Predicting Falls Among Psychiatric Inpatients: A Case-Control Study at a State Psychiatric Facility
In 1996 the Joint Commission on Accreditation of Health Care Organizations began monitoring sentinel events of patient falls. An analysis of fatal falls indicated that, of 22 fatal falls, four (18%) involved psychiatric patients in various psychiatric facilities and the rest occurred in general hospitals and long-term-care facilities ( 1 ). However, 17 (77%) of the 22 patients had an impaired mental status resulting from chronic mental illness or acute intoxication. Risk factors most frequently associated with fatal falls included use of sedative medications, urinary urgency, history of prior falls, and age over 70.
Prevention of falls in geriatric populations living at home and in long-term-care facilities has been studied extensively. Falls in general medical hospitals have also become a focus of scientific research. As per Myers' critical review ( 2 ) of the fall risk-assessment literature, only five out of the 32 hospital fall assessment tools that were reviewed were developed with the gold-standard case-control or cohort research methodology and also included details about the tool's specificity and sensitivity. These five tools most frequently included the following risk factors: mental state impairment, gait and mobility, elimination problems, medications, and fall history. Only one of the five tools had undergone further testing by other authors across different settings. The sensitivity of the tools ranged from 70% to 95%, and the specificity, when tested by other researchers in different populations, ranged between 29% and 54%. Low specificity (high percentage of false positives) was of concern because of a possible desensitizing effect it might have on the clinical staff. A later systematic review and meta-analysis found that the accuracy of fall risk-assessment tools varied depending on the type of patient population tested, and it identified two tools that would provide moderate accuracy across settings ( 3 ). Conversely, that study found that nurses' clinical judgment provided the same level of predictive accuracy but was more consistent across settings.
Two systematic reviews and meta-analyses ( 4 , 5 ) and the Joanna Briggs Institute ( 6 ) identified a lack of strong evidence to support that fall prevention programs in acute care hospitals reduce the number of falls or fallers and concluded that more research was needed on fall prevention in acute settings. Other reviews, by Gillespie and colleagues ( 7 ) and Oliver and colleagues ( 8 ), found that multifactorial intervention programs in which the interventions were selected on the basis of clinical judgment modestly reduced fall rates in hospital settings.
Falls in psychiatric populations have been studied less rigorously ( 9 , 10 ), and there is a lack of well-researched and validated fall risk models specifically developed for populations of psychiatric inpatients. Krauss and colleagues ( 11 ) included psychiatric inpatients (ten patients in the study group; 32 persons in a control group) in a case-control study of potential risk factors for falling at a large urban academic hospital. Gait and balance problems, lower-extremity problems, confusion, use of sedatives and hypnotics, use of diabetes medications, and the need to be assisted with the activities of daily living were significantly associated with falling. Removing psychiatric patients from the mix changed the results of the multivariate analysis in that a gait and balance deficit and problems with lower extremities became borderline significant.
Tay Sim-Yeng and colleagues ( 12 ) reported that falls accounted for 36% of incidents in a state psychiatric hospital in Singapore, occurring at a rate of .41 per 1,000 patient days, with an injury rate of 14%. A descriptive study of 17 fallers among 197 acutely ill psychiatric inpatients in Taiwan found that fallers were more likely than nonfallers to have had a previous fall and to have generalized weakness, confusion or disorientation, difficulty moving, elimination problems, and temperature elevation ( 13 ). A retrospective study of variables associated with falls at the Colorado Psychiatric Hospital ( 10 ) found that a history of falls, female gender, anxiety and agitation, sedating medications, and bowel urgency were associated with falls. Irvin ( 9 ) reported in a study of characteristics of fallers on a 40-bed psychiatric unit at a general hospital that gait and balance impairment and a history of falls were the only statistically associated variables.
