Relationship of Depression Screening and Physician Office Visit Duration in a National Sample
Major depressive disorder is a common, debilitating chronic illness with a lifetime prevalence of 16.2% and a 12-month prevalence of 6.6% in the U.S adult population ( 1 ). General depressive symptoms have been reported to have a lifetime prevalence affecting nearly one-fourth (23.1%) of U.S. adults ( 2 ). In 2000, the World Health Organization ranked depression as the fourth leading contributor to global burden of disease ( 3 ). In a study of 13 chronic conditions, only depression was associated with workplace attendance (presence and absence) and with critical incidents (such as job-related accidents, injuries, and other negative events) ( 4 ). As a common comorbidity, depression adds to the burden of many chronic disease states ( 5 , 6 , 7 , 8 , 9 , 10 ). Studies examining the costs of depression among U.S. workers have shown that employees with depression cost businesses $31 billion annually in lost productive time compared with peers without depression ( 11 ) and $51.5 billion in total workplace costs ( 12 ).
Given the high prevalence of depression and its adverse impact on medical expenditures and patient quality of life, one would expect that adequate detection and treatment would be key concerns among primary care providers ( 13 ). However, despite the consequences, depression often is unrecognized by physicians in a large proportion of patients ( 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 ). After reviewing available evidence and beginning in their 2002 recommendations ( 22 ), the U.S. Preventive Services Task Force (USPSTF) endorsed depression screening for adults (recommendation grade B) in primary care settings that have adequate systems to ensure accuracy of diagnosis, management, and treatment of the illness ( 23 ).
Although the USPSTF guidelines are well intended, the provision of preventive services may substantially add to the duration of physician visits. For example, a study examining primary care preventive services recommended by the 1996 USPSTF guidelines reported that absolute physician adherence to all recommendations and guidelines would increase a physician's workday by 7.4 hours ( 24 ). Other research examining USPSTF guidelines has found that, in general, preventive services add an average of 2.1 minutes per visit ( 25 ), with some services adding over five minutes to visit duration ( 26 ). A cost-utility analysis of depression screening before the implementation of the 2002 USPSTF recommendations estimated that depression screening added approximately six minutes to physician office visits when a nurse administered and a physician scored a depression screening instrument ( 27 ). However, the time necessary to conduct depression screening varies depending on the instrument and technique used, with no standard method endorsed by USPSTF.
The objective of this study was to evaluate the relationship between depression screening and duration of patients' visits with their primary care physician in a nationally representative sample of office visits. Quantifying differences in duration of physician visits with respect to use of depression screening while controlling the analyses for other factors that may influence physician time burden should provide evidence for policy makers as they consider actions to ensure that patients are routinely screened for depression and that facilitate optimal adherence to USPSTF guidelines.
Methods
Study design and overview
Patient and visit characteristics from a nationally representative sample of community-based family, general, and internal medicine primary care physicians' office visits were used to evaluate the relationship between depression screening and office visit duration.
Data source. Cross-sectional data from the 2005–2007 National Ambulatory Medical Care Survey (NAMCS) were used ( 28 ). The NAMCS is a national survey conducted by the National Center for Health Statistics of patient visits to non-federally employed, office-based physicians primarily engaged in direct patient care. The survey uses a three-stage probability design of primary sampling units, physicians' practices within those units, and patient visits within physicians' practices. Each visit is weighted by sampling probability, adjustment for nonresponse, physician specialty, and geographic location to obtain nationally representative estimates. These estimates were considered reliable if they had a standard error of 30% or less and if they were achieved with a sample of no fewer than 30 patient visits ( 28 ). This study was exempt from review by the University of Oklahoma Institutional Review Board because it used publicly available, deidentified data.
