Financial Incentives and Accountability for Integrated Medical Care in Department of Veterans Affairs Mental Health Programs
Serious mental illnesses (schizophrenia, bipolar disorder, and recurrent major depressive disorder) can affect up to 10% of the general population and are associated with substantial functional impairment, health care costs, and premature mortality ( 1 , 2 ). Poor outcomes have been partly attributed to co-occurring general medical conditions such as cardiovascular disease ( 3 ), diabetes ( 4 , 5 ), and hepatitis C ( 6 ), which disproportionately affect patients with serious mental illness. Cardiovascular disease is the most common condition associated with premature death among patients with serious mental illness ( 3 ). However, patients with serious mental illness are less likely than other patients to receive adequate quality of care for cardiovascular disease-related conditions and other medical comorbidities ( 7 , 8 ).
There are substantial challenges in the monitoring and management of co-occurring conditions in general medicine and specialty mental health settings. As with other medical specialties, integrated care for general medical conditions is considered critical for enhancing quality of care and outcomes for individuals with serious mental illness ( 9 , 10 ). However, health services for co-occurring conditions are often fragmented across mental health and general medical care settings, even within large health systems such as the U.S. Department of Veterans Affairs (VA) health system ( 10 ). This is partly attributable to the observation that many patients with serious mental illness regard the mental health clinic as their "home site" for most of their health care needs and are less inclined to seek medical services in general medical settings ( 11 ). Despite the VA's national and regional integration and its use of a common electronic medical record, physical, cultural, and administrative separation of general medical and mental health services may lead to fragmentation of care and, ultimately, poor quality and outcomes related to general medical services for patients with serious mental illness (Fragmentation of general medical and mental health services may persist because of a lack of perceived shared responsibility ( 12 ).
Fragmentation of general medical and mental health services may persist because of a lack of perceived shared responsibility (accountability) across different providers ( 13 ). Nonetheless, some of the most common psychiatric treatments, notably second-generation antipsychotics, have general medical consequences, including increased obesity and elevated diabetes and cardiovascular disease risks ( 4 ). This realization has subsequently challenged the status quo for separating out general medical from mental health care services and has added force to calls for mental health programs to share accountability for monitoring and managing patients' medical risks and for improving quality of care overall ( 10 , 14 ).
Several system-level strategies to promote greater accountability for care across clinical silos have been proposed, including organizational changes, such as co-location of medical providers in mental health clinics, and financial incentives for improving care processes, including pay for performance ( 15 ). Pay for performance involves financial incentives to providers or health care systems when certain target quality-of-care measures are achieved within providers' patient panels.
However, to date there have been no comprehensive studies characterizing the degree to which mental health care programs are accountable for monitoring and managing general medical conditions or whether these programs use organizational or financial strategies to promote accountability. Organizational strategies such as co-location may take years to implement fully, especially in settings with limited access to qualified providers. Financial incentives in turn may more readily encourage programs to utilize existing resources and providers to improve care. Understanding mutable system-level strategies that may facilitate greater accountability for providing general medical services at the level of the mental health program leadership may inform efforts to improve integrated care for patients with serious mental illness. The VA provides an ideal opportunity to study system-level factors associated with accountability across the U.S. given its national scope, consistency in financing, and "top-down" management structure ( 16 ).
We determined the extent to which VA mental health program leaders perceive their outpatient mental health programs as being primarily accountable for the screening and monitoring of co-occurring general medical conditions among veterans with serious mental illness, and we examined the system-level factors associated with accountability. Our primary hypothesis was that the use of financial incentives (pay for performance) would be associated with increased perceptions of accountability for the screening and monitoring of general medical conditions.
Methods
Data were from the national VA Mental Health Program Survey, conducted from October 2007 to December 2007 for all VA mental health programs in VA facilities located within the 50 United States. The survey included measures of health system-level factors and integration of general medical and mental health care. Mental health program leaders from 108 of 133 VA mental health programs (81%) completed the survey.