The purpose of this study was to add to the existing research on fall risk among psychiatric inpatients in an acute setting. This understudied group of patients might be qualitatively different from other populations served in acute settings. On the basis of our review of the relevant literature and prior fall data at our facility, we hypothesized that a number of factors would be predictive of falling: age 60 and above, medical comorbidities (history and acute), dizziness, weakness, sedation, and orthostatic blood pressure or pulse changes. We also hypothesized that compared with nonfallers, fallers would have taken a greater number of medications within a 24-hour period and that prescribed benzodiazepines would be significantly associated with falls. Our goal is to use these data and the existing evidence-based recommendations to develop a fall risk-assessment tool to facilitate clinical judgment among nursing staff. Subsequently, the tool would be studied for accuracy, as would the effectivness of fall prevention interventions.
Methods
We analyzed retrospective medical records of all patients who fell at the New York State Psychiatric Institute (NYSPI) between 2000 and 2005 and the same number of nonfallers admitted during the same period who matched the fallers on primary psychiatric diagnosis. Each fall and all fallers were identified by the institute's incident-reporting system. Within the system a fall was defined as a reported or witnessed accidental loss of balance that resulted in falling to any level lower than the patient. This study received approval by the NYSPI Institutional Review Board as a minimal-risk project using deidentified and aggregated patient information.
Sample
NYSPI is a 58-bed state inpatient psychiatric facility. The average length of stay between 2000 and 2005 was 35 days, ranging from 14 to 60 days. The annual fall rate ranged from .8 to 1.3 falls per 1,000 patient days. The most serious injury was a subdural hematoma, but most falls were benign. A fall prevention program was implemented in 2002 and consisted of identifying patients at risk at the time of admission by assessing for the following five risk factors: history of falls, alteration in mobility, alteration in consciousness, age 65 and older, and elimination urgency or incontinence. Interventions were multifactorial and were used selectively for each patient at risk.
The sample consisted of 74 fallers and 74 nonfallers (N=148 patients). Each faller represented one case, and information collected was for the first fall only.
Data collection
A group of registered nurses collected data that would be routinely available in the medical record: age, gender, race-ethnicity, medications administered, vital signs, medical history items documented at the time of admission, physical complaints on the day of the fall, and acute medical conditions documented in the progress notes. Medical history items included history of falls in the past 90 days, seizures, syncope, diabetes, history of impaired mobility, dizziness, pain, stroke, weakness, incontinence and elimination urgency, dehydration, confusion, and arthritis and musculoskeletal problems. These items were found in the nursing and physician admission assessments and physical exam forms; the assessment forms include prompts to ask the patient questions about medical problems and to assess patients' physical systems (cardiovascular, for example). The physical complaints on the day of the fall included symptoms documented in the progress notes 24 hours before and up to the time immediately after the fall. The acute medical conditions included any medical diagnoses documented in the physician's progress notes 24 hours before the fall. The same variables were collected for nonfallers on a randomly chosen day of their hospitalization.
Sitting-to-standing sets of daily vital signs (vital signs taken first in a sitting position and then after approximately two minutes of standing) were analyzed as raw numbers. Data were entered into a Microsoft Access database and visually checked for accuracy by several research staff assistants.
Data analysis
Data were converted into SPSS system files for analysis with SPSS, version 15. The distribution properties of all variables were examined for normality and distribution characteristics, and preliminary analyses examined the demographic measures across faller status and gender. Preliminary analyses indicated a number of gender differences; therefore, gender was included as a factor along with faller status in subsequent analyses, using two (faller status) by two (gender) analyses of variance (ANOVAs). Specifically, two-way ANOVAs were performed on current age, number of prescription drugs, summed physical complaints on the day of the fall, summed medical history items (taken at admission), and routine sitting and standing vital signs, with faller status and gender as main factors of the analyses. Dichotomous variables were created to account for the presence of an acute medical condition and the taking of blood pressure medications, selective serotonin reuptake inhibitors (SSRIs), mood stabilizers, antipsychotics, and benzodiazepines (lorazepam, clonazepam, and zolpidem). Cross-tabulations were performed for each of these dichotomous measures separately by faller status and gender, and the Fisher's exact test was applied to test distributions. Cross-tabulations greater than 2×2 cells were tested with the chi square statistic.
