrelated to the legally specified criteria for civil commitment. In making such a determination, we should consider three sets of issues. First, the increasing use of managed care strategies to control inpatient admissions has created institutional constraints on the admission evaluation process. These constraints are attributable to increasing workloads, cost decisions based on patients' insurance coverage, and the inadequacies of the work environment that increase practitioners' burden and may lead to inappropriate use of coercive powers. Second, procedural justice issues that have been of concern since the 1960s continue to be important in the contemporary psychiatric emergency service because of inappropriate advocacy, institutional processing, and inadequate patient participation in the evaluation decision process (16). Finally, race and gender social bias in decision making may lead to inappropriate use of coercive powers (17).
This study sought to determine whether factors other than the civil commitment criteria influence the disposition of patients seen in psychiatric emergency services, and, if so, whether these factors lead to unwanted and therefore coercive detentions. It also considers the relative importance of constraints, biases, and procedural justice issues in predicting psychiatric emergency service coercive dispositions.
Because civil commitment criteria are meant to provide a framework for justifying the limited circumstances that allow for the use of coercive intervention, ideally we should expect that no constraints, biases, or procedural justice issues should inappropriately influence the use of coercive intervention. Previous investigations have demonstrated the primacy of civil commitment criteria in admission decisions (18,19). This study moves beyond previous investigations by more accurately defining the coerced population as those who are not actually seeking retention and by specifying the constraints, biases, or procedural justice issues that may lead to a coercive disposition.
Methods
Sample and procedures
The evaluations of 583 patients in nine psychiatric emergency services in California—seven in the San Francisco Bay Area, one in Los Angeles, and one in the Central Valley area—that were observed during a two-year period between 1985 and 1986 constitute the study sample. All of the psychiatric emergency services in the study were licensed, authorized centers for psychiatric evaluations.
The patients were chosen consecutively on entry to the psychiatric emergency service. Observers were available around the clock, seven days a week. An observer did not skip observing an evaluation for any reason other than the patient's or the clinician's refusal to participate. The refusal rate—the proportion of evaluations that were not included in the study because of the patient's or clinician's preference—was 3.9 percent.
Patient evaluations were performed by psychiatric emergency service clinicians and observed by mental health professionals who were trained clinical research observers and experienced in assessing severely disturbed behavior. The observer accompanied the patient and the clinician throughout the course of the assessment until a disposition decision was reached by the clinician, witnessed all interactions, including telephone contacts, and was privy to all information available to the clinician. In addition to information about the patient that had been gathered by the clinician, the observer's impressions about the patient and several aspects of the clinician's treatment of the patient were recorded on structured scales in the form of process notes.
Interrater reliability in the range of .8 to .9 on key study instruments was established before the independent observations were initiated. Human subjects procedures were reviewed and approved by 11 committees affiliated with the psychiatric emergency services and researchers' institutions.
The psychiatric emergency service clinicians were at no time aware of the contents of the instruments coded by the observers. The dangerousness assessments in the psychiatric emergency service were based on specific units of information that are constructed into validated patterns of dangerousness and disability through the use of computer programs. The observers were not privy to the coding schemes and were effectively blinded to the scoring of the assessments, giving the study a double-blind effect.
After the initial reliability checks, the observers were accepted by the psychiatric emergency service clinicians as part of the routine staff. Clinicians made no effort to impress the observers or attend to liability concerns and freely shared their opinions about patients during the evaluations. The researchers' experience mirrored that of the makers of Frederick Wiseman's documentaries: once they were accepted, it was business as usual.
Measures
Coercive disposition.Patients who clearly expressed the wish to avoid hospitalization and who were detained were considered to have a coerced involuntary retention.
Admission criteria and severity of the patient's condition.Four admission criteria that are consistent with current and proposed legal requirements were analyzed as indicators of the severity of the patient's condition: the clinician's assignment of a DSM-III diagnosis of a psychotic disorder; the likelihood of the patient's causing harm to self, causing harm to others, or being gravely disabled at the time of the evaluation, as indicated by the score on TRIAD Dangerousness Scale (completed by the observer and ranging from 1 to 11, with higher scores indicating increased dangerousness) (20). The Treatability Scale, which was completed by the observer, indicates that the patient is judged to be treatable (20). Any of the scale's nine items that apply to the patient are scored either 0 or 1, and the sum of the scores is divided by the number of items scored. The result is a score varying between 0 and 1, with higher scores indicating greater treatability. The Benefit From Hospitalization Scale, which was completed by the observer, is a four-item measure of the patient's capacity to benefit from hospitalization. The scoring procedure is similar to that for the Treatability Scale. The summary score varies between 0 and 1, with higher scores indicating a greater likelihood of the patient's benefiting from hospitalization.
