Shorter Hospital Stays and More Rapid Improvement Among Patients With Schizophrenia and Substance Disorders
Abstract
OBJECTIVE: Length of stay and treatment response of inpatients with acute schizophrenia were examined to determine whether differences existed between those with and without comorbid substance-related problems. METHODS: The sample comprised 608 patients with a diagnosis of schizophrenia or schizoaffective disorder treated on hospital units with integrated dual diagnosis treatment. They were rated on admission and discharge by a psychiatrist using a structured clinical instrument. Patients with no substance-related problems were compared with those with moderate to severe problems using t tests, chi square tests, and analysis of variance. RESULTS: When analyses controlled for age, gender, and other clinical variables, dually diagnosed patients were found to have improved markedly faster compared with patients without a dual diagnosis. Their hospital stays were 30 percent shorter on both voluntary and involuntary units. They also showed somewhat greater symptomatic improvement and no increase in 18-month readmission rates. On admission the dual diagnosis group was more likely to be younger, male, and homeless and more likely to be a danger to self and others. Severity of psychosis was the same at admission for the two groups, but the dually diagnosed patients were rated as less psychotic at discharge. CONCLUSIONS: Dually diagnosed patients with schizophrenia appear to stabilize faster during acute hospitalization than those without a dual diagnosis. The authors hypothesize that substance abuse may temporarily amplify symptoms or that these patients may have a higher prevalence of better-prognosis schizophrenia. The availability of integrated dual-focus inpatient treatment and a well-developed outpatient system may also have helped these patients recover more rapidly.
Comorbidity of schizophrenia and an addiction disorder, such as alcohol dependence, has been associated with increased psychotic symptoms and higher rates of emergency room and psychiatric admissions, incarcerations, and homelessness (1,2,3,4,5,6,7,8). This comorbidity is extremely common—persons with schizophrenia are three times more likely than persons without a psychiatric disorder to abuse alcohol and six times more likely to abuse drugs (9).
Roughly half of those diagnosed as having schizophrenia develop episodes of substance abuse or dependence during their lifetime. Dually diagnosed patients demonstrate increased rates of treatment dropout, more noncompliance with treatment, and increased rates of discharge against medical advice from psychiatric treatment as well as from addiction treatment (1,2,3,4,5,6,7,8). Analyzing these studies, two national task forces concluded that separate treatment of psychiatric and addiction disorders is characterized by poor outcome (10,11). They recommended integrated treatment, especially for patients with more severe mental illness.
Integrated outpatient treatment combines both psychiatric and addiction services and personnel in the same setting at the same time. Studies of integrated treatment have demonstrated decreased use of acute inpatient services, increased outpatient utilization, decreased substance use, and high rates of treatment satisfaction (6,12,13,14,15,16). Most outcome studies of dual diagnosis treatment have focused on outpatient treatment. Studies of treatment response to acute dual diagnosis inpatient treatment have been relatively lacking. Such studies would ask how patients with a severe mental illness, such as schizophrenia, and a comorbid addictive disorder respond when admitted on an emergency basis to an inpatient unit that has specific integrated dual diagnosis treatment tracks.
Although numerous studies on inpatient psychiatric units with nonintegrated acute care have demonstrated that dually diagnosed patients have increased symptoms and poor outcomes, how such patients might respond to integrated treatment is unknown. It could be hypothesized that such treatment would result in equivalent resolution of psychiatric symptoms for both dually diagnosed patients and those with no comorbid substance use disorders. However, it could also be hypothesized that such treatment would result in longer lengths of stay because two disorders are being treated.
Because these important questions have received little attention, we report here on a study of patients' responses to acute inpatient dual diagnosis treatment in a system in which integrated dual-focus treatment has been available for five years. Our goal was to compare illness severity at admission and discharge, change in symptom severity from admission to discharge, and lengths of stay in a large sample of patients with and without alcohol or other drug problems. We restricted our focus to the axis I diagnoses of schizophrenia and schizoaffective disorder, hereafter referred to as schizophrenia, because schizophrenia is one of the most severe psychiatric disorders and patients with this disorder have high rates both of hospitalization and of substance abuse (17).