To have an integrative analysis, we performed multivariate logistic regression analyses. Twenty-three cases were missing data on vital signs; we therefore performed two separate multivariate logistic regressions, one with and one without the vital signs data included. Faller status served as the dependent outcome for both, and the various measures above were assessed as possible independent predictors. In performing the logistic regressions, gender and age were entered at the first step; this was followed by a backward-stepping procedure that entered the following measures into the logistic regression: the number of discrete drugs prescribed; the summed medical history items; the summed physical complaints on the day of the fall; the presence of an acute medical condition; and the taking of blood pressure medications, SSRIs, mood stabilizers, lorazepam, clonazepam, zolpidem, and antipsychotics. (In the backward-stepping procedure, all measures are entered into the logistic regression on a measure-by-measure basis, and those that do not meet a specified criterion [p to enter=.10; p to remove=.15] of significance are removed from the equation.)
Results
Sample characteristics
Of the 148 patients in the sample, 47 (32%) were male and 101 (68%) were female, mean±SD age was 38.3±16.8 years (median age was 38; range 13–82). Race-ethnicity was recorded for 125 patients out of 148, and 17 (14%) were black, 47 (38%) were Hispanic, 58 (46%) were white, one (1%) was Asian, and two (2%) were from other racial-ethnic groups. Primary clinical diagnoses included 50 patients (34%) with bipolar disorders, 36 (24%) with schizophrenia or psychotic disorders, 26 (18%) with major depressive disorder, 26 (18%) with opiate dependence, and ten (7%) with eating disorders. We examined the prevalence of falling among all patients with these clinical diagnoses during the five-year period of assessment: bipolar disorder, 25 of 365 (7%); schizophrenia, 18 of 896 (2%); major depressive disorder, 13 of 503 (3%); opiate dependence, 13 of 330 (4%); and eating disorder, five of 210 (2%). The chi square statistic was highly significant ( χ2 =21.26, df=4, p<.001), with the bipolar disorder group having by far the highest prevalence rate for falling.
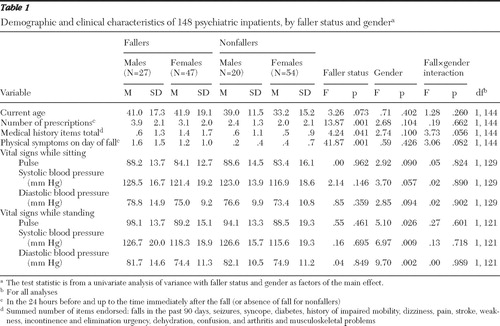
The demographic and clinical characteristics of the sample are presented by faller status and gender in Table 1 . There was a marginally significant effect of current age on faller status, indicating that the fallers as a group were somewhat older than the nonfallers. A categorical examination of age (age categories <20, 20s, 30s, 40s, 50s, and age 60 and older) showed that the youngest age group had the fewest fallers (eight of 27, 30%); for the 20s through the 50s age groups the percentages of fallers ranged from 42% to 59%. For the age group of 60 and older, 16 of 18 (89%) of the patients were fallers (overall χ2 =17.32, df=6, p=.008). Compared with nonfallers, fallers reported significantly more physical symptoms on the day of their fall (F=41.87, df=1 and 144, p=.001), endorsed significantly more medical history items (F=4.24, df=1 and 144, p=.041), and were being prescribed significantly more medications (F=13.87, df=1 and 144, p=.001).