Inclusion and exclusion criteria. The 2005–2007 NAMCS data contained 87,835 unique visits. The USPSTF depression screening guidelines target adult patients of primary care physicians. Therefore, data were limited to visits including adult patients (≥18 years) of general and family practices and internal medicine physicians indicated to be the patient's primary care physician. We excluded from analysis visits with primary-reason-for-visit codes related to injuries, adverse effects, or test results; visits coded as administrative (examinations for unemployment, licensing, Social Security disability, and so on); and visits that were uncodable (that is, there was insufficient information). Because this study focused on physician time burden, visits indicating presence of nonphysician clinicians (such as nurse practitioners or physician assistants) were excluded from the analytical sample. Visit time outliers were eliminated by restricting visit time to a range from one to 60 minutes. Because only visits with complete data were analyzed in multivariable analyses, all visits containing variables of interest coded as missing were excluded, leaving a final analytical sample of 14,736 family, general, and internal medicine primary care adult office visits in the United States between 2005 and 2007.
Study variables. The dependent measure of interest was duration of physician time spent with a patient for a particular visit. Time spent with physicians is defined in the NAMCS data documentation as the amount of time (in minutes) that a physician spent with the patient, not including time spent waiting for an appointment or with another type of practitioner ( 28 ). Although defined as a continuous variable, the distribution of time spent with a physician in the NAMCS data was largely recorded in increments of five minutes of visit duration (five minutes, ten minutes, 15 minutes, and so on). To preserve the nature of the data while balancing the need for adequate sample sizes to achieve reliable estimates in data analysis, we defined the duration of time spent with a physician at an office visit as an ordinal measure of four 15-minute time increments (that is, one to 15 minutes, 16–30 minutes, 31–45 minutes, and 46–60 minutes). Prior analyses that have examined physician time using NAMCS data ( 26 , 29 ) dichotomized the time variable at the median visit duration. However, an ordered measure provides a more precise estimate of the associations between depression screening and physician time while respecting the analytical assumption of the nonnormal distribution of the data.
Several patient characteristics were used as control variables in the multivariable analysis. Age was dichotomized as patients aged 65 or older or those younger than 65. Race-ethnicity was defined as white non-Hispanic or "other" (including black non-Hispanic, Hispanic, Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaska Native, or people of multiple races or ethnicities). The NAMCS documents 14 common chronic conditions, regardless of the diagnosis associated with that specific visit. Given its suspected relationship with depression screening, a diagnosis of depression (yes or no) was included as a separate control variable in the analyses. Of the 13 remaining possible, chronic conditions, the sum of the total number of chronic conditions was dichotomized as patients with more than the median number of chronic conditions or those with the median number or fewer.
Several visit characteristics were also suspected to be related to visit duration. An indicator variable was created to document the number of prior visits a patient had made to the sampled physician in the previous 12 months. This variable was dichotomized as patients with up to two prior visits versus those with three or more prior visits. Primary payment type was defined as private insurance, Medicare, Medicaid, or other, which included worker's compensation, self-pay, no charge, other, or unknown. The NAMCS data also document the order for or provision of numerous diagnostic or screening tests. The independent variable of primary interest in this study was order for or provision of depression screening documented in the patient medical record. Depression screening was defined separately from the other diagnostic and screening tests by a dichotomous variable (yes or no). Because the data collected in the NAMCS regarding diagnostic and screening tests are limited to the description of "order for or provision of" a given test, the meaning of the term "depression screening" as used in this study was defined as physician intent to screen the patient for depression.
All other diagnostic and screening tests were collapsed into a single dichotomous variable indicating at least one test versus no tests. Measurements of vital signs, height, and weight were not included as diagnostic tests in the analysis because they are standard practice at family, general, and internal medicine primary care visits. The order for or provision of health education at a visit was dichotomized as yes or no. A final indicator variable for visit type was used to identify an acute care, chronic care (including routine and flare-up chronic care), or preventive care visit.