Mental Health Program Survey
Mental Health Program Survey questions were based on a conceptual framework ( 10 ) developed by Shortell and colleagues ( 17 ) that describes how underlying system-level features (notably, resources) and organizational processes (accountability and performance incentives) are associated with clinical integration strategies, such as perceived accountability for co-occurring conditions, which in turn can influence patient outcomes. Using this framework, survey items were drawn from established VA organizational surveys, including the Primary Care Practices Survey ( 18 ) and the Drug and Alcohol Program Survey ( 19 ). The survey's content validity was evaluated and confirmed on the basis of input from VA experts with extensive knowledge regarding integrated mental health, substance use disorder, or general medical services for persons with serious mental illness.
Outpatient mental health program leaders were identified through a national list of mental health programs within VA medical centers, and their status and contact information was confirmed with queries to the chiefs of staff at each medical center. The leader of each mental health program was designated as the key informant for the program survey. As in previous organizational surveys ( 18 , 19 ), we chose to have one key informant complete the survey, because the program leader is chiefly responsible for the management and implementation of policy decisions regarding the organization and delivery of care for patients with serious mental illness at his or her facility. Using established methods for surveying VA program leaders ( 18 ), we sent the survey to the mental health program leader via express mail with a personalized cover letter describing the survey's purpose and a prepaid express mail return envelope. Once responses were received, the surveys were reviewed for completeness by study personnel and respondents were contacted if any section was incomplete or unclear. This study was reviewed and approved by the VA Institutional Review Board.
Outcome measures: primary accountability
The Mental Health Program Survey included questions on the program's accountability for screening and monitoring of common conditions among persons with serious mental illness, as well as on health system factors that can influence the degree to which general medical services are integrated within the mental health program. Accountability was defined as the extent to which providers in the mental health program were primarily responsible for services related to the following areas: psychotropic drug level monitoring—that is, initial order and follow-up; diabetes and cardiovascular disease risk screening tests (including fasting glucose and cholesterol) for patients given prescriptions for second-generation antipsychotic medications; obesity screening and weight management; hepatitis C screening; at-risk alcohol use screening; and tobacco use counseling. For each service, mental health program leaders were asked, "In general at your facility, who is primarily responsible for the following services for patients with mental disorders?" Response options were mental health providers, general medical providers, both mental health and general medical providers, or other type of provider.
Primary accountability was defined as the mental health providers' being primarily responsible for the task because these services represent care for common conditions experienced by patients with serious mental illness that are also closely related to their psychiatric treatment ( 7 , 9 ). Notably, second-generation antipsychotics have been associated with diabetes and cardiovascular disease risk factors, and hence screening tests such as fasting glucose and cholesterol are recommended ( 14 , 20 ). Moreover, dichotomizing primary accountability with other responses would represent a more conservative estimate of the degree of accountability that was actually perceived across sites, given potential for response bias (that is, persons reporting anything other than primary accountability are likely not to perceive any accountability).
Explanatory measures
Explanatory system-level factors thought to influence accountability included financial incentives and organizational characteristics, notably co-location of at least one full-time general medical provider in the mental health program, psychiatric nurse staffing, and academic affiliation. We chose to examine these mutable factors in order to inform policies and interventions to improve integrated care for VA patients with mental disorders. Financial incentives were defined as whether the mental health program leader received a financial bonus for achieving the minimum target for guideline-based performance measures set by the VA for key clinical services measured by the VA's External Peer Review program, including psychotropic drug level monitoring—initial order and follow-up; diabetes and cardiovascular disease risk screening tests for patients given prescriptions for second-generation antipsychotic medications; obesity screening and weight management; hepatitis C screening; at-risk alcohol use screening; tobacco use counseling; administering pneumococcal vaccination for patients older than 60 years; and colorectal cancer screening ( 21 ). For staffing, mental health program leaders were queried regarding the number of outpatient psychiatric nurses through a standard question on staff volume ( 17 ). Number of nurses was treated as a continuous variable and is a proxy for program size. Nurse volume (number of nurses) is a proxy for clinic size and has been found to be associated with improved chronic medical care management in prior studies ( 22 ). Academic affiliation was defined as whether the mental health program is currently training psychiatric residents (yes, or no) ( 17 ).