 |
In addition to examining the total number of physical complaints on the day of the fall, we examined the frequencies of the individual physical complaints. The following differed significantly (Fisher's exact test) across faller status: urinary frequency and incontinence (no nonfallers; nine fallers, 12%; p=.005), generalized weakness (one nonfaller, 1%; ten fallers, 14%; p=.009), mental status impairment (two nonfallers, 3%; 11 fallers, 15%; p=.017), and dizziness (one nonfaller, 1%; nine fallers, 12%; p=.017). Sedation (six nonfallers, 8%; 14 fallers, 19%; p=.091) and unsteady gait frequencies (two nonfallers, 3%; eight fallers, 11%; p=.097) differed between fallers and nonfallers, but the differences were not significant. In addition to the summed medical history items obtained at the time of admission, we examined the frequencies of the individual medical history items for those that significantly differed by faller status: history of falls in the past 90 days (no nonfallers; seven fallers, 9%; p=.013), history of syncope (no nonfallers; six fallers, 8%; p=.028), and history of impaired mobility (four nonfallers, 5%; 13 fallers, 18%; p=.037).
Significant gender effects were present for all of the standing vital signs ( Table 1 ): standing pulse rate (F=5.10, df=1 and 121, p=.026), systolic blood pressure (F=6.97, df=1 and 121, p=.009), and diastolic blood pressure (F=9.70, df=1 and 121, p=.002). Marginal gender effects were present for all of the vital signs taken while patients were sitting.
The distribution of fallers by gender did not differ statistically; 27 of 47 males (57%) and 47 of 101 females (47%) were fallers ( Table 2 ). For the summed medical history items endorsed, there was a marginal interaction of faller status and gender, such that the female fallers endorsed more items than did the other three groups (male fallers and the two nonfaller gender groups), which were all approximately equivalent. Forty-three of 148 patients (29%) in the sample had a currently documented acute medical condition, and 32 of these 43 patients (74%) were fallers (for acute medical condition, 32 fallers, 43%; 11 nonfallers, 15%; p=.001). Although the main focus was on differences between fallers and nonfallers, gender differences were present for acute medical condition. Twenty-two males (47%) in the sample compared with 21 females (21%) had an acute medical condition (p=.002).
 |
Treatment with medication
One hundred twenty patients (81%) were taking medications belonging to the following classes: 80 (54%) taking first- and second-generation antipsychotics, 81 (55%) taking benzodiazepines, 44 (30%) taking anticonvulsant mood stabilizers, 12 (8%) taking lithium, 36 (24%) taking SSRI antidepressants, 13 (9%) taking other antidepressants, and 16 (11%) taking antihypertensive and cardiac drugs. Patients in opiate dependence research studies were administered medications as follows: seven (5%) were given buprenorphine, seven (5%) naltrexone, and 18 (12%) clonidine.
As mentioned above, the fallers were prescribed significantly more medications than their nonfaller counterparts, and this finding was consistent for males and females. We also analyzed the sample by categorizing the fallers and the nonfallers by number of medications administered in a 24-hour period before the fall occurred. The numbers of current medications were categorized into three categories (none, 28 patients; one to three, 71 patients; and four or more, 49 patients); six (21%), 33 (47%), and 35 (71%) patients, respectively, were fallers ( χ2 =18.50, df=2, p=.001). Specifically, fallers were more likely than nonfallers to be prescribed antihypertensive medication (19% versus 3%, respectively; p=.003) and the benzodiazepine clonazepam (42% versus 18%, respectively; p=.001). Fallers and nonfallers were prescribed SSRIs, mood stabilizers, antipsychotics, and two other benzodiazepines (lorazepam and zolpidem) at similar rates. By gender, females were prescribed more SSRIs (30 females versus six males, 30% versus 13%, respectively; p=.038). Eleven percent of the patients in the sample, including three males and 13 females, were on an antihypertensive drug. In this group, 14 (88%) patients were fallers: all three males and 11 of the 13 females ( χ2 =11.131, df=1, p=.001). Thirty-six (24%) patients in the sample were taking an SSRI; 21 (58%) of these were fallers. The difference in the proportions of patients on SSRI medication among the fallers and the nonfallers was not statistically significant. However, among the male fallers, six (22%) were taking an SSRI, whereas none of the nonfallers were taking an SSRI ( χ2 =6.52, df=1, p=.011).