Analysis
Univariate descriptive statistics were calculated to profile the study sample. Ordered logistic regression was used to evaluate the relationship between depression screening and primary care physician visit duration while controlling for important covariates in a multivariable model. Predicted probabilities were calculated from the multivariable ordered logistic regression to assess the distribution of visit duration time intervals stratified by visits with and without depression screening. To provide population estimates, all data management and analyses were performed in Stata, version 10.1 ( 30 ), with complex survey commands using Taylor-linearized variance estimation, sampling weights, and masked sampling design variables provided in the NAMCS data set ( 31 ). An a priori alpha level of .05 was the criterion for statistical significance.
Results
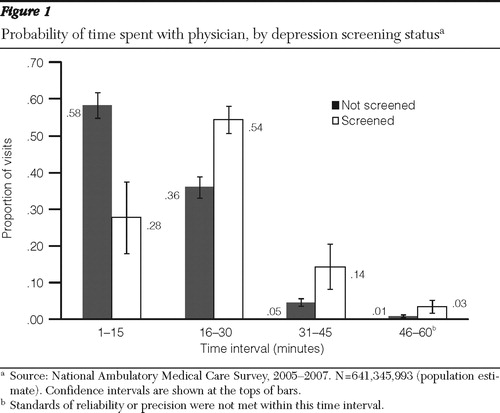
A total of 14,736 complete, community-based adult visits to family, general, and internal medicine primary care physicians were analyzed from the 2005–2007 NAMCS data set, which represented 641,345,993 visits nationally ( Table 1 ). Henceforth, all results are presented and discussed at the population level. Overall, most visits were from one to 15 minutes long (56.1%). The distribution of visit duration was positively skewed, with a median visit time of 15 minutes. Depression screening was documented at 3.4% of visits.
 |
Several variables were associated with longer visit duration in the ordered logistic regression model ( Table 1 ). Most important, depression screening at a visit was associated with significantly higher odds of having a longer visit duration compared with visits not involving depression screening (adjusted odds ratio=3.66).
Subsequent to the primary analysis, the dependent variable, visit duration, was specified and tested in a number of ways in several multivariable post hoc analyses using an identical set of independent variables from the primary analysis and the same complex survey commands. Results of a multivariable linear regression analysis using physician visit duration (in minutes) as a continuous dependent variable demonstrated no variation in results compared with results presented in Table 1 . Multivariable models using log-linear, square root, and squared transformations of the continuous dependent variable also demonstrated no variation in results when compared with the ordered logistic model. It is important to note that none of these techniques normalized the distribution of the visit duration variable. Finally, to compare this study's results with prior NAMCS studies examining physician visit duration, the dependent variable was dichotomized at its median of 15 minutes in a logistic regression model. With the exception of number of prior visits in the previous 12 months (p=.184), the interpretation of results did not vary from the primary analysis using the ordered dependent variable.
The distribution of the probability of a physician visit in a given time interval estimated from the ordered logistic regression demonstrates differing patterns of visit duration when stratified by visits with and without depression screening while holding other independent variables at their sample means ( Figure 1 ). Whereas 27.7% of depression screening visits occurred in the one- to 15-minute interval, 58.4% of nonscreening visits occurred in this time interval. However, this relationship subsequently reversed, with higher proportions of visits including depression screening at longer visits.
Discussion
This research sought to evaluate the relationship between depression screening and physician visit duration. Depression screening was found to be independently associated with an increased time burden on primary care physicians after controlling analyses for other factors that may contribute to physician visit duration. Although this result is not surprising, time burden is often overlooked by policy makers when proposing new disease identification and management guidelines.
The U.S. Department of Health and Human Services has acknowledged that primary care providers have little incentive to perform mental health screenings ( 32 ), and research has shown that physicians may deliberately misdiagnose major depressive disorder in patients' medical records for reasons of reimbursement ( 33 ). Without efficient mechanisms to facilitate depression screening in primary care, physicians may not be able to adequately provide this service. Therefore, well-intended, evidence-based guidelines may not be fully implemented and optimized. The shame and stigma associated with mental disorders may also discourage many individuals from seeking care ( 34 ); therefore, a proactive effort by health care providers is of the utmost importance.