Analysis
All analyses were performed using SAS, version 9.1. For the accountability measure, responses were dichotomized as to whether the mental health provider was primarily accountable versus all other responses (that is, whether the primary care provider, both mental health and primary care provider, or other provider was primarily responsible). Multivariable logistic regression analyses were used to determine the association between financial incentives and other system factors and accountability for each outcome (for example, psychotropic drug level monitoring and diabetes and cardiovascular disease risk assessment). We accounted for clustering by Veterans Integrated Service Network (VISN) in our multivariable logistic regression analyses by using the sandwich estimate of variance ( 23 ).
Results
Out of 108 mental health programs, 29 (27%) had a co-located general medical clinician (≥1 full-time equivalent), and the mean±SD number of nurses was 14.5±25.7. The mean number of psychiatric residents and interns that were trained in the mental health program within the past year was 10.1±12.8.
As shown in Table 1 , 78% of mental health programs reported that they were primarily responsible for psychotropic drug level monitoring. In contrast, 36% said that they were primarily responsible for diabetes and cardiovascular risk screening. In addition, 12% reported accountability for obesity screening and weight management. For screening associated with high-risk behaviors, only 10% of mental health programs said they were primarily accountable for hepatitis C screening, whereas a higher number said they were accountable for alcohol screening (17%) and tobacco counseling (23%).
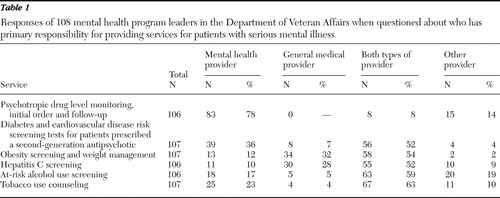 |
In addition, a substantial number of mental health program leaders reported shared accountability between mental health and other providers. Notably, 52% of leaders reported shared accountability for diabetes and cardiovascular risk screening, and 54% reported joint accountability for obesity screening and weight management. Shared accountability was also prevalent for risk factor screenings (screening for hepatitis C and alcohol misuse) and tobacco use counseling, but only 8% of programs reported shared accountability for psychotropic drug level monitoring ( Table 1 ).
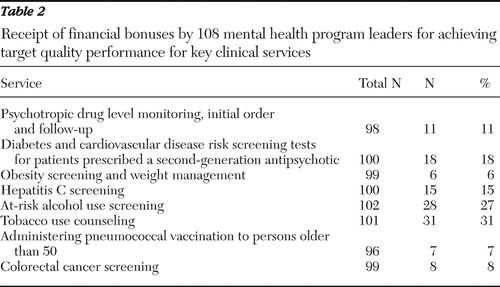
For financial incentives, only 18% of mental health program leaders stated that they received financial bonuses for diabetes and cardiovascular disease risk screening, 15% received bonuses for hepatitis C screening, and 6% received bonuses for obesity screening and weight management ( Table 2 ). Financial incentives were most commonly used for tobacco use counseling and alcohol screening and least commonly used for pneumococcal vaccination or colorectal cancer screening.