Number of days on medication on day of the fall
Patients had been started on medication or restarted on previous medication for a mean±SD of 12.3±14.5 days before their fall. Data about how long the patients had ceased taking their regular medication before they resumed it were not collected. Patients had a fall an average of 11.5±11.1 days after an increase in medication dose.
Logistic regression
To identify the most salient associations with faller status, we performed a logistic regression analysis ( Table 3 ). Originally, we performed two logistic regressions, one with and one without vital signs data. We present the results of the logistic regression performed without the vital signs, because the results were substantially similar for both analyses. The most salient predictors of faller status were the summed physical complaints on the day of the fall (Wald statistic=19.07, p=.001) and receipt of clonazepam (Wald statistic=8.84, p=.003). The summed medical history items (Wald statistic=3.51, p=.061) and receipt of antihypertensive medication (Wald statistic=3.17, p=.075) were associated with faller status, but the associations did not reach significance. A somewhat surprising finding, given the literature, was that neither age nor gender was significantly associated with faller status.
 |
Discussion
Although univariate analyses revealed many variables to be associated with faller status, including current physical complaints, clonazepam treatment, antihypertensive treatment, age category, and number of medications, only physical complaints and clonazepam treatment survived the logistic regression analysis as significant independent predictors of faller status in our sample of psychiatric inpatients. In addition, logistic regression showed that the sum of medical history items was associated with faller status, although the association was not significant. Specifically, of the individual medical history items endorsed, a history of falls in the past 90 days, a history of syncope, and a history of impaired mobility each appeared with significantly higher frequencies among the fallers compared with the nonfallers.
Although we did not expect gender to predict falls, on admission to the hospital, females presented with more medical history items—a factor that in our study was significantly associated with faller status. A cross-sectional study of 4,050 women aged 60–79 showed that prevalence of falling increased with increasing numbers of simultaneously occurring chronic illnesses of the circulatory system, chronic obstructive pulmonary disease, depression, and arthritis ( 14 ). In a comparison of females and males, there was a positive correlation between the increasing number of medications administered and falling. However, the gender difference disappeared when patients took four or more medications in a 24-hour period.
As anticipated, the summed physical complaints on the day of the fall proved to be significantly associated with falling. Of the individual complaints, urinary frequency, generalized weakness, mental status impairment, and dizziness had significantly higher frequencies among the fallers versus the nonfallers in our sample. Frequencies of sedation and unsteady gait differed marginally between the fallers and the nonfallers.
According to Oliver and colleagues' ( 15 ) systematic review of risk-assessment tools, lower-limb weakness, gait instability, impaired judgment, elimination problems, and prescribing "culprit drugs"—such as sedatives and hypnotics—were some of the more consistently emerging fall predictors across all settings. Including these factors in screens for potential fallers predicted falls with sensitivity and specificity levels of 70%. Clonazepam and antihypertensive medications were "culprit drugs" that were significantly associated with falls in our sample, although the latter only marginally so. Of the five studies mentioned by Myers ( 2 ), other factors, such as generalized weakness, were examined in two studies and dizziness and vertigo were examined in one, but none of these symptoms were included in the final assessment tools.
The findings of this study should be interpreted with consideration of the following limitations. This was a retrospective examination of a limited sample of inpatient data; it was a case-control analysis of an understudied population, with the goal of identifying characteristics of psychiatric patients at greater risk of falls. The study was limited by its small sample and retrospective assessment, and it is unclear how generalizable or reproducible these findings will be. Larger samples in prospective studies in acute psychiatric settings are needed to determine whether psychiatric patients are qualitatively different from medical-surgical inpatients. Psychiatric patients may take sedating medications on a daily basis and remain fully ambulatory, whereas medical-surgical patients take fewer sedating drugs and are restricted to their beds. These and possibly other differences, such as fewer acute medical problems on a general adult psychiatric unit, may separate psychiatric inpatients, as a group, from medical-surgical inpatients in reference to fall risks.