Given the additional physician time burden and costs associated with depression screening, alternative methods for implementation warrant continued study. Research examining potential strategies to facilitate and integrate cost-effective depression screening within the current structure of the primary care system is needed. Alternative and accessible community health care providers such as pharmacists may be well positioned to screen and refer patients who are at risk of a depressive disorder. Other promising mechanisms include computerized screening kiosks in physicians' offices, which were recently described in a study of an electronic version of the nine-item Patient Health Questionnaire ( 35 ). Such devices likely will save personnel time and deliver real-time screening results to patients' physicians.
Because depression is a highly prevalent comorbidity that adversely affects the management of other disease states and generates excess financial costs ( 36 ), the USPSTF determined depression screening to be an appropriate method for improving depression treatment. Despite these guidelines, there is no consensus on the feasibility and implementation of depression screening for the general population. In 2001–2002, a study using simulated models to analyze the cost utility of depression screening found that regular screening could incur costs in excess of $50,000 per quality-adjusted life year ( 27 , 37 ). Although the study concluded that more effective therapies and efficient treatment protocols may improve the cost utility of depression screening, we are unaware of any controlled studies examining both the actual costs and consequences of implemented depression screening programs subsequent to the publication of the 2002 USPSTF depression screening guidelines. Thus, to more fully understand depression screening practices in primary care, there is a critical need for research examining the real-world implementation of depression screening programs. Important domains that should be studied include efficient use of personnel, providers, and technology; patient disposition into treatment; and subsequent patient outcomes.
There were several limitations to this study. As is common with survey methodology, data gathering was subject to recording and transcribing errors. The cross-sectional data collected through the NAMCS precludes consideration of direct causation between depression screening and physician visit duration. Although adjustments were made to account for the complex survey procedure of the NAMCS, results are only estimates. Publicly available NAMCS data files contain masked sampling unit and strata markers to protect patient privacy. Compared with the use of unmasked markers, the masking procedure decreases the precision of error estimates when weighting is applied to correct for the complex nature of the NAMCS survey data. However, internal testing by National Center for Health Statistics staff has indicated that standard errors produced with masked markers may tend to slightly overestimate error terms ( 31 ), therefore yielding a more conservative statistical analysis.
Measures from diagnostic and screening tests, including depression screening, as well as health education, do not directly address whether those services were provided at the office visits or simply ordered by the physician. Nonetheless, a documented intent to screen for depression was associated with increased duration of visit. The NAMCS has been found to accurately document diagnostic tests but to underestimate behavioral counseling ( 38 , 39 ); however, such studies occurred before the implementation of the depression screening variable in data collection and thus cannot be extrapolated to the accuracy of screening documentation. In addition, this study included only visits where physicians were seen and excluded nonphysician clinicians. In offices with multiple types of practitioners, physicians may see sicker patients with more complex case histories, which therefore may affect depression screening rates.
Because of a smaller number of visits that lasted from 46 to 60 minutes, some cells in bivariate cross-tabulations contained fewer than 30 observations. Although this may lead to instability in statistical analysis, this time interval was not of direct importance to the results of this study; the shift from visits of one to 15 minutes to those of 16–30 minutes was not limited by sample size. Although it has been reported that the NAMCS may overestimate visit duration ( 38 , 39 ), this study sought only to examine the relationship of depression screening and visit duration. A consistent overestimation in visit duration should not affect the significant pattern of relationships found in this study. In addition, a post hoc multivariable model (results not shown) excluding visits where visit duration was imputed by the National Center for Health Statistics staff did not change the interpretation of results.
Although several potential covariates were included in the multivariable analysis, additional factors unaccounted for, such as physician characteristics and practice patterns not captured in the publicly available NAMCS data, may have influenced the relationship between physician visit time and depression screening. For example, physicians who spend more time with patients may conduct more thorough patient examinations and may be the type of physician who screens for depression. Therefore, analysis of physician practice patterns represents an important area of future research to identify factors associated with successful depression screening programs in primary care physicians' practices.
