Outcomes of Four Treatment Approaches in Community Residential Programs for Patients With Substance Use Disorders
Abstract
OBJECTIVE: Treatment approaches used in community residential facilities for patients with substance use disorders were identified, and patients' participation in treatment and case-mix-adjusted one-year outcomes for substance use, symptoms, and functioning in facilities with different treatment approaches were examined. METHODS: A total of 2,376 patients with substance use disorders treated in a representative sample of 88 community residential facilities were assessed at entry to and discharge from the facility and at one-year follow-up. The community residential facilities were classified into four types based on the major emphasis of the treatment program: therapeutic community, psychosocial rehabilitation, 12-step, and undifferentiated. RESULTS: Patients in programs that used the therapeutic community, psychosocial rehabilitation, and 12-step approaches had comparable one-year outcomes in symptoms and functioning that were better than those of patients in undifferentiated programs. A more directed treatment orientation, a longer episode of care, and completion of care were independently related to better one-year outcomes. These findings held for patients with only substance use disorders and for patients with both substance use and psychiatric disorders. CONCLUSIONS: Community residential programs that have a more directed treatment orientation and that motivate patients to complete treatment have better substance use outcomes. As an increasingly important locus of specialized care, community residential facilities need to develop and maintain more differentiated and distinctive treatment orientations.
As proponents of deinstitutionalization planned more than 40 years ago, the locus of active treatment for substance abuse and psychiatric patients has finally moved from the hospital to the community. Community residential programs are an integral part of this development. Although a considerable amount of research has focused on community programs (1,2,3,4,5), more information is needed about the most prevalent treatment orientations in community programs, especially programs for patients with alcohol use disorders, and about these patients' posttreatment outcomes in the areas of substance use and functioning. Some researchers have described treatment models in residential programs (6,7), but these models have been based on the types of services provided rather than on treatment approach or orientation.
We focus here on community residential facilities characterized by one of four treatment orientations: therapeutic community, psychosocial rehabilitation, 12-step, and undifferentiated. We address three questions. First, do patients in community residential facilities with different treatment orientations vary in length of stay and participation in treatment? Second, do patients in community residential facilities with different treatment orientations differ in one-year symptom and functioning outcomes? And, third, are the treatment orientation of the community residential facility and patients' length of stay and level of participation in treatment independently related to patients' one-year outcomes?
Background
The three most prevalent orientations toward residential substance abuse treatment are the therapeutic community model, which reflects principles of personal responsibility and reliance on the community as a therapeutic agent (1,8,9,10,11); the psychosocial rehabilitation model, which emphasizes the development of work and social skills and ways of managing high-risk situations (12,13,14); and the 12-step model, which is based on principles drawn primarily from Alcoholics Anonymous (AA) (15,16).
Therapeutic community, psychosocial rehabilitation, and 12-step programs each have a distinctive, directed treatment orientation. In contrast, some community programs primarily provide residential and meal services and do not follow a defined treatment approach (4). Such undifferentiated or laissez-faire programs typically have only limited counseling services and social activities and are oriented more toward safety and security than active treatment.
Programs with a more directed treatment orientation tend to provide more health and treatment services (17,18) and to encourage patients to participate more intensively in treatment than those with a less directed approach. More specifically, programs with a strong emphasis on psychosocial treatment goals tend to serve patients who are more engaged in program activities, who communicate more with each other, and who are more satisfied with treatment. Patients in these types of programs also are more likely to complete treatment (4,19). In an earlier study of the community residential facilities reported on here, we found that more emphasis on therapeutic community and 12-step treatment orientations was associated with increased participation of patients in counseling services and social activities (20).
Research evidence consistently supports the effectiveness of therapeutic communities (8,9,21,22,23,24) and psychosocial rehabilitation programs (12,13,14), and empirical support for the effectiveness of 12-step treatment is growing (25,26,27). The few existing comparisons between different treatment models have tended to show broadly similar outcomes, especially between 12-step and psychosocial rehabilitation programs. With the exception of studies of therapeutic community programs, however, most previous studies have focused on hospital-based rather than community-based programs.
