The Cost of Access to Mental Health Services in Managed Care
Abstract
Managed care has controlled the cost of specialty mental health services, but its impact on access to care is not well described. In a retrospective design, the study used empirical data to demonstrate a direct relationship between managed care plans' claims costs per member per month and the proportion of plan members who use specialty mental health services annually. Each increment of $1 per member per month in spending on claims was associated with a .9 percent increase in the proportion of enrollees receiving specialty mental health treatment. These data raise concerns that plans with low per-member per-month costs may unduly restrict access to specialty treatment.
As managed care has effectively controlled the cost of behavioral health services, access to mental health services has become of increasing concern to patients, providers, payers, and advocates for the mentally ill. The proportion of total health benefit costs attributed to behavioral health in private, employment-based health insurance decreased from 6.1 percent of the total health benefit in 1988 to only 3.1 percent in 1997, according to a recent study (1). However, the impact of cost containment on the delivery of mental health services, including access to care, warrants investigation.
In the era before managed behavioral health care, between 5.8 percent and 5.9 percent of all adults in the United States used specialty mental health services each year in either public or private treatment settings. These findings on access from the Epidemiologic Catchment Area survey in the early 1980s (2) and the National Comorbidity Survey in the early 1990s (3) have not been replicated on a national level since the onset of the managed care era in the middle to late 1990s. However, data reflecting cost and access in a managed care environment were collected by researchers at the National Institute of Mental Health (NIMH) for a report requested by the Senate Appropriations Committee on the impact of parity and managed care on the cost, access, and quality of mental health services (4).
The study reported here tested the hypothesis that a direct relationship exists between insurance companies' expenditures on behavioral health care, measured as the per-member per-month treatment cost (independent variable), and access to care, measured as the proportion of plan members who use services annually (dependent variable). This retrospective study used data from previously published reports and data collected for the NIMH report.
It may seem tautological that plans with lower per-member per-month costs treat fewer patients. However, differences in treatment intensity or quality rather than differences in the number of patients treated may account for variability in per-member per-month costs. To our knowledge, this study is the first examination of empirical data to address this question.
Methods
Published data from managed care programs reporting data on cost and access were obtained from a literature review (5,6,7,8). The data covered the years 1992 to 1997. The authors also collected 1993 to 1997 data from proprietary managed care sources and the North Carolina state employee benefit program after the state carved out its mental health benefits in 1992. Analyses are based on a total of 1.25 million persons and 2.75 million person-years.
Claims costs are reported in per-member per-month dollar expenditures by the behavioral health plan. Costs were adjusted for inflation to reflect 1997 dollars, using the medical care consumer price index (9). Neither administrative costs nor patient deductibles and copayments are included.
Access to care was measured using outpatient treated prevalence rates, that is, the proportion of members using outpatient services annually. This measure slightly understates the proportion of individuals receiving any services because a few users may use only inpatient or intermediate-level services. However, most data sources are unable to provide unduplicated counts across treatment settings. Outpatient treated prevalence was chosen as the best estimate of the overall proportion of service users.
The unit of analysis was the managed care plan. To test the hypothesis that claims costs and treated prevalence are directly related, linear regression was used to analyze the data using STATISTIX for Windows (10). The R2 represents the proportion of variability in the per-member per-month cost that is explained by the linear relationship between that cost and treated prevalence rates.
Results
A wide range of claims costs and treated prevalence rates was found across plans. Claims costs for mental health services varied sixfold, from $1.97 to $12.04 per member per month (1997 dollars), and treated prevalence varied more than tenfold, from 1.03 to 9.97 percent.
Cost and access data are plotted in Figure 1. A straight line describes the relationship between cost and access well. The regression equation is as follows: treated prevalence (percent) =.9 × per-member per-month cost (dollars) + .25
The slope of the line is .90, and the R2 value is .65. Thus each increment of $1 per member per month in spending on claims was associated with a .9 percent increase in the proportion of enrollees receiving specialty mental health treatment. Conversely, each decrement of $1 in spending was associated with a .9 percent decrease in the treated prevalence rate.
Discussion
These data raise concerns that plans paying lower per-member per-month costs actively contain costs by restricting access to specialty treatment. Before widespread managed care, the Epidemiologic Catchment Area study and the National Comorbidity Survey reported treated prevalence rates of 5.8 to 5.9 percent, with an average of 14 visits per patient per year. Our study shows that it costs about $6 per member per month to reach this level of access. If this is the "appropriate" treated prevalence rate, then claims costs below $6 per member per month should raise concerns about the decline in access, quantity, and quality as a consequence of cost containment. Cost containment strategies that may effectively limit access include benefit design features, such as high copayments and deductibles, stringent authorization-of-care practices, and incentives to reduce referrals to specialty treatment.
Several limitations of the study should be noted. First, we used a convenience sample of managed care plans: those that had published data on cost and access and those that agreed to provide data to NIMH. These plans reflect a wide range of costs but may not be representative of managed care plans overall. However, one might expect that plans voluntarily reporting these data are among the better plans. Second, these plans encompass a range of managed care practices, from loosely managed nonrisk contracts to more tightly managed at-risk arrangements. Third, in some plans, selection factors or different cultural attitudes toward seeking treatment may contribute to variation in demand for services.