Methods
Sample
The study sample consisted of all acute and emergency patients who were psychiatrically hospitalized during a three-year period (1993–1996) at Harborview Medical Center, a large, urban, university-run county hospital with three acute inpatient psychiatric units in Seattle. Patients in the sample had a definite primary diagnosis of schizophrenia or schizoaffective disorder (N=766). Virtually all patients were indigent, and their hospitalization was covered by Medicaid or Medicare. Patients with a questionable diagnosis of schizophrenia were omitted from the study (see the section on assessment). This diagnostic subsample accounted for 18 percent of the total inpatient psychiatric admissions. Because this study is based on routinely collected medical records data, no individual informed consent was obtained; however, the study's methodology was approved by our institutional review board.
As a standard part of the structured clinical evaluation, the patient's clinical psychiatrist uses all available data, including toxicology screens (18), to rate a patient's substance use on a continuum. A rating of 0 indicates no problems related to substance use; 1 or 2 indicates minor problems such as arguments and moodiness; 3 or 4 indicates major problems and is equivalent to a DSM-IV diagnosis of abuse; 5 or 6 indicates severe problems and is equivalent to a DSM-IV diagnosis of dependence. Ratings were missing for 64 of the 766 patients, and they were dropped from the analysis.
The 393 patients (56 percent) who had no substance-related symptoms were compared with the 275 patients (39 percent) who had moderate to severe substance-related problems, a rating of 3 to 6. The latter group are referred to as dually diagnosed patients. About 5 percent (N=32) of the patients had a rating of either 1 or 2, indicating mild problems. These patients did not fit into either group and were dropped from further analysis.
Ratings based on clinical information such as interviews, history, and toxicology screens have been found to be more accurate than discharge diagnoses for identifying substance use problems for both psychiatric inpatients (19) and outpatients (20) and have been advocated by an international consortium (21).
Fifty-four patients (8 percent) left the hospital against medical advice. Leaving against medical advice was significantly related to substance use; 5 percent of patients without a dual diagnosis left against medical advice, compared with 12 percent with a dual diagnosis (χ2=11.28, df=1, p<.001). Data for these patients were removed from further analyses, because the length of their hospital stays and any changes in severity scores did not reflect planned psychiatric treatment.
Six patients had hospital stays longer than two months and were defined as outliers; two patients had 64-day stays, and the other four had stays of 68, 69, 88, and 96 days. These patients were omitted from the study sample. Hence, the total study sample consisted of 608 patients, 368 with no substance use diagnosis (61 percent) and 240 with a dual diagnosis (40 percent).
Inpatient dual diagnosis treatment tracks
During the course of this study and for five years previously, all three acute psychiatric units at Harborview Medical Center had well-established dual diagnosis treatment tracks. In addition to standard psychiatric assessment and interventions, these tracks include key elements in the three areas of assessment, treatment, and discharge planning.
Drug and alcohol issues are independently and repeatedly assessed by all unit personnel, including physicians and nursing, social work, and chemical dependency staff. As a regular part of the unit structure, drug and alcohol issues are treated through the use of several therapies, including individual, group, and family therapy and medication. Drug and alcohol issues are also a key element in discharge planning related to housing, follow-up treatment, medication, and so forth. Patients without a dual diagnosis receive similar services, but without the drug and alcohol focus.
Assessments
All patients in the sample received standardized, psychiatrist-administered assessment batteries within 48 hours of admission and at discharge. Information was obtained on demographic characteristics and psychiatric history. DSM-IV diagnoses were documented by a checklist of criteria. Patients completed the Psychiatric Assessment Form (PAF), an expanded 23-item version of the Psychiatric Symptom Assessment Scale (PSAS) that has been shown to be reliable and valid for use with inpatients (22,23). The internal consistency reliability was .76 for both admission and discharge ratings. All PAF items are rated with descriptive behavioral benchmarks, with 0 indicating no problem; 1 and 2, a mild problem; 3 and 4, a moderate problem; and 5 and 6, severe pathology. We created a hallucinations-delusions item subscale by summing key items. We also report data on suicidality, depression, elevated mood, and hostility items.
