Alcohol & Drug Abuse: Improving Cost-Effectiveness in a Substance Abuse Treatment Program
In 1995 undersecretary for health Kenneth W. Kizer, M.D., M.P.H., announced his vision for change for the Department of Veterans Affairs (VA) health care system (1), followed in 1996 by his prescription for change (2). A main goal of this vision was expansion of the continuum of clinical service settings from inpatient to outpatient care to achieve excellence in health care in a more cost-efficient manner. During this same period, improving access to care for veterans (3) and increasing the number of veterans treated at each VA facility (4) became priorities.
This column reviews the response of one VA substance abuse program to these changes. In 1995 the James A. Haley VA Hospital had a 30-bed intensive 21-day inpatient program, a small eight- to 12-week outpatient program, and three aftercare groups. Our challenge was to transform this inpatient-focused program into a comprehensive ambulatory care service for patients who are largely homeless and unemployed and who have very limited family support or transportation capabilities. This challenge presented an opportunity to increase access to the program and to create a variety of new programs to better meet the diversified needs of our patients.
Program transformation
Background
Concerns about closure of the inpatient unit and quality of care were addressed in an earlier study by our team (5). That study compared the cost-effectiveness of a residential setting and an inpatient setting for patients in a three-week modified 12-step substance abuse treatment program. The two treatment groups did not differ significantly in abstinence rates after two months, but the residential program was much more cost-effective than the inpatient program—$4,346 versus $11,920 per patient. This proactive study helped position our team for the changes we were about to undergo.
The process
When the reorganization process began, no one on our team had a clear vision of the final product. However, we did have several principles to guide our efforts. First, the program had to become more accessible and more efficient, which meant that the expensive inpatient program had to close. Second, we would have to treat a larger number of individual patients in the coming years because VA reimbursement would no longer be based on hospital bed days of care. Instead, it would be based on the number of unique patients treated per fiscal year (4).
One of the major problems that we faced was staff anxiety and uncertainty about whether change would result in patients' receiving lower quality of care and in staff members' losing their jobs. These concerns were realistic. The reorganization described here did indeed result in many program changes, and we did lose staff, although they were absorbed by other hospital services. By involving staff members in a meaningful way in the reorganization, we were able to reduce anxiety and to reach consensus on major components of the new program. These goals were accomplished through a series of daily working lunch meetings with as many staff members who could attend over a period of two months.
Needs of patients and referring services
A key to any successful business is to know who your customers are. Only then can you meet your customers' needs. In our case, our customers consisted of patients and referring services. In past surveys, our patients told us that they wanted more individualized programs and more evening activities. The hospital staff who referred patients wanted faster responses to requests for consultation and shorter waiting times for patients to receive treatment. These requests became our goals.
Task forces that consisted of at least two staff members were assigned to unserved potential patient groups or services. Each task force was given about one week to investigate its subject area, collect data on the needs of patients and of staff members making referrals, and assess the feasibility of starting a new program to meet those needs. The task forces were then asked to present their findings and recommendations to our entire substance abuse team at daily lunch meetings.
After all the program possibilities were presented, staff had to reach agreement on which services would be most effective and would best meet the needs of our patients and referral sources. To make these decisions, we adopted three simple criteria: successful services are fast, good, and cheap. In our setting, these criteria translated into accessible, high-quality, and affordable patient care.
Program building blocks
Our first decision was to eliminate consultation waiting lists. We expanded our assessment team and made every effort to provide consultations on a same-day basis. This change increased access to all our programs and was appreciated by our patients and referring staff.
The first new component was a 16-bed residence, which was justified by our earlier study that found residential treatment more cost-effective than inpatient treatment (5). The residence was needed because closure of the inpatient unit left us no way to treat homeless patients, those with transportation problems, and those residing in high-drug-use and stressful environments. We were able to convince the hospital administration to let us use some of the funds saved from closing the inpatient unit to establish the residence. We then contracted with a nearby community facility—a five- to ten-minute walk from the hospital—for 16 supervised residential beds at a cost of $600 per bed per month. The supervision is provided by non-VA staff.