Some treatment orientations may produce better patient outcomes because they include more intensive services and are more successful at retaining patients and motivating them to participate in the program. Leda and associates (17) found that more intensive psychosocial treatment is associated with a higher proportion of patients returning to independent life in the community, and several studies have shown that longer episodes of community residential treatment are associated with better follow-up outcomes (21,22,23,24,28,29).
One important question is whether specific treatment orientations may be differentially associated with posttreatment outcomes among patients who are more versus less severely disturbed. Highly directed treatment programs that have increased demands and strong expectations for performance may be better suited for higher functioning patients than for more impaired patients (30). More specifically, because the 12-step philosophy focuses on substance use as the primary problem, 12-step programs may be more effective with patients with substance use disorders only and less effective with dually diagnosed patients. To examine this issue, we considered the role of patients' diagnoses in treatment outcome.
Methods
Sample
As part of a prospective longitudinal evaluation, we did an intake assessment of 2,822 patients with substance use disorders who entered one of a representative sample of 88 community residential facilities nationwide during the period from January 1994 to September 1995. These facilities had contracted with the Department of Veterans Affairs (VA) to provide community care for VA patients with substance use disorders. Patients completed an intake information form on admission to the community residential facility, and a staff member completed a discharge checklist when the patient left the facility. Additional information about the overall research project is available elsewhere (20,31).
About 12 months after discharge from the community residential facility, patients were asked to complete a follow-up form that covered the same content as the intake form. Of the 2,822 patients assessed at intake, 65 had died before completion of the one-year follow-up. Complete data were obtained at discharge and at follow-up from 2,376 of the remaining 2,757 patients, or 86 percent of those who were still alive. The VA nationwide inpatient database captured information on patients' clinical diagnoses and inpatient treatment in the year before and the year after admission to residential care in the community.
The patients who were successfully followed were almost all men (99 percent). Fifty-two percent were Caucasian, and 37 percent were African American. On average, they were 42 years old and had completed almost 13 years of education. Only 9 percent were currently married. Sixty-five percent of the patients had only substance use disorder diagnoses, 35 percent had both substance use and psychiatric diagnoses, and 6 percent had only psychotic diagnoses. Thirty-seven percent of the patients had had inpatient substance abuse or psychiatric treatment in the year before the current episode of care. There were no significant differences between the patients who participated in the one-year follow-up and those who did not on any of these variables.
Participation in treatment and one-year outcomes
To measure patients' participation in the community residential facility programs, we obtained information from facility staff on the number of days patients stayed in residential care, on whether patients completed the program, and on patients' involvement in three types of program activities. Participation in counseling and skills training, which included individual counseling, group counseling, social skills training, and work therapy, was measured using 11 items. Self-help activities, including AA and Narcotics Anonymous groups, were measured using three items. Social activities, including physical fitness activities, classes or lectures, and discussion groups, were measured using nine items. Items on these indexes were rated on a 4-point scale ranging from not at all to 11 times or more. To obtain a measure of the intensity of treatment, scores were divided by the number of weeks the patient spent in the program.
We also asked residential facility staff to rate each resident's supportive relationships with other residents, as measured using six items scored on a 5-point scale. These items included questions about whether the resident counts on other residents for help when needed and whether other residents cheer up the resident when he or she is sad or worried (32).
To assess patients' functioning, we used six measures of one-year outcomes. Two measures of substance use outcomes reflected the patient's status in the three months before intake and in the three months before the follow-up. They were abstinence from alcohol and drugs and no problems due to substance use, as indicated by responses of "never" to each of 15 items covering health problems, job problems, legal problems, and so on.
We assessed two psychological outcomes that also reflected the patient's status in the three months before intake and in the three months before the follow-up. The outcome—clinically significant distress—was indicated by responses of "quite a bit" or "extremely" on five or more of the 12 items on the depression and anxiety scales of the Brief Symptom Inventory (BSI) (33), such as "thoughts of ending your life" and "spells of terror or panic." The second outcome—clinically significant psychiatric symptoms—was indicated by responses of "quite a bit" or "extremely" on four or more of the ten items on the BSI paranoid ideation and psychoticism scales, such as "feeling that you are watched or talked about by others" and "the idea that something is wrong with your mind."
The two social outcomes were whether the patient had been arrested in the last year and whether the patient was employed either part time or full time. Both of these outcomes were scored yes or no.