Conclusions
The study showed that, at least at the psychiatric hospital we studied, a fall prevention program should focus on the patients who have risk factors identified by the systematic reviews: use of certain "culprit" medications, mental status impairment, and elimination problems. Various types of mobility problems, such as poor balance—not just unsteady gait—should be studied further. Among psychiatric inpatients, generalized weakness, dizziness, and sedation should be studied as independent risk factors for falls, because these symptoms might be the ones qualitatively separating psychiatric inpatients from other inpatient populations. Finally, studies of specific program interventions are needed, with the ultimate goal of enabling institutions to develop effective evidence-based fall prevention programs tailored to specific needs.
Acknowledgments and disclosures
The authors acknowledge the support of John Zatonsky, R.N., and Mark Robin, R.N.
The authors report no competing interests.
1. Fatal Falls: Lessons for the Future. Sentinel Event Alert. Oakbrook Terrace, Ill, Joint Commission on the Accreditation of Healthcare Organizations, 2000Google Scholar
2. Myers H: Hospital fall risk assessment tools: a critique of the literature. International Journal of Nursing Practice 9:223–235, 2003Google Scholar
3. Haines TP, Hill K, Walsh W, et al: Design-related bias in hospital fall risk screening tool predictive accuracy evaluations: systematic review and meta-analysis. Journal of Gerontology: Medical Sciences 6:664–672, 2007Google Scholar
4. Gates S, Fisher JD, Cooke MW, et al: Multifactorial assessment and targeted intervention for preventing falls injuries among older people in community and emergency care settings: systematic review and meta-analysis. British Medical Journal 336:130–133, 2008Google Scholar
5. Coussement J, De Paepe L, Schwendimann R, et al: Interventions for preventing falls in acute- and chronic-care hospitals: a systematic review and meta-analysis. Journal of the American Geriatrics Society 56:29–36, 2008Google Scholar
6. Falls in hospital: best practice; in Evidence Based Practice Information Sheets for Health Professionals. Adelaide, Australia, Joanna Briggs Institute for Evidence Based Nursing and Midwifery, 1998Google Scholar
7. Gillespie LD, Gillespie WJ, Robertson MC, et al: Interventions for prevention of falls in elderly people. Cochrane Database Review 4:CD00340, 2003Google Scholar
8. Oliver D, Connelly JB, Victor CR, et al: Strategies to prevent falls and fractures in hospitals and care homes, effect of cognitive impairment: systematic review and meta-analysis. British Medical Journal 334:83, 2007Google Scholar
9. Irvin D: Fall events. Journal of Psychosocial Nursing 12:9–15, 1999Google Scholar
10. Vaughn K, Young BC, Rice F, et al: A retrospective study of patient falls in a psychiatric hospital. Journal of Psychosocial Nursing and Mental Health Services 31:37–42, 1993Google Scholar
11. Krauss MG, Evanoff B, Hitcho E, et al: A case-control study of patient, medication, and care-related factors for inpatient falls. Journal of General Internal Medicine 20:116–122, 2005Google Scholar
12. Tay Sim-Yeng C, Queck C, Pariayasami S, et al: Fall incidence in a state psychiatric hospital in Singapore. Journal of Psychosocial Nursing and Mental Health Services 38:10–16, 2000Google Scholar
13. Tsai YF, Witte N, Radunzel M, et al: Falls in a psychiatric unit. Applied Nursing Research 11:115–121, 1998Google Scholar
14. Lawlor DA, Patel R, Ebrahim S: Association between falls in elderly women and chronic diseases and drug use: cross sectional study. British Medical Journal 327:712–717, 2003Google Scholar
15. Oliver D, Daly F, Martin F, et al: Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age and Aging 33:122–130, 2004Google Scholar