Mental disorder and dangerousness are the prevailing admission criteria in California and should be the sole subject of the assessment. Treatability and ability to benefit from hospitalization represent measurable aspects of a "need for treatment criteria" approach, proposed by advocates of the American Psychiatric Association's Model Law (10,21,22). Use of these variables in civil commitment evaluations would be considered by some an expansion of clinical discretion and by others a violation of due process.
Procedural justice indicators. Procedural justice indicators measure whether the evaluation was carried out in a manner that would lead an impartial observer to conclude that a serious and unbiased effort was made to determine the patient's status on the legal admission criteria. We used three indicators of procedural justice—involuntary legal status at entry to the psychiatric emergency service, score on a scale assessing the degree to which physicians engaged patients in the evaluative process, and influence of advocates for hospitalization.
Deviance theorists argue that civil commitment proceedings lack procedural justice because persons arriving at the psychiatric emergency service are routinely processed and retained on the basis of their prior status or label (3). Under such circumstances, prediction of the patient's disposition would be highly associated with the patient's legal status at entry to the psychiatric emergency service. We tested this assumption by including this indicator as a predictor of coercive disposition in assessing psychiatric emergency service decisions.
Legal status at entry should not necessarily be a significant predictor of retention if psychiatric emergency service clinicians are properly evaluating patients' dangerousness and taking into account the fact that patients' status on the dangerousness standard may change significantly during a 24-hour evaluation period in the psychiatric emergency service. For example, suicidal patients may respond to crisis intervention and no longer be dangerous to themselves, and individuals on amphetamines whose condition mimics a psychotic state may improve as the drug effects subside.
The primary concern in assessing procedural justice is to determine whether the process is conducted fairly (24,25). Fairness can be achieved only when the patient has been given the chance to participate in the evaluation to the maximum extent possible (1,25,26,27). The Art of Care Scale, although designed to measure one aspect of quality of care (28), can be used to measure the extent and character of such participation. The scale score is the average of four items (scored 1 if present and 0 if absent) that address the clinician's attempt to engage in a collaborative interaction, elicit information from the patient, include the patient in planning at a level appropriate to his or her functioning, and attend to the patient's feelings with empathy. In this study, interrater agreement in coding these items from process notes in 20 randomly selected evaluations rated by four different rater pairs averaged 79 percent, and the internal consistency was good (alpha=.69).
An additional concern in civil commitment evaluations has been the inappropriate influence of advocates in the psychiatric emergency service evaluation process. A patient may fail to exercise a free choice in entering a psychiatric hospital; therefore, undue influence exerted by others whose preferences may dominate the evaluation may lead to coercive retention (24,25,29,30). Family members, friends, companions, foster home managers, and even legal guardians often take an affirmative stand supporting a decision to retain the patient. These people may be present in the psychiatric emergency service during the evaluation or may have been contacted by psychiatric emergency service staff about the retention or release decision. Their having expressed a definite opinion supporting hospitalization places them in an advocacy position.
Institutional constraints. Three institutional constraints that might contribute to a clinician's use of a coercive disposition were measured. They were the clinician's workload, measured by a four-item Bartlett-factor score (created with principal axis factoring and quartermax rotation with Kaiser normalization) (31) that included the patient-staff ratio in the psychiatric emergency service (factor weight=.257), the clinician's patient load (factor weight=.683), and the total number of inpatient beds (factor weight=-.132) and of out-of-hospital beds (factor weight= -.168) available at the time of the evaluation; the difficulty of the setting in which the evaluation was completed, scored 1 or 0 for the presence or absence of relentless noise, limited space, limited telephone access, visual distractions, or other negative conditions; and whether the patient had insurance coverage.
Social bias indicators. Social bias indicators that might prejudice a clinician's action toward adopting a coercive disposition include demographic characteristics that have a conventional association with discrimination, such as the patient's gender (coded 1 for female and 0 for male) and ethnic minority status (coded 1 for African American and 0 for other).