Treatment orientations
To obtain information about the characteristics of the community residential facilities, we asked the manager of each facility to complete the Drug and Alcohol Program Treatment Inventory (DAPTI) (34) and the Policies and Services Characteristics Inventory (PASCI) (35). Five scales were drawn from the DAPTI to identify facilities' orientations toward care. Each scale was composed of eight 4-point items ranging from 0, not like our program, to 3, major part of our program.
The first of the five scales, which measured programs' therapeutic community orientation, focused on the extent to which a program encouraged patients to accept personal responsibility for their decisions and actions and took steps to strengthen patients' sense of self-worth and trust. The second scale measured programs' rehabilitation orientation, or the extent to which the program emphasized the development of better work habits and the acquisition of new job skills. The third scale focused on the 12-step orientation and measured the extent to which the program emphasized helping patients to accept that they are powerless over the abused substance and to work through the 12 steps of AA.
The fourth scale measured programs' psychodynamic orientation, or the extent to which the program focused on increasing patients' understanding of why substance use problems develop and how to establish better interpersonal relationships. The fifth scale focused on the cognitive-behavioral orientation and measured the extent to which the program emphasized developing patients' confidence in coping with high-risk situations and helping them identify alternative responses to using drugs or alcohol.
We defined four types of treatment programs in terms of their standard scores on these scales (mean±SD=50±10). Community residential facilities that scored at the mean or above on the therapeutic community, cognitive-behavioral, psychodynamic, and 12-step indexes were classified as therapeutic community programs (N=25) (see Table 1). Facilities that scored at the mean or above on the rehabilitation and cognitive-behavioral orientations and did not meet criteria for therapeutic community programs were classified as rehabilitation programs (N=21). Facilities that scored at the mean or above on the 12-step orientation and did not meet the criteria for therapeutic community or rehabilitation programs were classified as 12-step programs (N=19). Finally, facilities that did not meet the criteria for therapeutic community, rehabilitation, or 12-step programs were classified as undifferentiated (N=23).
The four types of programs differed predictably in their policies and services. Consistent with their emphasis on personal responsibility, therapeutic community programs were most likely to have resident committees and to involve residents in peer counseling and non-12-step self-help groups (see Table 1). Rehabilitation programs were most likely to provide social and daily living skills training, work therapy, and job counseling. In general, 12-step and undifferentiated programs were less likely to provide each of these types of services.
To examine differences among the four types of community residential facility programs in patients' length of stay and participation in facility-based services and activities, we conducted one-way analyses of variance and Student-Newman-Keuls tests for continuous variables and chi square analyses for the dichotomous variable. We then conducted logistic regression analyses with paired contrasts to examine differences among the four types of community residential facility programs in patients' symptoms and functioning at baseline and one-year follow-up outcomes. The analyses of baseline functioning controlled for patients' age, marital status, and prior treatment, and the analyses of one-year outcomes controlled for these variables as well as for the intake value of the outcome criterion. To adjust for multiple comparisons among program types, we set the significance level for the paired contrasts at p=.008. Finally, we conducted logistic regression analyses to examine the independent effects of the directedness of treatment and patients' participation in treatment on one-year outcomes.
Results
As Table 2 shows, on average, patients in rehabilitation programs had longer episodes of care than did patients in the other three program types. However, patients in therapeutic community programs received the most intensive counseling services. Patients in therapeutic community programs also were most involved in social activities and developed the most supportive relationships with other residents. Patients in undifferentiated programs were least involved in counseling services and social activities, developed less supportive relationships with their peers, and were least likely to complete treatment.
Paired t tests showed that patients in each of the four types of programs improved significantly (p<.05 for all comparisons) between baseline and follow-up on all six one-year outcomes (see Table 3). Patients in therapeutic community, rehabilitation, and 12-step programs had comparable one-year outcomes in all cases. In addition, patients in these three types of programs tended to have better substance use and symptom outcomes than did patients in undifferentiated programs.
Next, we conducted logistic regression analyses to examine the relative importance of treatment orientation and patients' participation in treatment in predicting one-year outcomes. Because therapeutic community, rehabilitation, and 12-step programs had comparable outcomes, we constructed a variable to reflect directive treatment in which patients in these three programs were coded 1 and patients in undifferentiated programs were coded 0. Indexes of program participation other than length of stay and treatment completion were not consistently related to the outcomes and thus were dropped.