 |
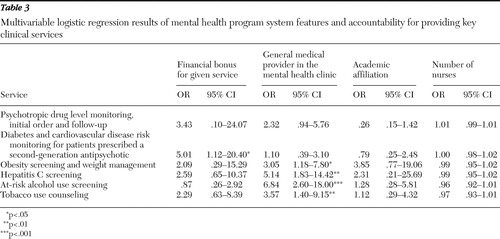
After the analysis controlled for system factors (co-location of medical providers, staffing, and academic affiliation), receiving financial bonuses for diabetes and cardiovascular disease risk screening was independently associated with mental health program leaders' perceived accountability for diabetes and cardiovascular disease monitoring (odds ratio [OR]=5.01, p<.05) ( Table 3 ). In addition, co-location of general medical providers was also associated with perceived accountability for screening and monitoring associated with high-risk conditions, namely hepatitis C screening (OR=5.14, p<.01), at-risk alcohol use screening (OR=6.84, p<.001), obesity screening and weight management (OR=3.05, p<.05), and tobacco counseling (OR=3.57, p<.01) ( Table 3 ). However, having a co-located general medical provider in the mental health programs was not associated with perceived accountability for diabetes and cardiovascular disease risk monitoring. Academic affiliation and number of nurses were not independently associated with accountability ( Table 3 ).
 |
Discussion
Until now, no national studies have characterized the degree of accountability of mental health providers for integrating medical care or the use of financial incentives across practices. In the national VA Mental Health Program Survey we found that financial incentives related to diabetes and cardiovascular risk assessment were associated with greater perceived accountability for this service within mental health programs, consistent with our hypothesis. However, financial incentives for other tasks were not associated with accountability. Organizational factors, notably co-location of a general medical provider, was associated with increased accountability for the screening for conditions associated with high risk behaviors, such as hepatitis C and alcohol misuse.
Only one-third of VA mental health program leaders reported primary accountability for monitoring of diabetes and cardiovascular disease risk factors associated with second-generation antipsychotics. In contrast, the majority reported primary accountability for psychotropic drug level monitoring. There was even less perception of primary accountability by mental health program leaders for screening for conditions that are associated with high-risk behaviors, such as hepatitis C or alcohol misuse, even though these conditions occur disproportionately among patients with serious mental illness and can have an adverse effect on outcomes ( 6 , 24 ). Still, a substantial proportion of program leaders reported a high level of endorsement of shared responsibility for clinical tasks, including cardiovascular risk factor monitoring when second-generation antipsychotics are prescribed. Given the highly integrated nature of VA health care, it is not surprising that these issues might be addressed by either clinical service. It is likely that mental health program leaders in the VA are ahead of other non-VA health systems in acknowledging accountability for management of general medical conditions. The recent systemwide implementation of collaborative care models for depression, posttraumatic stress disorder, and substance use management in primary care (that is, VA Primary Care-Mental Health Integration) may further promote the notion of shared responsibility between primary care and mental health providers ( 25 ). Nonetheless, further research on the true meaning of shared accountability (for example, to what extent it leads to truly coordinated care) is necessary to determine whether shared accountability leads to improved medical care quality and ultimately improved outcomes for veterans with serious mental illness.
Overall, less than 20% of mental health programs used financial incentives to encourage improved performance measures for diabetes and cardiovascular disease risk monitoring among patients prescribed second-generation antipsychotics, and even fewer VA mental health program leaders received financial bonuses for achieving performance targets for obesity screening and weight management, which can also be associated with these medications. We found that financial incentives for diabetes and cardiovascular risk factor monitoring were associated with a greater probability of perceived accountability for performing this service. However, financial incentives were not associated with accountability for the other clinical services, including psychotropic drug level monitoring, obesity screening, at-risk alcohol use screening, or tobacco use counseling. The current focus on the cardiovascular risk factors of second-generation antipsychotics might have contributed to a greater awareness by mental health providers of the importance of the medical side effects of these medications. In addition, guidelines were recently published regarding the regular monitoring of cardiovascular disease and diabetes risk for patients given prescriptions for second-generation antipsychotic medications ( 14 , 19 ), and the VA has recently taken the lead to improve the monitoring and management of diabetes and cardiovascular risk among patients taking second-generation antipsychotic medications ( 26 ).