Our second new component was an intensive outpatient day program. The day program operates Monday through Friday and offers 18 hours a week of group treatment as well as individual counseling. Most patients stay three weeks. Patients in the residential program are offered an additional 12 treatment hours a week. The additional treatment consists of four hours of craft groups, four hours of life skills groups, and a four-hour weekly outing supervised by recreational therapy staff. The residential patients also participate in group meetings and Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) self-help groups at the residential facility in the evenings and on weekends.
After the intensive day program was set up, an intensive evening rehabilitation program was started for three nights a week from 5:30 to 7:30. The six- to eight-week program is designed for employed patients and those unable to attend the day program.
We developed a relapse prevention program, based on a cognitive-behavioral treatment model, that meets twice weekly for one hour for a period of six to eight weeks. This program serves patients who already understand the basic principles of substance abuse treatment and recovery and patients who do not agree with the 12-step philosophy of AA and NA.
An intervention program for people cited for driving under the influence (DUI) was developed for referrals from the county court. The DUI program is held one evening a week for one and a half hours for 12 weeks.
We developed a specialized program for women veterans, with a recovery group for those early in their treatment and an aftercare support group for those who understand and practice recovery.
An outpatient detoxification clinic was added and staffed by both nurses and physicians.
A domestic violence intervention program was initiated after staff received all the appropriate training. Patients are referred by the county court to complete a 28-week program. A support group is now offered in the posttraumatic stress disorder clinic for patients who also have substance abuse problems.
A preventive-educational service is also offered to other hospital programs and inpatient units that treat patients at high risk for substance abuse, such as inpatient psychiatry wards and the day treatment and homeless programs.
The three aftercare groups that were part of the former program continue to meet once weekly in the evening and daytime.
Figure 1 illustrates the changes made in the program, and lists services offered according to treatment intensity.
Integration of inpatient and outpatient staff
Our old program had a small outpatient team and a large inpatient team. The inpatient component of the old program consisted of two psychiatrists, one nurse practitioner, four addiction counselors, one social worker, eight registered nurses, two nursing assistants, one psychologist, and a unit clerk. The outpatient component consisted of one half-time psychiatrist, two addiction counselors, one clinical nurse specialist, one psychologist, and one administrative program assistant.
The new program brought all the staff into one location. Several staff members were transferred to other services, including one psychologist, one social worker, four registered nurses, and two nursing assistants. These transfers reduced the annual cost of the substance abuse program by $250,000 to $300,000.
Program evaluation and follow-up
A program evaluation questionnaire permitted us to compare patient evaluations of our services before and after the reorganization. No differences were noted in patient satisfaction.
Research has shown that patients who stay in treatment longer do better (6,7,8). In the new program, every patient who graduates from one of our services is scheduled for follow-up with his or her counselor or case manager, initially every two weeks and then monthly for at least one year. The great majority of our patients are also referred to AA or NA and other aftercare activities.
Discussion
By the end of the 1980s, both public and private substance abuse treatment services confronted the need for cost containment, which has profoundly influenced the types of care offered and the clients seen (9). As early as 1990, predictions were made that the federal government and corporations would reduce treatment costs by shifting to intensive outpatient programs and away from inpatient care. The greater emphasis on outpatient services, treatment efficacy, and cost-benefit considerations has already led treatment programs to develop plans to deal with financial cutbacks and phase-out plans if services become financially unsupportable (10).
In 1993 Kunnes (11) noted that treatment costs for substance abuse were rising more rapidly than both the rate of general inflation and the costs of other medical services. To ensure that comprehensive care remained available for all who need it, he recommended that the system be restructured in a way that encourages cost-effectiveness while maintaining accountability and quality of care.