The severity of the schizophrenia or schizoaffective disorder was rated by a psychiatrist on a standardized DSM-IV checklist that produced a severity-of-illness scale ranging from 0, no symptoms, to 100, all symptoms. Studies have demonstrated that accurate diagnoses of schizophrenia can be made even in the context of substance abuse (24), especially by university-based physicians using structured methods (25), as we did here. Patients who had psychotic features similar to schizophrenia but whose symptoms or course were unclear, or who experienced such symptoms only in the context of substance use, were given a diagnosis of psychosis not otherwise specified. A total of 371 patients had this diagnosis (12 percent of all patients admitted during the three-year period), and they were not included in the study.
The Mini Mental State Examination (MMSE) was administered at admission to assess cognitive functioning. The MMSE has scores ranging from 0 to 30, with high scores indicating better cognitive functioning. Length of stay and rehospitalization at the same facility within 18 months of the index visit were obtained from computerized medical records. Although this facility is the major public psychiatric hospital in the county, it is possible that the patients were rehospitalized in another facility. However, rehospitalization elsewhere should have either affected both groups equivalently or resulted in the dually diagnosed group being more likely to have been rehospitalized at Harborview because of its dual tracks.
Statistical analyses
Descriptive data were generated for the entire sample. Chi square tests with continuity corrections were performed for differences on categorical variables between patients with and without a dual diagnosis. T tests were used to examine group differences in age and MMSE scores. Two group analyses of covariance (ANCOVAs) were performed to examine group differences on the continuous variables. Demographic variables that were significantly different between patients with and without dual diagnoses were used as covariates. In analyses of variables measuring severity at discharge, the admission score for that variable was also included as a covariate. Medians and ranges for length of stay were examined, and median tests for independent groups were performed to ensure that the results were not due to the skewness of the data on length of stay. Analyses for length of stay were repeated for voluntary and involuntary patients.
Results
Sample
As Table 1 shows, of the 608 patients in the total sample, 65 percent were males and 68 percent were white. Twelve percent were employed, 28 percent were homeless on admission, and 17 percent had a moderate to severe comorbid medical illness. The mean±SD age was 38.4±11.9 years, with a range from 17 to 85 years. The mean±SD score on the MMSE at admission was 25.2±6, indicating mild cognitive impairment.
Seventy percent of the sample had two or more lifetime psychiatric inpatient hospitalizations. Forty percent were involuntarily committed to inpatient treatment. Forty-three percent had a history of assaultive behavior. Forty-two percent had a diagnosis of schizoaffective disorder, and 58 percent had a diagnosis of schizophrenia.
Demographic and clinical history
Table 1 also presents these data for patients with and without a dual diagnosis. Dually diagnosed patients were significantly more likely to be male, younger, and homeless and to have a history of assaultive behavior, although a significantly smaller proportion of patients were involuntary admissions. The two groups did not differ in ethnicity, employment, medical comorbidity, MMSE score, or history of psychiatric hospitalization. Fifty-three percent of the dual diagnosis group had a schizoaffective diagnosis, compared with 40 percent of patients without a dual diagnosis (χ2=9.98, df=1, p<.002).
Symptoms at admission and discharge
Table 2 presents data on measures of symptoms at admission and discharge for the total sample and the comparison groups. Significant differences were found between groups in age, gender, and the diagnosis of schizoaffective disorder, and these variables were used as covariates in the analyses examining group differences. Homelessness was not used as a covariate because it was viewed as a possible consequence of substance use. A dichotomously scored variable representing schizoaffective diagnosis was included as a covariate. The admission severity score was included as a covariate in analyses of discharge severity scores.