Conclusions
Depression screening is a recommended practice in primary care settings to triage patients into depression treatment. This study demonstrated that depression screening was associated with extended physician office visit duration. Future research examining both the costs and consequences of depression screening using formal cost-effectiveness or cost-benefit analysis for novel comparator strategies (using technology or personnel other than physicians to conduct screenings) are warranted to determine appropriate strategies that facilitate more complete implementation of efficient depression screening programs.
Acknowledgments and disclosures
The authors report no competing interests.
1. Kessler RC, Berglund P, Demler O, et al: The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 289:3095–3105, 2003Google Scholar
2. Johnson J, Weissman MM, Klerman GL: Service utilization and social morbidity associated with depressive symptoms in the community. JAMA 267:1478–1483, 1992Google Scholar
3. Depression, Mental Health. Geneva, World Health Organization. Available at www.who.int/mental_health/management/depression/definition/en . Google Scholar
4. Wang PS, Beck A, Berglund P, et al: Chronic medical conditions and work performance in the Health and Work Performance Questionnaire Calibration Surveys. Journal of Occupational and Environmental Medicine 45:1303–1311, 2003Google Scholar
5. Bisschop MI, Kriegsman DMW, Deeg DJH, et al: The longitudinal relation between chronic diseases and depression in older persons in the community: the Longitudinal Aging Study Amsterdam. Journal of Clinical Epidemiology 57:187–194, 2004Google Scholar
6. Ciechanowski PS, Katon WJ, Russo JE: Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Archives of Internal Medicine 160:3278–3285, 2000Google Scholar
7. Egede LE: Effect of comorbid chronic diseases on prevalence and odds of depression in adults with diabetes. Psychosomatic Medicine 67:46–51, 2005Google Scholar
8. Evans DL, Charney DS, Lewis L, et al: Mood disorders in the medically ill: scientific review and recommendations. Biological Psychiatry 58:175–189, 2005Google Scholar
9. Moussavi S, Chatterji S, Verdes E, et al: Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370:851–858, 2007Google Scholar
10. Rudisch B, Nemeroff CB: Epidemiology of comorbid coronary artery disease and depression. Biological Psychiatry 54:227–240, 2003Google Scholar
11. Stewart WF, Ricci JA, Chee E, et al: Cost of lost productive work time among US workers with depression. JAMA 289:3135–3144, 2003Google Scholar
12. Greenberg PE, Kessler RC, Birnbaum HG, et al: The economic burden of depression in the United States: how did it change between 1990 and 2000? Journal of Clinical Epidemiology 64:1465–1475, 2003Google Scholar
13. Goldman LS, Nielsen NH, Champion HC: Awareness, diagnosis, and treatment of depression. Journal of General Internal Medicine 14:569–580, 1999Google Scholar
14. Gerber PD, Barrett J, Manheimer E, et al: Recognition of depression by internists in primary care: a comparison of internist and "gold standard" psychiatric assessments. Journal of General Internal Medicine 4:7–13, 1989Google Scholar
15. Jones LR, Badger LW, Ficken RP, et al: Inside the hidden mental health network: examining mental health care delivery of primary care physicians. General Hospital Psychiatry 9:287–293, 1987Google Scholar
16. Nielsen AC, Williams TA: Depression in ambulatory medical patients: prevalence by self-report questionnaire and recognition by nonpsychiatric physicians. Archives of General Psychiatry 37:999–1004, 1980Google Scholar
17. Ormel J, Van Den Brink W, Koeter MW, et al: Recognition, management and outcome of psychological disorders in primary care: a naturalistic follow-up study. Psychological Medicine 20:909–923, 1990Google Scholar
18. Schulberg HC, Saul M, McClelland M, et al: Assessing depression in primary medical and psychiatric practices. Archives of General Psychiatry 42:1164–1170, 1985Google Scholar