A fourth limitation is that our analysis does not account for the lack of independence of multiple observations of the same plan in different years. Finally, mental health treatment in primary care settings was not measured. However, because we studied only plans with behavioral health carve-outs, this limitation is unlikely to be a major source of variability between plans.
It is also important to note that although the proportion of enrollees receiving treatment is a useful indicator of access to care, it does not reflect other aspects of access such as treatment intensity, waiting times for appointments and telephone responses, access to a continuum of services, geographic access, and culturally competent treatment. Nor do populationwide treatment rates reflect differences in access for vulnerable populations, including poor people, members of racial minority groups, those with physical disabilities, and those with severe mental illness.
Conclusions
The direct relationship between claims costs and treated prevalence rates suggests that at low levels of spending, access to care may be compromised. Our results also show that the relationship between cost and access holds throughout a wide range of costs; no upper limit for access was found even at high spending levels, nor was there a spending level below which access leveled off and nonaccess strategies for cost control were the only ones used.
Further studies are needed to examine how barriers to access are enacted and whether they preferentially affect certain patient groups, such as those with severe mental illness. Studies examining treatment intensity and quality in high- and low-cost plans are also needed.
Acknowledgments
The authors thank Agnes Rupp, Ph.D., and Sam Zuvekas, Ph.D., for helpful discussion and comments.
When this study was conducted, Dr. Weissman was a special expert at the National Institute of Mental Health (NIMH). She is now a psychiatrist at the Mental Illness Research, Education, and Clinical Center at the Bronx Veterans Affairs Medical Center. Dr. Pettigrew is a statistical consultant in the division of services and intervention research at NIMH. Dr. Sotsky formerly was senior science adviser in the office of the associate director for epidemiology and health policy research at NIMH. He is now research professor for psychiatry and public health at the Center for Health Services Research and Policy at George Washington University in Washington, D.C. Dr. Regier formerly was associate director for epidemiology and health policy research at NIMH. He is now executive director of the American Psychiatric Institute for Research and Education. Send correspondence to Dr. Regier at the American Psychiatric Association, 1400 K Street, N.W., Washington, D.C. 20005 (e-mail, [email protected]). This paper was presented at the annual meeting of the American Psychiatric Association held May 15–20, 1999, in Washington, D.C.
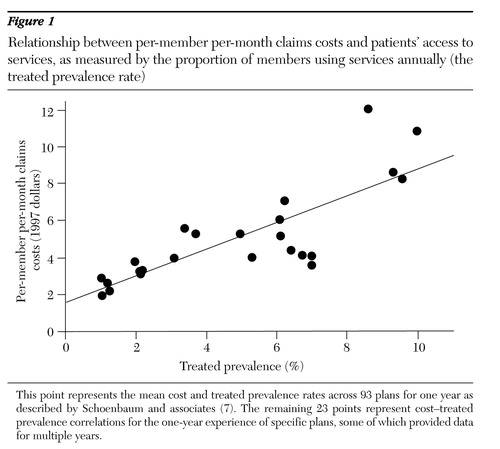
Figure 1. Relationship between per-member per-month claims costs and patients' access to services, as measured by the proportion of members using services annually (the treated prevalance rate)
1. Health Care Plan Design and Cost Trends:1988 Through 1997. Washington, DC, Hay Group, 1998Google Scholar
2. Regier DA, Narrow WE, Rae DS, et al: The de facto US mental and addictive disorders service system: Epidemiologic Catchment Area prospective 1-year rates of disorders and services. Archives of General Psychiatry 50:85-94, 1993Crossref, Medline, Google Scholar
3. Kessler RC, Frank RG, Edlund M, et al: Differences in the use of psychiatric outpatient services between the United States and Ontario. New England Journal of Medicine 336:551-557, 1997Crossref, Medline, Google Scholar
4. Parity in Financing Mental Health Services: Managed Care Effects on Cost, Access, and Quality. Washington, DC, National Advisory Mental Health Council, 1998Google Scholar
5. Goldman W, McCulloch J, Sturm R: Costs and use of mental health services before and after managed care. Health Affairs 17(2):40-52, 1998Google Scholar
6. Ma CA, McGuire TG: Costs and incentives in a behavioral health carve-out. Health Affairs 17(2):53-69, 1998Google Scholar
7. Schoenbaum M, Zhang W, Sturm R: Costs and utilization of substance abuse care in a privately insured population under managed care. Psychiatric Services 49:1573-1578, 1998Link, Google Scholar
8. Sturm R, Goldman W, McCulloch J: Mental health and substance abuse parity: a case study of Ohio's state employee program. Working paper 128. Los Angeles, University of California, Los Angeles, Research Center on Managed Care for Psychiatric Disorders, 1998Google Scholar
9. Consumer Price Index for Medical Care. Washington, DC, Department of Labor, Bureau of Labor Statistics, 1998Google Scholar
10. STATISTIX for Windows, Version 2.0. Tallahassee, Fla, Analytical Software, 1996Google Scholar