At admission, the comparison groups did not differ on any severity measures except for suicidality. The dual diagnosis group was significantly more suicidal on admission, although by discharge the mean scores for the two groups were identical on both items measuring suicidality. At discharge, after the analysis controlled for age, gender, schizoaffective disorder, and admission level of severity, the dual diagnosis group on average was rated as having less severe hallucinations and delusions. No other discharge differences were statistically significant.
Length of stay and recidivism
Table 3 presents data on length of stay and recidivism. Dually diagnosed patients had significantly shorter stays, averaging around five days or about 30 percent shorter than those of patients without a dual diagnosis. This finding was significant when age, gender, schizoaffective diagnosis, history of assault, and admission suicidality and depression were used as covariates. The results were also significant when nonparametric median tests were used. The stays of voluntary patients with a dual diagnosis were on average four days shorter than the stays of voluntary patients without substance abuse.
The same group differences were found for the involuntary patients using the ANCOVA and the nonparametric tests. The average stay for involuntary patients without a dual diagnosis was four days longer than for patients with dual diagnoses. No significant differences were found in the recidivism rates of the two groups over the 18-month follow-up period.
Discussion
Our findings indicate that among patients with schizophrenia, those with a dual diagnosis had significantly shorter hospital stays—about 30 percent shorter—than those without a comorbid substance use disorder, and the dual diagnosis group had a somewhat greater treatment response. This finding held for both voluntary and involuntary patients. The results could not be explained by demographic variables or by differences in clinical history. Indeed, the fact that the dual diagnosis group had more males should have increased the mean length of stay for the group and resulted in poorer outcome, because accumulating evidence shows that males with schizophrenia have a more severe form of the disorder than women (26).
The increased rate of discharges against medical advice in the dual diagnosis group, consistent with previous studies (23), also did not account for our findings. We further analyzed data to see if any cohort (by year) effect could be found on either the prevalence of comorbid substance problems or length of stay, and no significant effects were found.
One possible explanation is that the symptoms of patients with a dual diagnosis were induced or amplified by their substance use. Such symptoms might normalize fairly rapidly after the removal of abused substances, which would account for their shorter stays and improved outcomes. Unfortunately, it is not possible to differentiate acute substance-induced or -amplified psychotic symptoms from those of pure schizophrenia. Our ratings merely reflect a total summary of symptoms, substance-induced and otherwise. However, the higher level of suicidality and assaultive history in our dually diagnosed patients is consistent with findings that aggressiveness and suicidality are associated with substance-induced states (27).
These same findings could also be explained if dually diagnosed patients have a somewhat different form of schizophrenia, one with more inherent affect or impulsivity. This possibility is consistent with several findings for persons with schizophrenia—that those who abuse substances have better premorbid adjustment (28), that those with a deficit syndrome are less likely to abuse substances (29), and that dually diagnosed patients show a trend toward faster functional recovery when involuntarily hospitalized (30). However, other studies of dually diagnosed patients have found earlier age at first hospital admission and poorer treatment response (31).
A strength of this study is a methodology that includes diagnosis and illness ratings made as part of a standard procedure with known reliability and validity by academic attending psychiatrists who calibrated their ratings at monthly meetings and training sessions. The findings may be limited, however, by the context of treatment for severe mental illness provided in King County, which has limited hospitalization, first by countywide agreements, and, more recently, by a managed care system. This system maintains one of the lowest hospitalization rates in the U.S. (32) by diverting most subacute emergency cases to an outpatient assertive case management treatment system.
This system, by definition, tends to admit patients who are either of significant and immediate danger to themselves or others or who have failed to respond to outpatient treatment. The data suggest that our dually diagnosed patients are in the former group, with increased suicidality and assaultiveness, and that patients without dual diagnoses are in the latter group, with slower response to hospitalization as measured by ratings on symptoms of psychosis.