Consistent with the results of the initial logistic regression analyses, involvement in a more directive treatment program predicted better one-year outcomes (see Table 4). In addition, a longer episode of care in a community residential facility consistently predicted better outcomes. Patients who completed treatment had better substance use outcomes and were more likely to be employed.
Patients with both substance use and psychiatric diagnoses experienced one-year outcomes comparable to those for patients with only substance use diagnoses in the areas of abstinence, substance use problems, and arrests. As expected, however, the dually diagnosed patients had poorer outcomes on distress, psychiatric symptoms, and employment. None of the interactions between patients' diagnoses and the directedness or length of stay in the community residential facility were significant.
Discussion
We described four distinct treatment orientations in community residential facilities that were characterized by predictable differences in patients' participation in treatment and one-year outcomes.
Patients in therapeutic community programs had the most intensive care, and patients in rehabilitation programs had the longest episodes of treatment. These findings are consistent with those of earlier studies showing that more structured and directed programs enhance patients' involvement in care (17,18). The findings extend prior work by showing that patients in more structured programs engage in more social activities and develop more supportive relationships with their peers. In turn, patients who participate more intensively in counseling and social activities are more likely to complete treatment and to engender staff confidence in their eventual positive outcomes (20,24).
A substantial percentage of the community residential facilities in this study—about 25 percent—had undifferentiated programs that did not emphasize any specific treatment approach. Patients who entered these programs were treated less intensively, and, in fact received less than half the number of counseling sessions than patients in therapeutic community programs received. In addition, they were less involved in social activities in the facility, established less supportive relationships with other residents, and were less likely to complete treatment. Previous studies have shown that patients in less cohesive and structured programs are more likely to drop out of treatment (4).
Consistent with earlier comparisons of alternative treatment models (25,26,27), patients in therapeutic community, rehabilitation, and 12-step treatment experienced comparable one-year outcomes. More important, patients in programs with any one of the three directed treatment orientations had better outcomes than did patients in undifferentiated programs. These findings support the idea that a strong emphasis on a specific treatment orientation may improve the longer-term outcomes of patients with substance use disorders, partly because it is associated with patients' participation in program activities and better outcomes at discharge (20,31).
Longer episodes of care in community residential facilities and completion of the facility's program were associated with better one-year outcomes, even after considering the influence of treatment orientation. These findings extend earlier work (28,29) by showing that both the directedness of treatment and patients' participation in and completion of treatment independently predict better substance use and psychosocial outcomes. Once the analysis controlled for directedness and length of stay, the intensity of treatment had little or no association with one-year outcomes. Thus the duration and continuity of treatment may be more closely related to outcome than is its intensity (36,37).
Dually diagnosed patients' substance use outcomes were comparable to those for patients with only substance use disorders; however, they showed poorer psychological outcomes and were less likely to be employed. These findings are consistent with those of several earlier studies (38,39,40). Contrary to expectations from some earlier work (4,30), dually diagnosed patients did not do worse in more active models of care (41). These findings may reflect the fact that more severely impaired patients were referred for inpatient care and thus were not represented in our sample. Previous studies have shown generally comparable relationships between the length of stay in a community residential facility and readmission outcomes among patients with only substance use disorders and among dually diagnosed patients (28,29).
Several limitations of this project should be noted. Most important, because patients were not randomly assigned to community residential facilities, clinicians' referral patterns or self-selection may have led more highly motivated patients to enter more directive programs. We also relied on managers' reports of their program's treatment orientation rather than on observers' independent ratings. However, the large and representative sample, adjustment for case-mix, and high follow-up rate bolster confidence in the findings. Nevertheless, the findings are based on data for a sample composed primarily of men in one system of care and may not generalize to women, younger patients, or patients with more acute and severe psychiatric disorders.
Conclusions
Overall, our findings imply that the presence of a strong treatment orientation is more closely associated with patients' participation in treatment and treatment outcome than is the particular theory underlying that orientation (42). To reduce the high percentage of patients who drop out of treatment, managers of community residential facilities need to promote a strong psychosocial treatment orientation, communicate high expectations for patients' continuation in treatment, and recognize that participation in the treatment program is a function of patients' relationships with staff and experiences in the program as well as a function of their initial motivation. To strengthen the emphasis on psychosocial treatment, staff can use the DAPTI (34) and PASCI (35) to understand and improve their program's treatment milieu and thereby to enhance patients' motivation to complete treatment and patients' longer-term treatment outcomes.