Data analysis
We report the demographic characteristics of the patients and clinicians and the results of the bivariate analyses of factors predicting whether coercive retention was the outcome of a psychiatric emergency service evaluation. Bivariate relationships were evaluated with t tests for differences in means and chi square analyses for differences in proportions.
A two-stage logistic regression model was used to examine the relative importance and significance of admission criteria, procedural justice indicators, institutional constraints, and social biases in clinicians' decisions on coercive dispositions. The first stage included the aforementioned factors. In the second stage, a set of control factors was entered. The model was run twice, once with a block of control factors involving quality-of-care issues measured by clinicians' experience and Gustofson's Technical Quality of Care Scale (20), and the second time with a block of control factors involving methods issues such as the time of entry into the psychiatric emergency service, the time the retention or release decision was made (both coded as 0 for 9 a.m. to 5 p.m. or 1 for all other times), and the hospital in which the decision was made (eight of nine possible dummy variables coded 0 or 1).
Results
Characteristics of patients and clinicians
The modal patient was white (N= 381, or 65.3 percent), male (N=332, or 56.9 percent), age 27 (mean±SD= 35.4±14.9), and a fluent English-speaker (N=552, or 94.7 percent). Ethnic minority groups were well represented in the sample, which included 98 African Americans (16.8 percent), 68 persons with a Spanish surname (11.7 percent), eight Asians (1.4 percent), and 28 members of other minority groups (4.8 percent), including Pacific Islanders, Native Americans, and those who identified themselves as multiethnic. Only 14 patients (2.4 percent) spoke no English.
Patients' functioning at entry to the psychiatric emergency service was rated by clinicians with the Global Assessment Scale (GAS). The patients' mean±SD score on the GAS was 35.4±13.4 (median=35), and 383 patients (65.7 percent) had a GAS score of 40 or below, indicating a condition severe enough to warrant acute treatment (30). These patients' functioning levels indicated that they had major impairment or needed constant supervision.
The evaluating clinicians were primarily psychiatrists or other physicians (N=254, or 43.6 percent) but also included registered nurses (N=65, or 11.3 percent), master's-level psychologists (N=65, or 11.3 percent) and social workers (N=45, or 7.7 percent), licensed psychiatric technicians (N=56, or 9.6 percent), trainees (N=14, or 2.4 percent), doctoral-level psychologists (N=8, 3.1 percent), and persons with other credentials (N=65, or 11.2 percent), such as marriage and family counselors. Most nonpsychiatrists had access to a psychiatrist for consultation. Of the evaluators, 488 (84 percent) were white, 46 had a Spanish surname (7.9 percent), 32 were African American (5.5 percent), 11 were Asian (2.1 percent), and four were members of other ethnic groups (.7 percent). The evaluators had a mean±SD of 5.8±4.9 years of experience working in the psychiatric emergency service.
Admission criteria. The mean± SD TRIAD dangerousness score was 3.1±2.2, indicating that the average patient was ill enough to meet any one of the three dangerousness criteria for civil commitment—danger to self, danger to others, or grave disability. Although 546 of the patients (93.8 percent) were considered to have some mental disorder, only 364 (62.5 percent) were found by clinicians to have a psychotic disorder. Almost half of the patients (N=216, 44.8 percent) had scores above the mean on the Treatability Scale, and 117 (24.3 percent) were viewed as most able to benefit from hospitalization.
Procedural justice indicators. A majority of the patients entered the psychiatric emergency service with an involuntary legal status (N=347, or 55.9 percent). Advocates offered advice to hospitalize a patient in 168 of the 583 evaluations (28.8 percent). Of the advocates who supported hospitalization, 37.3 percent (N= 68) were relatives or friends, 33.7 percent (N=61) were professionals, and 14.5 percent (N=26) were interested community members, such as landlords. On the Art of Care Scale, 231 patients (39.6 percent) received the highest score, indicating that, within their capabilities, they had been fully engaged in the evaluation process.
Institutional constraints. More than a fourth of the patients (N=159, or 27.3 percent) had no medical insurance, and 11 percent (N=64) were evaluated under conditions that were considered difficult. The workload factor score was a function of four conditions at the time of the evaluation: evaluator caseload (mean±SD=1.78±1.52 patients, range=one to eight patients), patient-staff ratio in the psychiatric emergency service (mean±SD=.84± .62, range=.14 to 4.00), available beds in the hospital (mean±SD= 3.8±4.8, range=0 to 20), and available beds outside the hospital (mean±SD=3.8±4.8, range=0 to 24). Although the factor score was primarily defined by the weight given to caseload and secondarily to patient-staff ratio, bed availability influences clinicians' experience of workload.