We might be criticized for including patients with schizoaffective disorder in our sample of patients with schizophrenia. We chose to include them because of concerns about the accuracy of differentiating distinct versus substance-induced affective syndromes among substance-using persons with schizophrenia. We therefore included both groups, but controlled for the schizoaffective diagnosis in our results. The findings from a separate analysis that combined both groups without such control were nearly identical to the data in our tables; however, these analyses, as expected, found even more profound differences between the groups in ratings of depression and suicidality.
Conclusions
In this study with a large sample, dually diagnosed patients with acute schizophrenia improved markedly faster than patients with schizophrenia who did not have a dual diagnosis. The dually diagnosed patients demonstrated 30 percent shorter lengths of stay, somewhat greater symptomatic improvement across measures, and no increase in 18-month readmission rates. We do not know whether our findings would be replicated if dual diagnosis treatment were not available. Other recent research on dually diagnosed patients has found either shorter lengths of stay (30) or stays of about the same length (33) as for patients without a dual diagnosis, and significantly greater overall treatment costs for dually diagnosed patients in typical psychiatric inpatient care (34,35). However, these studies did not control for demographic, diagnostic, or other clinical variables and did not use reliable admission and discharge ratings. The patients did not have access to a modern case management outpatient system or to dual diagnosis treatment.
It might be hypothesized that both acute inpatient dual diagnosis intervention and the outpatient programs that are more often described (10,11,12,13,14,15,16,17) and are aimed at the substance disorder might prevent or delay an immediate relapse to substance use and resulting revolving-door hospitalization. If this is the case, then the added expenses of integrating addiction staff, retraining psychiatric staff, and changing mental health care system practices might be offset by the relatively shorter inpatient stays in the dual diagnosis group, as was found within this system of care. We look forward to further clinical health services research in this area.
The authors are affiliated with the department of psychiatry and behavioral sciences of the University of Washington School of Medicine at Harborview Medical Center, Box 359911, 325 Ninth Avenue, Seattle, Washington 98104 (e-mail, [email protected]).
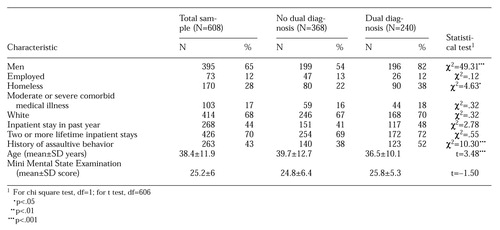 |
Table 1. Characteristics of 608 inpatients with schizophrenia or schizoaffective disorder, categorized by whether they had a dual diagnosis of a substance use disorder
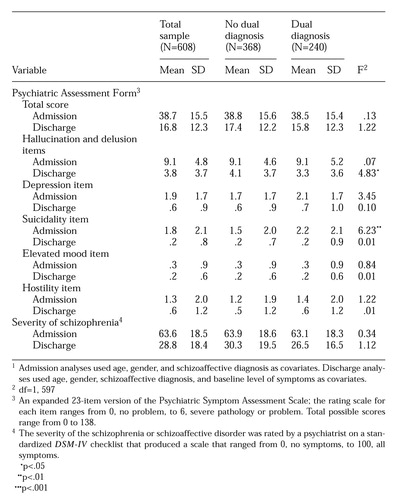 |
Table 2. Mean scores at discharge and admission of 608 inpatients with schizophrenia or schizoaffective disorder, categorized by whether they had a dual diagnosis of a substance use disorder1
1Admission analyses used age, gender, and schizoaffective diagnosis as covariatesDischarge analyses used age, gender, schizoaffective diagnosis, and baseline level of symptoms as covariates.