Nonetheless, the long-term impact of financial incentives on quality improvement remains to be seen. The evidence regarding whether financial incentives such as pay for performance improve the quality of care in general medical settings has been mixed, with some studies achieving modest success in diabetes care, although overall there is a dearth of any conclusive empirical evidence regarding the effectiveness of pay for performance in improving quality ( 27 ). Prior research suggests that larger financial incentives, upwards of 10%–15% of the providers' salary, may be necessary for providers to pay attention to the incentive ( 28 ). There is also concern that financial incentives might lead to "cherry picking" by providers, which might lead to avoidance of patients with more complex health care needs ( 29 ), which could shortchange sicker patients with multiple comorbidities ( 30 ). Still, before establishing performance incentives, guidelines regarding who is accountable for what types of general medical services, such as diabetes and cardiovascular risk factor monitoring among patients prescribed second-generation antipsychotics, and how accountability should be shared across different providers may need to be established so that providers are more willing to adopt incentive programs.
In terms of organizational factors, co-location of general medical providers increased the likelihood that conditions associated with high-risk behaviors (hepatitis C and at-risk alcohol use) would be assessed. A previous randomized controlled trial of co-located general medical providers compared with usual care in mental health settings led to improved quality of preventive services among VA patients with serious mental illness ( 31 ). However, less than one-quarter of VA mental health programs had a co-located general medical clinician. Although this estimate may seem low, the proportion of VA mental health programs with co-located general medical providers may far exceed those outside the VA ( 32 ). The VA, with its integrated payer and provider system, also has greater potential to promote integrated care services through co-location of providers. Academic affiliation (availability of residents) and staffing (number of nurses in the mental health program) were not independently associated with accountability. Perhaps these underlying organizational factors represent well-established features of the overall facility, and in contrast, other factors such as co-location and use of financial incentives might be more closely related to accountability.
This study represents an important and timely assessment of organizational and financial factors associated with accountability for general medical services among mental health programs within one of the largest U.S. providers of health care services for persons with serious mental illness. However, there are limitations to this study that warrant consideration. First, we recognize that a key limitation of measuring health system features based on any survey is the potential for misclassification bias arising from key informant responses, which may or may not represent actions made by all patient-provider dyads in their particular site. Particularly, we were unable to distinguish whether perceived accountability was attributable to the "top down" setting of financial bonuses in the VA rather than providers' actual perceptions of accountability ( 32 ).
Second, we were unable to distinguish whether financial incentives preceded accountability or vice-versa (temporal ambiguity), because mental health program directors may have perceived a clinical task as within their realm of accountability before incentive programs were implemented. Although survey respondents were asked whether they received a bonus, the question did not delineate between individual versus group (that is, mental health program-wide) bonuses. For VA performance measures, incentives are typically given to VISN directors, with varying agreements regarding distribution at the facility level. In a recent survey of VA chiefs of staff, about half (49%) reported that bonuses in their facilities went to individual providers, 24% reported that they went to groups of providers (for example, mental health programs), and 28% reported that bonuses were split between groups and individual providers ( 33 ).
We were also unable to determine whether the primary care leader at the same VA facility received a financial bonus for these procedures, which could have been attributed to lower rates of accountability for these procedures by mental health program leaders. To date there are no published data on the use of VA financial incentives among individual primary care providers. Future research is needed to determine to what extent financial incentives are given at the individual versus group level and how that influences quality of care in mental health settings. Moreover, for our key outcomes that represent side effects of second-generation antipsychotic medications (diabetes and cardiovascular risk factor monitoring and obesity screening and weight management), it is unlikely that primary care would have financial incentives for diabetes and cardiovascular risk monitoring when the mental health service prescribes the antipsychotic, because it would be unreasonable for primary care to be held responsible for ordering a test within a time frame initiated by a prescription if it is not a prescription made within primary care.
In addition, patient-level factors that might influence differences in accountability across sites, such as psychiatric or medical burden, were not available. Only co-location was assessed, and information on other integrated care models such as the chronic care model was unavailable, although a more definitive study of integrated care models is under way. Finally, we were unable to determine whether financial incentives or accountability were actually linked to improved patient outcomes, because available data on patient-level quality of care from the same year were not available for these particular clinical services.