Acknowledgments
This project was supported by the Department of Veterans Affairs Mental Health Strategic Health Group and the Health Services Research and Development Service of the Office of Research and Development. The authors thank Elizabeth Burnett, B.A., Melissa King, M.P.H., and Michael Patterson, B.A., for help in data collection, and John Finney, Ph.D., Paige Crosby Ouimette, Ph.D., Jeanne Schaefer, Ph.D., and Christine Timko, Ph.D., for their comments on an earlier draft of the manuscript.
The authors are affiliated with the Program Evaluation and Resource Center and Center for Health Care Evaluation of the Department of Veterans Affairs Health Care System and Stanford University Medical Center in Palo Alto, California. Address correspondence to Dr. Moos at the Center for Health Care Evaluation (152), VA Health Care System, 3801 Miranda Avenue, Palo Alto, California 94304 (e-mail, [email protected]).
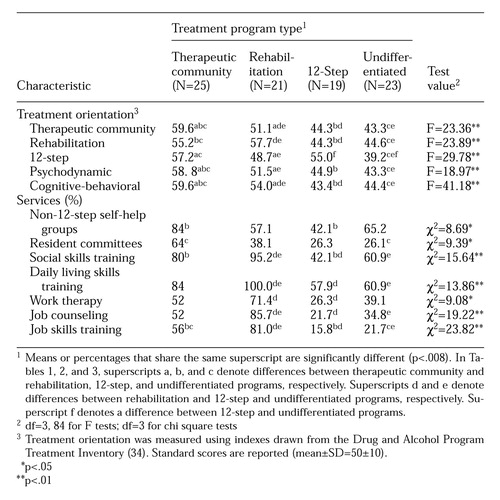 |
Table 1. Treatment orientation and services offered in four types of treatment programs in 88 community residential facilities serving patients with substance use disorders treated in the Veterans Affairs health care system
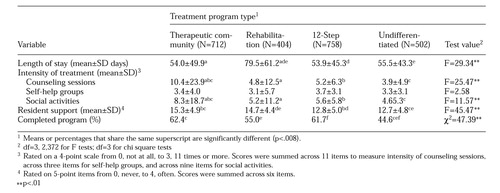 |
Table 2. Patients' length of stay and level of participation in treatment in four types of treatment programs in community residential facilities serving patients with substance use disorders (N=2,376)
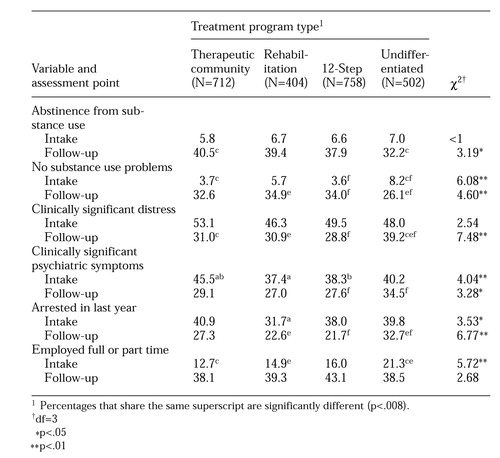 |
Table 3. Symptoms and functioning at intake and one-year follow-up of patients in four types of treatment programs in community residential facilities serving patients with substance use disorders (N=2,376), in percentage of patients
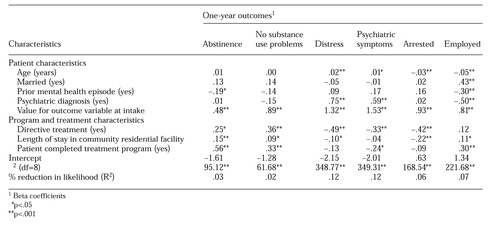 |
Table 4. Logistic regression analyses of the relationship between characteristics of patients and treatment programs in community residential facilities and patients' one-year outcomes in symptoms and functioning (N=2,376)
1. De Leon G, Ziegenfuss JT Jr: Therapeutic Communities for Addictions. Springfield, Ill, Thomas, 1986Google Scholar
2. Hubbard RL, Marsden ME, Rachal JV, et al: Drug Abuse Treatment: A National Study of Effectiveness. Chapel Hill, University of North Carolina Press, 1989Google Scholar
3. Lehman AF, Slaughter JG, Myers CP: Quality of life in alternative residential settings. Psychiatric Quarterly 62:35-49, 1991Crossref, Medline, Google Scholar
4. Moos R: Evaluating Treatment Environments: The Quality of Psychiatric and Substance Abuse Programs. New Brunswick, NJ, Transaction, 1997Google Scholar
5. Simpson DD, Joe GW, Broome KM, et al: Program diversity and treatment retention rates in the Drug Abuse Treatment Outcome Study (DATOS). Psychology of Addictive Behaviors 11:279-293, 1997Crossref, Google Scholar
6. Etheridge RM, Hubbard RL, Anderson J, et al: Treatment structure and program services in the Drug Abuse Treatment Outcome Study (DATOS). Psychology of Addictive Behaviors 11:244-260, 1997Crossref, Google Scholar
7. Randolph FL, Ridgway P, Carling PJ: Residential programs for persons with severe mental illness: a nationwide survey of state-affiliated agencies. Hospital and Community Psychiatry 42:1111-1115, 1991Abstract, Google Scholar