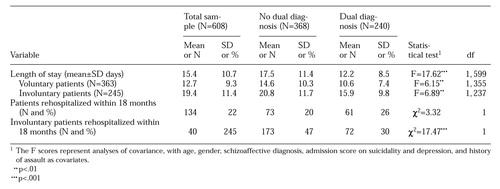 |
Table 3. Length of stay and recidivism among 608 inpatients with schizophrenia or schizoaffective disorder, categorized by whether they had a dual diagnosis of a substance use disorder1
1The F scores represent analyses of covariance, with age, gender, schizoaffective diagnosis, admission score on suicidality and depression, and history of assault as covariates
1. Cuffel BJ: Comorbid substance use disorder: prevalence, patterns of use, and course. New Directions for Mental Health Services, no 70:93-105, 1996Google Scholar
2. Pulver AE, Wolyniec PS, Wagner MG, et al: An epidemiologic investigation of alcohol-dependent schizophrenics. Acta Psychiatrica Scandinavica 79:603-612, 1989Crossref, Medline, Google Scholar
3. Mueser KT, Yarnold PR, Levinson DF, et al: Prevalence of substance abuse in schizophrenia: demographic and clinical correlates. Schizophrenia Bulletin 16:31-56, 1990Crossref, Medline, Google Scholar
4. Gupta S, Hendricks S, Kenkel AM, et al: Relapse in schizophrenia: is there a relationship to substance abuse? Schizophrenia Research 20:153-156, 1996Google Scholar
5. Swofford CD, Kasckow JW, Scheller-Gilkey G, et al: Substance use: a powerful predictor of relapse in schizophrenia. Schizophrenia Research 20:145-151, 1996Crossref, Medline, Google Scholar
6. Drake RE, Mueser KT, Clark RE, et al: The course, treatment, and outcome of substance disorder in persons with severe mental illness. American Journal of Orthopsychiatry 66:42-51, 1996Crossref, Medline, Google Scholar
7. Lehman AF, Myers CP, Corty E, et al: Prevalence and patterns of "dual diagnosis" among psychiatric inpatients. Comprehensive Psychiatry 35:1-5, 1994Crossref, Google Scholar
8. Bartels SJ, Teague GB, Drake RE, et al: Service utilization and costs associated with substance abuse among rural schizophrenic patients. Journal of Nervous and Mental Disease 181:227-232, 1993Crossref, Medline, Google Scholar
9. Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. JAMA 264:2511-2518, 1990Crossref, Medline, Google Scholar
10. Ries RK (ed): Assessment and Treatment of Patients With Coexisting Mental Illness and Alcohol and Other Drug Abuse. Rockville, Md, Center for Substance Abuse Treatment, 1994Google Scholar
11. Minkoff K (ed): Co-occurring Mental and Substance Disorders (Dual Diagnosis) Clinical Standards and Workforce Competencies Project: Annotated Bibliography. Rockville, Md, Center for Mental Health Services, 1997Google Scholar
12. Mueser KT, Bellak AS, Blanchard JJ: Co-morbidity of schizophrenia and substance abuse: implications for treatment. Journal of Consulting and Clinical Psychology 60:845-856, 1992Crossref, Medline, Google Scholar
13. Carey KB: Substance use reduction in the context of outpatient psychiatric treatment: a collaborative, motivational, harm reduction approach. Community Mental Health Journal 32:291-306, 1996Crossref, Medline, Google Scholar
14. Jerrell J, Ridgely MS: Comparative effectiveness of three approaches to serving people with severe mental illness and substance abuse disorders. Journal of Nervous and Mental Disease 183:566-576, 1995Crossref, Medline, Google Scholar
15. Rosenthal RN, Hellerstein DJ, Miner CR: A model of integrated services for outpatient treatment of patients with comorbid schizophrenia and addictive disorders. American Journal of Addictions 1:339-348, 1992Google Scholar
16. Ries RK, Comtois KA: Illness severity and treatment services for dually diagnosed severely mentally ill outpatients. Schizophrenia Bulletin 23:239-246, 1997Crossref, Medline, Google Scholar
17. Kessler RC, Nelson CB, McGonagle KA, et al: The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. American Journal of Orthopsychiatry 66:17-31, 1996Crossref, Medline, Google Scholar