Coercive retention
Bivariate analyses. Of the 583 evaluations we investigated, 18.7 percent (N=109) involved patients who were retained against their wishes. Bivariate differences favoring coercive retention were noted for two admission criteria: the TRIAD dangerousness score (mean± SD=4.01±2.21 versus mean±SD= 2.77±2.27 for coercively retained patients and other patients, respectively; t=5.37, df=192.9, p<.001) and a psychotic diagnosis (80.6 percent for coercively retained patients versus 58.8 percent for other patients; χ2= 17.44, df=1, p<.001). The only other bivariate difference favoring coercive retention was the more frequent presence of advocacy for hospitalization in the evaluations of patients who were coercively retained (38.3 percent versus 20.6 percent for other patients; χ2=14.27, df=1, p<.001).
Multivariate analysis. Because neither the quality of care nor the controls related to site and time of assessment significantly contributed to the multivariate model for predicting coercive retention, findings are presented for a single-stage logistic regression analysis that included only those factors in our theoretical construction. Five factors significantly predicted coercive retention (see Table 1). The most important factor in predicting a coercive detention was a diagnosis of a psychotic disorder. For patients with such a diagnosis, the likelihood of being coercively detained was 370 percent higher than for patients without such a diagnosis, all other factors taken into account. Patients with other psychiatric admission criteria also were more likely to receive coercive retention.
A 3-point increase in the dangerousness score, which is a clinically significant increase, was associated with a 54 percent increase in the probability of retention, and a 1-point increase in the treatability score (that is, from 0 to 1) was associated with a 72 percent reduction in the probability of coercive retention. The presence of at least one advocate for hospitalization was associated with a 204 percent increase in the probability of coercive retention, and an increase of 1 unit on the workload scale was associated with a 13 percent increase in the probability of retention. The availability of a less restrictive alternative to hospitalization was associated with a 54 percent reduction in the probability of a coercive retention.
Role of the advocate
Given the distinct and apparently influential role of the advocate in coercive retention, we conducted a separate analysis using logistic regression to predict advocacy for hospitalization from all other factors in the analysis, excluding disposition. We found only one significant predictor in this model—psychosis. This finding suggested that the advocates were acting on the basis of their belief that the patient was severely mentally ill and in need of protective custody rather than on the basis of any biases against the patient. This conclusion was buttressed by additional information from the research observer's process notes supporting the truthfulness of the advocates and their contribution to certainty in the assessment of the patient's dangerousness or grave disability.
Unfortunately, data gathering was well under way before these questions were asked, and therefore data on these issues were available for only 119 evaluations. In 19 of the 20 evaluations in which an advocate for hospitalization was present (95 percent), the observer was inclined to support the truthfulness of the advocate and indicated that the information provided by the advocate made the assessment of the patient's level of dangerousness more certain (χ2= 4.00, df=1, p<.05). Thus it appears that advocates for hospitalization facilitate procedural due process rather than bias the process.
Discussion
In civil commitment the state allows a special abridgment of individual rights. Therefore, only strict conformity to narrowly defined commitment criteria can ensure procedural justice, prevent unnecessary coercion, and be fully consistent with the guarantees of the Fourteenth Amendment. In California the criteria for civil commitment are dangerousness to self or others or grave disability due to a mental disorder, in the absence of a less restrictive alternative for care of the patient. To ensure procedural justice, no indicators other than those criteria should enter into the decision to coercively retain a patient.
The decisions for coercive retention in the evaluations we studied were, appropriately, primarily a function of the patient's psychosis and degree of dangerousness. These retentions were further constrained by the availability of a less restrictive alternative to commitment and facilitated by information from advocates. We were gratified to find that the old issues of institutional processing—as measured by clinicians' response to patients with involuntary legal status at entry to the psychiatric emergency service—which were of concern to adherents of the social deviance perspective, and the continuing issues of social bias were not significant predictors of coercive retention in this study.