8. Bale R, Zarcone V, Van Stone W, et al: Three therapeutic communities: process and outcome in a prospective controlled study of narcotic addiction treatment. Archives of General Psychiatry 41:185-191, 1984Crossref, Medline, Google Scholar
9. Barr H: Outcome of drug abuse treatment in two modalities, in Therapeutic Communities for Addictions. Edited by De Leon G, Ziegenfuss JT Jr. Springfield, Ill, Thomas, 1986Google Scholar
10. Burda PC, Starkey TW, Dominguez F, et al: A biopsychosocial approach to the chronic psychiatric patient. VA Practitioner 8:55-60, 1991Google Scholar
11. Willer BS: Individualized patient programming: an experiment in the use of evaluation and feedback for hospital psychiatry. Evaluation Quarterly 1:587-608, 1977Crossref, Google Scholar
12. Platt JJ: Vocational rehabilitation of drug abusers. Psychological Bulletin 117:416-433, 1995Crossref, Medline, Google Scholar
13. Bell M, Ryan E: Integrating psychosocial rehabilitation into the hospital psychiatric service. Hospital and Community Psychiatry 35:1017-1023, 1984Abstract, Google Scholar
14. Campanelli PC, Sacks JY, Heckart K, et al: Integrating psychiatric rehabilitation within a community residence framework. Psychosocial Rehabilitation Journal 16(1):135-153, 1992Google Scholar
15. Cahn S: Alcoholism halfway houses: relationships to other programs and facilities. Social Work 14:50-60, 1969Google Scholar
16. McCrady BS: Alcoholics Anonymous and behavior therapy: can habits be treated as diseases? Can diseases be treated as habits? Journal of Consulting and Clinical Psychology 62:1159-1166, 1994Google Scholar
17. Leda C, Rosenheck R, Fontana A: Impact of staffing levels on transitional residential treatment programs for homeless veterans. Psychosocial Rehabilitation Journal 15(1):55-67, 1991Google Scholar
18. Moos R, Pettit E, Gruber V: Characteristics and outcomes of three models of community residential care for substance abuse patients. Journal of Substance Abuse 7:99-116, 1995Medline, Google Scholar
19. Kruzich J, Kruzich S: Milieu factors influencing patients' integration into community residential facilities. Hospital and Community Psychiatry 36:378-382, 1985Abstract, Google Scholar
20. Moos R, King M, Burnett E, et al: Community residential program policies, services, and treatment orientations influence patients' participation in treatment. Journal of Substance Abuse 9:171-187, 1997Crossref, Medline, Google Scholar
21. Condelli WS, Hubbard R: Relationship between time spent in treatment and client outcomes from therapeutic communities. Journal of Substance Abuse Treatment 11:25-33, 1994Crossref, Medline, Google Scholar
22. Hubbard RL, Craddock SG, Flynn PM, et al: Overview of 1-year follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychology of Addictive Behaviors 11:261-278, 1997Crossref, Google Scholar
23. McLellan AT, Childress AR, Griffith J, et al: The psychiatrically severe drug abuse patient: methadone maintenance or therapeutic community? American Journal of Drug and Alcohol Abuse 10:77-95, 1984Google Scholar
24. Simpson DD, Joe GW, Brown BS: Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychology of Addictive Behaviors 11:294-307, 1997Crossref, Google Scholar
25. McLellan AT, Grissom GR, Brill P, et al: Private substance abuse treatments: are some programs more effective than others? Journal of Substance Abuse Treatment 10:243-254, 1993Google Scholar