Conclusions
Our results suggest that financial incentives may potentially promote accountability in VA mental health programs for cardiovascular risk factor monitoring among patients given prescriptions for second-generation antipsychotic medications. Co-location of general medical providers may also promote perceived accountability for conditions associated with high-risk behaviors. Future research is necessary to determine whether these financial incentives improve medical care quality and outcomes for patients with serious mental illness. Co-location of providers as well as complementary strategies such as the chronic care model may also promote accountability for managing co-occurring conditions and health behaviors ( 34 ).
Acknowledgments and disclosures
This research was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (grants IIR05-195 and IIR 07-115). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. The authors thank the following individuals for providing a critical review of the Mental Health Program Survey: Mark Bauer, M.D., Stephen Cavicchia, Psy.D., Joseph Conigliaro, M.D., M.P.H., Larry Drill, M.S.W., M.P.H., Joanne Kirchner, M.D., David Oslin, M.D., Linda McBride, R.N., Kathleen Schutte, Ph.D., and Marcia Valenstein, M.D.
The authors report no competing interests.
1. Murray CJ, Lopez AD: Evidence-based health policy—lessons from the Global Burden of Disease Study. Science 274:740–743, 1996Google Scholar
2. Achieving the Promise: Transforming Mental Health Care in America. Pub no SMA-03-3832. Rockville, Md, Department of Health and Human Services, President's New Freedom Commission on Mental Health, 2003Google Scholar
3. Hennekens C: Increasing global burden of cardiovascular disease in general populations and patients with schizophrenia. Journal of Clinical 68:4–7, 2007Google Scholar
4. Newcomer JW: Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs 19:1–93, 2005Google Scholar
5. Kilbourne AM, Cornelius JR, Han X, et al: General medical conditions in older patients with serious mental illness. American Journal of Geriatric Psychiatry 13:250–254, 2005Google Scholar
6. Rosenberg SD, Goodman LA, Osher FC, et al: Prevalence of HIV, hepatitis B, and hepatitis C in people with severe mental illness. American Journal of Public Health 91:31–37, 2001Google Scholar
7. Kilbourne AM, Welsh D, McCarthy JF, et al: Quality of care for cardiovascular disease-related conditions in patients with and without mental disorders. Journal of General Internal Medicine 23:1628–1633, 2008Google Scholar
8. Druss BG, Bradford DW, Rosenheck RA, et al: Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA 283:506–511, 2000Google Scholar
9. Institute of Medicine: Improving Quality of Health Care for Mental and Substance Use Conditions. Washington DC, National Academy Press, 2005Google Scholar
10. Horvitz-Lennon M, Kilbourne AM, Pincus HA: From silos to bridges: meeting the general health care needs of adults with severe mental illnesses. Health Affairs 25:659–669, 2006Google Scholar
11. Druss BG, Rosenheck RA: Locus of mental health treatment in an integrated service system. Psychiatric Services 51:890–892, 2000Google Scholar
12. Evaluation of Services for Seriously Mentally Ill Patients in the Veterans Health Administration of the Department of Veterans Affairs, Revised Statement of Work. Washington, DC, Department of Veterans Affairs, Office of Policy, Planning, and Preparedness, Mar 2006Google Scholar
13. Koran LM, Sox HC Jr, Marton KI, et al: Medical evaluation of psychiatric patients: I. results in a state mental health system. Archives of General Psychiatry 46:733–740, 1989Google Scholar
14. Marder SR, Essock SM, Miller AL, et al: Physical health monitoring of patients with schizophrenia. American Journal of Psychiatry 161:1334–1349, 2004Google Scholar