The 1995 mandate to reorganize our VA substance abuse program was initially greeted by staff with considerable anxiety and concern. However, the process of reorganization described here led to a program that was well received by our patients, the referring services, and our team. Our outpatient and residential programs remain very active and are now able to serve at least twice the number of patients per year. A total of 538 patients were served in fiscal year 1995 before the reorganization, compared with 1,299 patients in fiscal year 1996 and 1,148 patients in fiscal 1997, after the reorganization was completed. Patients, staff, and referring colleagues appreciate the lack of waiting lists. Staff are now able to offer program services of various intensities tailored to the special needs of each patient.
The authors are affiliated with the Department of Veterans Affairs James A. Haley Health Care System, 13000 Bruce B. Downs Boulevard, Tampa, Florida 33612 (e-mail, [email protected]), and the department of psychiatry at the University of South Florida in Tampa. Dr. Francis is assistant chief of the mental health and behavioral sciences service and assistant professor, Dr. Hughes is director of the alcohol and drug abuse treatment program and professor, and Dr. Schinka is clinical neuropsychologist and associate professor. Richard J. Frances, M.D., is editor of this column.
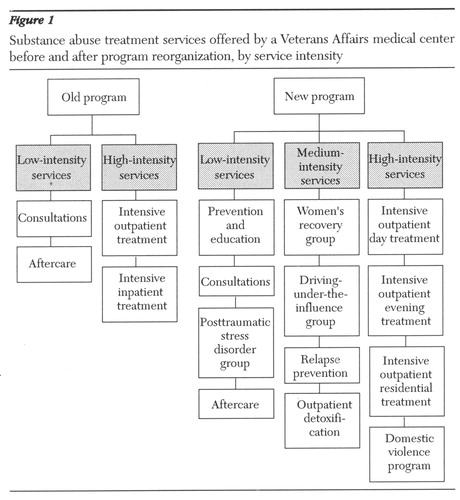
Figure 1. Substance abuse treatment services offered by a Veteran Affairs medical center before and after program reorganization, by service intensity
1. Kizer KW: Vision for Change: A Plan to Restructure the Veterans Health Administration, 1995. Washington, DC, US Government Printing Office, 1995Google Scholar
2. Kizer KW: Prescription for Change: The Guiding Principles and Strategic Objectives Underlying the Transformation of the Veterans Health Care System. Washington, DC, Department of Veterans Affairs, Mar 1996Google Scholar
3. Miller LJ: Providing and improving access to care in VHA. Forum (newsletter of VA health services research and development), Nov 1996, pp 1-4Google Scholar
4. Lehner L, Burgess J Jr, Hults D, et al: Data and information requirements for the Department of Veterans Affairs resource allocation systems. Medical Care 34(suppl 3):MS21-30, 1996Google Scholar
5. Schinka JA, Francis E, Hughes P, et al: Comparative outcomes and costs of inpatient care and supportive housing for substance-dependent veterans. Psychiatric Services 49:946-951, 1998Link, Google Scholar
6. Moos RH, Petit B, Gruber V: Longer episodes of community residential care reduce substance abuse patients' readmission rates. Journal of Studies on Alcohol 56:433-444, 1995Crossref, Medline, Google Scholar
7. Hubbard RL, Marsden ME, Rachal JV, et al: Drug Abuse Treatment. Chapel Hill, NC, University of North Carolina Press, 1989Google Scholar
8. De Leon G: The therapeutic community: status and evolution. International Journal of Addiction 20:823-844, 1985Medline, Google Scholar
9. Schmidt L, Weisner C: Developments in alcoholism treatment, in Recent Developments in Alcoholism: Vol 2: Ten Years of Progress. Edited by Galanter M. New York, Plenum, 1993Google Scholar
10. Wetermeyer J: Substance use disorders: predictions for the 1990s. American Journal of Drug and Alcohol Abuse 18:1-11, 1992Crossref, Medline, Google Scholar
11. Kunnes R, Niven R, Gustafson T, et al: Financing and payment reform for primary health care and substance abuse treatment. Journal of Addictive Diseases 12(2):23-42, 1993Google Scholar