26. Project Match Research Group: Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol 58:7-29, 1997Crossref, Medline, Google Scholar
27. Ouimette P, Finney J, Moos R: Twelve-step and cognitive-behavioral treatment for substance abuse: a comparison of treatment effectiveness. Journal of Consulting and Clinical Psychology 65:220-234, 1997Crossref, Google Scholar
28. Moos R, Moos B: Stay in residential facilities and mental health care as predictors of readmission for patients with substance use disorders. Psychiatric Services 46:66-72, 1995Link, Google Scholar
29. Moos R, Pettit E, Gruber V: Longer episodes of community residential care reduce substance abuse patients' readmission rates. Journal of Studies on Alcohol 56:433-443, 1995Crossref, Medline, Google Scholar
30. Timko C, Moos R, Finney J: Models of matching patients and treatment programs, in New Directions in Person-Environment Psychology, 2nd ed. Edited by Craik K, Price R, Walsh WB. Hillsdale, NJ, Erlbaum, in pressGoogle Scholar
31. Moos R, King M: Participation in community residential treatment and substance abuse patients' outcomes at discharge. Journal of Substance Abuse Treatment 14:71-80, 1997Crossref, Medline, Google Scholar
32. Moos R, Moos B: Life Stressors and Social Resources Inventory Manual. Odessa, Fla, Psychological Assessment Resources, 1994Google Scholar
33. Derogatis L: Brief Symptom Inventory: Administration, Scoring, and Procedures Manual, 3rd ed. Minneapolis, National Computer Systems, 1993Google Scholar
34. Swindle R, Peterson K, Paradise M, et al: Measuring program treatment orientations: the Drug and Alcohol Treatment Inventory. Journal of Substance Abuse 7:61-77, 1995Medline, Google Scholar
35. Timko C: Policies and services in residential substance abuse programs: comparisons with psychiatric programs. Journal of Substance Abuse 7:43-59, 1995Crossref, Medline, Google Scholar
36. Finney J, Moos R: Psychosocial treatment for alcohol use disorders, in A Guide to Treatments That Work. Edited by Nathan P, Gorman JM. New York, Oxford University Press, 1997Google Scholar
37. Ouimette PC, Moos R, Finney, J: Influence of outpatient treatment and 12-step group involvement on one-year substance abuse treatment outcomes. Journal of Studies on Alcohol 59:513-522, 1998Crossref, Medline, Google Scholar
38. Moos R, Brennan P, Mertens J: Diagnostic subgroups and predictors of one-year readmission among late-middle-aged and older substance abuse patients. Journal of Studies on Alcohol 55:173-183, 1994Crossref, Medline, Google Scholar
39. Ouimette PC, Ahrens C, Moos R, et al: Posttraumatic stress disorder in substance abuse patients: relationships to 1-year posttreatment outcomes. Psychology of Addictive Behaviors 11:34-47, 1997Crossref, Google Scholar
40. Rounsaville BJ, Dolinsky ZS, Babor TF, et al: Psychopathology as a predictor of treatment outcome in alcoholics. Archives of General Psychiatry 44:505-513, 1987Crossref, Medline, Google Scholar
41. Nuttbrock L, Rahav M, Rivera J, et al: Mentally ill chemical abusers in residential treatment programs: effects of psychopathology on levels of functioning. Journal of Substance Abuse Treatment 14:269-274, 1997Crossref, Medline, Google Scholar
42. Luborsky L, Crits-Christoph P, Mintz J, et al: Who Will Benefit From Psychotherapy? Predicting Therapeutic Outcomes. New York, Basic Books, 1988Google Scholar