15. Bodenheimer T, May JH, Berenson RA, et al: Can money buy quality? Physician response to pay for performance. Issue Brief no 102. Washington, DC, Center for Studying Health System Change, 2005Google Scholar
16. Meterko M, Mohr DC, Young GJ: Teamwork culture and patient satisfaction in hospitals. Medical Care 42:492–498, 2004Google Scholar
17. Shortell S: Remaking Health Care in America: The Evolution of Organized Delivery Systems, 2nd ed. San Francisco, Jossey-Bass, 2000Google Scholar
18. Yano EM, Simon B, Canelo I, et al: VHA Survey of Primary Care Practices. Technical Monograph 00-MC12. Washington, DC, Veterans Administration, Aug 2000Google Scholar
19. Tracy SW, Trafton JA, Weingardt KR, et al: How are Substance Use Disorders Addressed in VA Primary Care and Psychiatric Settings? Results of the DAPS National Survey. Palo Alto, Calif, VA Palo Alto Program Evaluation Resource Center, 2006Google Scholar
20. American Diabetes Association: Consensus development conference on antipsychotic drugs and obesity and diabetes. Clinical Psychiatry 65:267–272, 2004Google Scholar
21. FY 2005 Executive Career Field. Network Director Performance Measurement System and JCAHO Hospital Core Measures Technical Manual. Washington, DC, VHA Office of Quality and Performance, 2005. Available at http://vaww.oqp.med.va.gov/oqp_services/performance_measurement/tech_man.asp Google Scholar
22. Druss BG, Marcus SC, Olfson M, et al: Trends in care by nonphysician clinicians in the United States. New England Journal of Medicine 348:130–137, 2003Google Scholar
23. Carroll RJ, Wang S, Simpson DG, et al: The Sandwich (Robust Covariance Matrix) Estimator. College Station, Texas A&M University, Department of Statistics, 1998. Available at www.stat.tamu.edu/ftp/pub/rjcarroll/sandwich.pdf Google Scholar
24. Conway KP, Compton W, Stinson FS, et al: Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry 67:247–257, 2006Google Scholar
25. Post EP, Van Stone WW: Veterans Health Administration Primary Care-Mental Health Integration initiative. North Carolina Medical Journal 69:49–52, 2008Google Scholar
26. Healthcare Inspection: Atypical Antipsychotic Medications and Diabetes Screening and Management. Washington, DC, Department of Veterans Affairs, Office of Inspector General, 2007Google Scholar
27. Young GJ, Meterko M, Beckman H, et al: Effects of paying physicians based on their relative performance for quality. Journal of General Internal Medicine 22:872–876, 2007Google Scholar
28. Hillman AL, Ripley K, Goldfarb N, et al: The use of physician financial incentives and feedback to improve pediatric preventive care in Medicaid managed care. Pediatrics 104:931–935, 1999Google Scholar
29. Casalino LP, Alexander GC, Jin L, et al: General internists' views on pay-for-performance and public reporting of quality scores: a national survey. Health Affairs 26:492–499, 2007Google Scholar
30. Boyd CM, Darer J, Boult C, et al: Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA 294:716–724, 2005Google Scholar
31. Druss BG, Rohrbaugh RM, Levinson CM, et al: Integrated medical care for patients with serious psychiatric illness: a randomized trial. Archives of General Psychiatry 58:861–868, 2001Google Scholar
32. Alfano E: Get It Together: How to Integrate Physical and Mental Health Care for People With Serious Mental Disorders: Executive Summary. Washington, DC, Bazelon Center for Mental Health Law, 2004Google Scholar
33. Yano E, Fleming B, Canelo I, et al: National Survey Results for the Chief of Staff Module of the VHA Clinical Practice Organizational Survey: Technical Monograph 07-CPOS01. Sepulveda, Calif, Department of Veterans Affairs, Health Services Research and Development Service, Center for the Study of Healthcare Provider Behavior, 2007Google Scholar
34. Kilbourne AM, Bauer MS, Nossek A, et al: Improving medical and psychiatric outcomes for individuals with bipolar disorder: a randomized, controlled effectiveness trial. Psychiatric Services 59:760–768, 2008Google Scholar