18. Kranzler HR, Tennen H, Babor TF, et al: Validity of the longitudinal, expert, all data procedure for psychiatric diagnosis in patients with psychoactive substance use disorders. Drug and Alcohol Dependence 45:93-104, 1997Crossref, Medline, Google Scholar
19. Lehman AF, Myers CP, Dixon LB, et al: Detection of substance use disorders among psychiatric inpatients. Journal of Nervous and Mental Disease 184:228-233, 1996Crossref, Medline, Google Scholar
20. Drake RE, Alterman AI, Rosenberg SR: Detection of substance use disorders in severely mentally ill patients. Community Mental Health Journal 29:175-192, 1993Crossref, Medline, Google Scholar
21. Merikangas KR, Mehta RL, Molnar BE, et al: Comorbidity of substance use disorders with mood and anxiety disorders: results of the international consortium in psychiatric epidemiology. Addictive Behaviors 23:893-907, 1998Crossref, Medline, Google Scholar
22. Roy-Byrne PP, Dagadakis C, Ries R, et al: A psychiatrist-rated battery of measures for assessing the clinical status of psychiatric inpatients. Psychiatric Services 46:347-352, 1995Link, Google Scholar
23. Bigelow LB, Berthot BD: The Psychiatric Symptom Assessment Scale (PSAS). Psychopharmacology Bulletin 25:168-173, 1989Medline, Google Scholar
24. Strakowski SM, Tohen M, Flaum M, et al: Substance abuse in psychotic disorders: associations with affective syndromes: DSM-IV Field Trial Work Group. Schizophrenia Research 14:73-81, 1994Crossref, Medline, Google Scholar
25. Fennig S, Craig TJ, Tannenberg-Karant M, et al: Comparison of facility and research diagnoses in first-admission psychotic patients. American Journal of Psychiatry 151:1423-1429, 1994Link, Google Scholar
26. Andia AM, Zisook S, Heaton RK, et al: Gender differences in schizophrenia. Journal of Nervous and Mental Disease 183:522-528, 1995Crossref, Medline, Google Scholar
27. Steadman HJ, Mulvey EP, Monahan J, et al: Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Archives of General Psychiatry 55:393-401, 1998Crossref, Medline, Google Scholar
28. Arndt S, Tyrell G, Flaum M, et al: Comorbidity of substance abuse and schizophrenia: the role of pre-morbid adjustment. Psychological Medicine 22:379-388, 1992Crossref, Medline, Google Scholar
29. Kirkpatrick B, Amador XF, Flaum M, et al: The deficit syndrome in the DSM-IV Field Trial: I. alcohol and other drug abuse. Schizophrenia Research 20:69-77, 1996Crossref, Medline, Google Scholar
30. Sanguineti VR , Samuel SE: Comorbid substance abuse and recovery from acute psychiatric relapse. Hospital and Community Psychiatry 44:1073-1076, 1993Abstract, Google Scholar
31. Sokolski KN, Cummings JL, Abrams BI, et al: Effects of substance abuse on hallucination rates and treatment responses in chronic psychiatric patients. Journal of Clinical Psychiatry 55:380-387, 1994Medline, Google Scholar
32. Manderscheid RW, Sonnenschein MA (eds): Mental Health, United States, 1996. Rockville, Md, Center for Mental Health Services, 1996Google Scholar
33. Bradley CJ, Zarkin GA: Inpatient stays for patients diagnosed with severe psychiatric disorders and substance abuse. Health Services Research 31:387-408, 1996Medline, Google Scholar
34. Dickey B, Azeni H: Persons with dual diagnoses of substance abuse and major mental illness: their excessive costs of psychiatric care. American Journal of Public Health 86:973-977, 1996Crossref, Medline, Google Scholar
35. Hoff RA, Rosenheck RA: Long-term patterns of service use and cost among patients with both psychiatric and substance abuse disorders. Medical Care 36:835-843, 1998Crossref, Medline, Google Scholar