19. Simon GE, Von Korff M: Recognition, management, and outcomes of depression in primary care. Archives of Family Medicine 4:99–105, 1995Google Scholar
20. Von Korff M, Shapiro S, Burke JD, et al: Anxiety and depression in a primary care clinic: comparison of Diagnostic Interview Schedule, general health questionnaire, and practitioner assessments. Archives of General Psychiatry 44:152–156, 1987Google Scholar
21. Wells KB, Hays RD, Burnam MA, et al: Detection of depressive disorder for patients receiving prepaid or fee-for-service care. Results from the Medical Outcomes Study. JAMA 262:3298–3302, 1989Google Scholar
22. Pignone MP, Gaynes BN, Rushton JL, et al: Screening for depression in adults: a summary of the evidence for the US Preventive Services Task Force. Annals of Internal Medicine 136:765–776, 2002Google Scholar
23. US Preventive Services Task Force: Screening for depression: recommendations and rationale. Annals of Internal Medicine 136:760–764, 2002Google Scholar
24. Yarnall KSH, Pollak KI, Østbye T, et al: Primary care: is there enough time for prevention? American Journal of Public Health 93:635–641, 2003Google Scholar
25. Stange KC, Flocke SA, Goodwin MA: Opportunistic preventive services delivery: are time limitations and patient satisfaction barriers? Journal of Family Practice 46:419–424, 1998Google Scholar
26. Pollak KI, Krause KM, Yarnall KSH, et al: Estimated time spent on preventive services by primary care physicians. BMC Health Services Research 8:245, 2008Google Scholar
27. Valenstein M, Vijan S, Zeber JE, et al: The cost-utility of screening for depression in primary care. Annals of Internal Medicine 134:345–360, 2001Google Scholar
28. 2007 National Ambulatory Medical Care Survey (NAMCS) micro-data file documentation. Hyattsville, Md, National Center for Health Statistics, 2007Google Scholar
29. Coco A, Mainous AG: Relation of time spent in an encounter with the use of antibiotics in pediatric office visits for viral respiratory infections. Archives of Pediatrics and Adolescent Medicine 159:1145–1149, 2005Google Scholar
30. Stata Statistical Software, Version 10. College Station, Tex, Stata Corp, 2007Google Scholar
31. Using Ultimate Cluster Models With NAMCS and NHAMCS Public Use Files. Hyattsville, Md, Centers for Disease Control and Prevention, National Center for Health Statistics, 2004. Available at www.cdc.gov/nchs/data/ahcd/ultimatecluster.pdf Google Scholar
32. Mauch D, Kautz C, Smith S: Reimbursement of Mental Health Services in Primary Care Settings. Rockville, Md, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, 2008Google Scholar
33. Rost K, Smith GR, Matthews DB, et al: The deliberate misdiagnosis of major depression in primary care. Archives of Family Medicine 3:333–337, 1994Google Scholar
34. Barney LJ, Griffiths KM, Jorm AF, et al: Stigma about depression and its impact on help-seeking intentions. Australian and New Zealand Journal of Psychiatry 40:51–54, 2006Google Scholar
35. Fann JR, Berry DL, Wolpin S, et al: Depression screening using the Patient Health Questionnaire–9 administered on a touch screen computer. Psycho-oncology 18:14–22, 2009Google Scholar
36. Katon WJ: Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biological Psychiatry 54:216–226, 2003Google Scholar
37. Zeber JE, Vijan S, Valenstein M: The cost-utility of depression screening: usual care versus collaborative treatment; in Abstracts of the Academy for Health Services Research and Health Policy Annual Meeting 19:14, 2002Google Scholar
38. Gilchrist VJ, Stange KC, Flocke SA, et al: A comparison of the National Ambulatory Medical Care Survey (NAMCS) measurement approach with direct observation of outpatient visits. Medical Care 42:276–280, 2004Google Scholar
39. Stange KC, Zyzanski SJ, Smith TF, et al: How valid are medical records and patient questionnaires for physician profiling and health services research? A comparison with direct observation of patient visits. Medical Care 36:851–867, 1998Google Scholar