Our finding that the institutional constraint of clinicians' workload was a factor in coercive retention is of particular concern in a managed care environment that deemphasizes the use of inpatient care and emphasizes time management and efficiency. This finding raises the possibility that clinicians are not being given enough staff support and other resources to make a decision solely on the basis of the specified criteria. The psychiatric emergency service can be a dangerous place, especially when a large number of patients are present. Without enough support, clinicians may choose to coercively retain a person who otherwise might have been given a more appropriate disposition.
Patients whose evaluation suggested a higher level of treatability were less likely to be retained. Thus we can conclude that this variable does not introduce a bias for coercive retention into the evaluation process. Assessment of treatability includes a judgment of the patient's willingness to accept and participate in treatment, and this relationship may help to explain why higher levels of treatability are associated with a lower likelihood of retention. Clinicians are probably more likely to believe that a patient with a higher level of treatability will comply with an alternative disposition. Treatability seems to function as an alternative clinical indicator that allows the clinician to weigh the adequacy of the less restrictive alternative option.
Although the findings of this study may not be replicable in other jurisdictions, they do represent the practice in nine different counties in California. Further, because no significant effects of study site were observed beyond those contributed by the study variables, we believe the findings may be generalized to other jurisdictions in California and, to a lesser extent, to other states that use the dangerousness criterion as part of a crisis evaluation in the first phase of the civil commitment process.
Conclusions
Decision making leading to coercive dispositions in the civil commitment evaluations we studied generally afforded patients due process. The evaluations satisfied the aspiration of the legal process in commitment proceedings "to minimize the risk of erroneous decisions" (6). In these evaluations, this risk was minimized by strict adherence to a process of reaching civil commitment disposition solely on the basis of the prevailing admission criteria. The presence of an advocate for hospitalization seemed to facilitate, rather than bias, due process.
Nevertheless, when inappropriate influences such as workload pressures result in an individual's detention, that person's Fourteenth Amendment liberties may have been infringed. The person may not have been afforded the proper procedural safeguards or may not have met the constitutional standard for involuntary commitment. The problems related to workload that we identified appear to be the result of an underfunded psychiatric emergency service system. The solution is not to abandon what appears to be an excellent effort to ensure patients' rights to due process under adverse conditions but to improve those conditions so that violations of due process do not arise.
Acknowledgments
This study was supported by grant MH-37310 and training grant MH-18828 from the National Institute of Mental Health.
Dr. Segal is professor and director and Dr. Laurie is research associate in the mental health and social welfare research group of the School of Social Welfare of the University of California, 120 Haviland Hall, Berkeley, California 94720 (e-mail, [email protected]). Mr. Segal is an attorney with Preston, Gates, and Ellis, LLP, in Seattle.
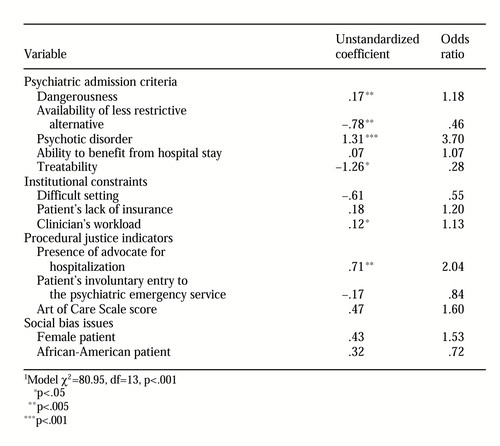 |
Table 1. Logistic regression analysis of factors predicting coercive retention of patients in civil commitment evaluations (N=445) in nine general hospital psychiatric emergency services in 1
1. Hoge SK, Lidz CW, Eisenberg M, et al: Family, clinician, and patient perceptions of coercion in mental hospital admissions: a comparative study. International Journal of Law and Psychiatry 21:131-146, 1998Crossref, Medline, Google Scholar
2. Segal SP, Watson M, Goldfinger S, et al: Civil commitment in the psychiatric emergency room: I. the assessment of dangerousness by emergency room clinicians. Archives of General Psychiatry 45:748- 752, 1988Crossref, Medline, Google Scholar
3. Segal SP, Watson M, Goldfinger S, et al: Civil commitment in the psychiatric emergency room: II. mental disorder indicators and three dangerousness criteria. Archives of General Psychiatry 45:753-758, 1988Crossref, Medline, Google Scholar
4. Segal SP, Watson M, Goldfinger S, et al: Civil commitment in the psychiatric emergency room: III. disposition as a function of mental disorder and dangerousness indicators. Archives of General Psychiatry 45:759-763, 1988Crossref, Medline, Google Scholar
5. Vitek v Jones, 445 US 480, 491-492 (1980)Google Scholar
6. Addington v Texas, 441 US 418, 425-427 (1979)Google Scholar
7. O'Connor v Donaldson, 422 US 563, 575-576 (1975)Google Scholar
8. Zinermon v Birch, 494 US 113, 138-139 (1990)Google Scholar
9. Lanterman-Petris-Short Act (Cal Welf & Inst Code, div 5 pt 1)Google Scholar
10. Assembly Interim Committee on Ways and Means, Subcommittee on Mental Health: The Dilemma of Mental Commitments in California: A Background Document. Sacramento, California State Legislature, 1966Google Scholar
11. Brakel SJ, Parry J, Weiner BA: The Mentally Disabled and the Law, 3rd ed. Chicago, American Bar Foundation, 1985Google Scholar
12. Applebaum PS: Almost a Revolution: Mental Health Law and the Limits of Change. New York, Oxford University Press, 1994Google Scholar
13. Kanapaux W: Outpatient commitment builds momentum: did NY debate incite public fear or solve a neglected problem? Behavioral Healthcare Tomorrow 8:12- 18, 1999Google Scholar
14. Cal Welf & Inst Code, Sec 5150Google Scholar
15. Cal Welf & Inst Code, Sec 5151Google Scholar
16. Scheff T: Being Mentally Ill. Chicago, Aldine, 1966Google Scholar
17. Whaley AL: Ethnicity/race, paranoia, and psychiatric dangerousness: clinician bias vs sociocultural differences. Journal of Psychotherapy and Behavioral Assessment 19:1-20, 1997Crossref, Google Scholar
18. Wanck B: Two decades of involuntary hospitalization legislation. American Journal of Psychiatry 141:33-38, 1984Link, Google Scholar
19. Appelbaum PS: Civil commitment: is the pendulum changing direction? Hospital and Community Psychiatry 33:703-704, 1982Google Scholar
20. Segal SP, Egley L, Watson MA, et al: The quality of psychiatric emergency evaluations and patient outcomes in county hospitals. American Journal of Public Health 85:1429-1431, 1995Crossref, Medline, Google Scholar
21. Stromberg CD, Stone AA: Statute: a model state law on civil commitment of the mentally ill. Harvard Journal on Legislation 20:275-396, 1983Medline, Google Scholar
22. Rubenstein LS: APA's model law: hurting the people it seeks to help. Hospital and Community Psychiatry 36:968-972, 1985Abstract, Google Scholar
23. Tyler T: The psychological consequences of judicial procedures: implications for civil commitment hearings. Southern Methodist University Law Review 46:433- 445, 992Google Scholar
24. Tyler TR, Lind EA: A relational model of authority in groups, in Advances in Experimental Social Psychology, vol 25. Edited by Zanna M. New York, Academic Press, 1992, pp 115-192Google Scholar
25. Monahan J, Hoge SK, Lidz C, et al: Coercion and commitment: understanding involuntary mental hospital admission. International Journal of Law and Psychiatry 18:246-263, 1997Google Scholar
26. Hoge SK, Lidz CW, Eisenberg M, et al: Perceptions of coercion in the admission of voluntary and involuntary psychiatric patients. International Journal of Law and Psychiatry 20:167-181, 1997Crossref, Medline, Google Scholar
27. Lidz CW, Hoge SK, Gardner W, et al: Perceived coercion in mental hospital admission: pressures and process. Archives of General Psychiatry 52:1034-1039, 1995Crossref, Medline, Google Scholar
28. Segal SP, Egley L, Watson MA, et al: Factors in the quality of patient evaluations in general hospital psychiatric emergency services. Psychiatric Services 46:1144- 1148, 1995Link, Google Scholar
29. Bloom BL, Asher SJ (eds): Psychiatric Patient Rights and Patient Advocacy: Issues and Evidence. New York, Human Sciences Press, 1982Google Scholar
30. Endicott J, Spitzer RL, Fleiss JL, et al: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry 33:771-776, 1976Crossref, Google Scholar
31. SPSS for Windows, Version 9.0. Chicago, SPSS Inc, 1999Google Scholar



