Risk of Incarceration Between Cohorts of Veterans With and Without Mental Illness Discharged From Inpatient Units
Concern that persons with mental illness are unjustly overrepresented in the criminal justice system has received considerable attention ( 1 , 2 ). Structured interview studies have suggested that the proportion of inmates with severe mental illness in jails and prisons in the United States ranges between 6% and 16% ( 3 , 4 , 5 , 6 ), whereas the rate of severe mental illness in the general population has been estimated at 2.8% (annual prevalence) ( 7 , 8 ), which exceeds rates from community studies by more than three times. A recent study by the Department of Justice suggested that the prevalence of mental health problems, including both psychiatric and substance use disorders in jails and prisons, may be as high as 64% and 56%, respectively ( 6 ). These estimates exceed by a substantial margin the 29.5% lifetime rate for all psychiatric and substance use disorders found in the general population ( 8 ). Differences in methodology make comparisons across studies difficult; however, the Department of Justice findings suggest that there may be an elevated risk of incarceration for people with psychiatric or substance use disorders. Such findings have been of concern to mental health advocates and researchers alike. Also, the ability of correctional facilities to treat large numbers of inmates with psychiatric and substance abuse disorders has been questioned.
A consistent finding of many studies of offenders is the high occurrence of alcohol dependence and drug abuse, particularly among those with mental disorders unrelated to problems with substance use ( 9 , 10 , 11 , 12 ). The combination of severe mental illness and a substance use disorder is believed to be associated with increased risk of arrest, violence, other antisocial behavior, and failure with outpatient treatment ( 13 , 14 , 15 , 16 ). These negative outcomes among persons with co-occurring disorders are substantially elevated compared with clients in mental health treatment who have no history of substance abuse ( 5 , 16 ). Moreover, even with mental health and substance abuse treatment, patients with co-occurring disorders have higher rates of incarceration than those who receive mental health services exclusively ( 17 , 18 ), and these rates are not fully explained by the fact that illicit drug use is in itself illegal. Consequently, an emerging body of evidence suggests that persons with mental illnesses and substance abuse and dependence disorders represent a distinctive subgroup at heightened risk of involvement with the criminal justice system.
The link between mental illness, substance abuse and dependence, and involvement with the criminal justice system has spurred the development of a host of outpatient treatment programs that seek to reduce recidivism within the population of persons with co-occurring disorders who have been incarcerated ( 19 ). Many of these programs operate on the assumption that identification and treatment of psychiatric and substance abuse risk factors among offenders with such problems can reduce their risk of recidivism in the criminal justice system. Despite these assumptions, there has been only a handful of studies that compared treatment effects between traditional programs and modified offender-based treatments ( 20 ).
Jail diversion programs and mental health courts have been identified as potentially effective interventions for providing mental health services to persons with severe mental illness who are involved in the criminal justice system ( 21 , 22 ). These models are based on the assumption that a leveraged system of care is needed to reduce the risk of future criminal behavior. The high prevalence of substance abuse and dependence among mentally ill offenders, however, is a major confounding factor within this population. One recent study suggested that co-occurring substance abuse or dependence is more strongly predictive of arrest and incarceration than severe mental illness itself ( 23 ). Consequently, the hypothesis that untreated psychiatric symptoms are the primary explanation for the high rates of mental illnesses among jail and prison inmates deserves further evaluation.
The aim of this study was to describe risk of incarceration among veterans receiving inpatient health services from the Department of Veterans Affairs (VA) and to identify risk factors for incarceration, including variables assessing access to VA care, presence of mental illness, presence of substance abuse and dependence, and presence of co-occurring disorders after adjustment for sociodemographic characteristics. Multiple cohorts of patients were entered into the study, from 1993 to 1997, in order to explore trends, in particular whether reduced access to psychiatric services after the 1996 closure of 80% of inpatient psychiatric treatment beds at the VA Connecticut Healthcare system was associated with increased rates of incarceration ( 24 ).
Methods
Sample
The sample consisted of all male veterans who received medical, surgical, psychiatric, or substance abuse inpatient services in the VA Connecticut Healthcare System between 1993 and 1997. Female veterans were excluded because there were insufficient numbers to conduct meaningful subanalysis. Data were unduplicated by taking each patient's first recorded inpatient stay within the five-year time frame, which meant that the fiscal year 1993 cohort, which had no exclusions, was substantially different from subsequent cohorts. Demographic, clinical, and utilization data were extracted from VA administrative electronic databases along with Social Security numbers and other pertinent demographic data necessary for linkage with incarceration data from the state Department of Correction. Once the applicable demographic and clinical variables were extracted, the data were merged with the Department of Correction database of individuals incarcerated between 1993 and 1997 in order to identify VA patients who were incarcerated within one year after their hospital discharge. The identified sample consisted of a total of 36,385 veterans of whom 36,157 had no match for incarcerations and 228 (.63%) had such a match.
This study was approved by the Human Investigations Committees at the VA Connecticut Healthcare System, Yale University, and by the Connecticut Department of Correction.
Analyses
Analyses proceeded in several steps. First, the sample was divided into two groups: those with a match of incarceration in the State of Connecticut Department of Correction records and those without. Incarceration records were used instead of arrest records because arrest records were not readily available.
Second, demographic, clinical, and criminal justice factors were compared across groups to assess differences for significance. Third, a logistic regression model of the likelihood of incarceration was constructed. It included demographic characteristics, year of inpatient discharge, and receipt of various health and mental health services in the six months before the index discharge and diagnostic indicators. A second, reduced logistic regression model was constructed in an effort to produce a more parsimonious model. Finally, odds ratios were calculated from both models to explore risk factors for incarceration among the cohorts.
Results
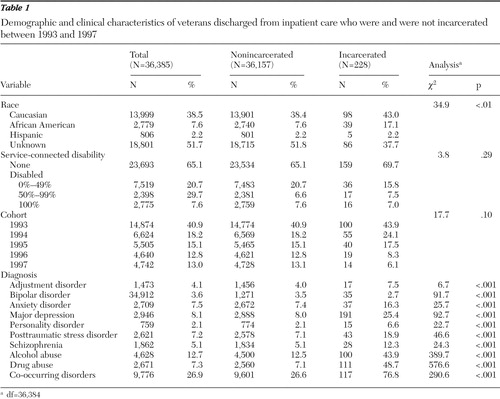
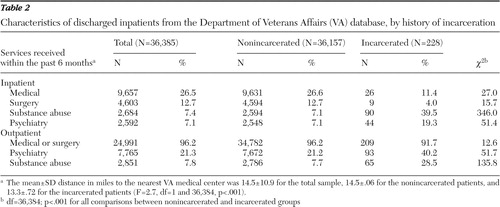
Summary statistics are provided in Tables 1 and 2 . Mean±SD age was 57.5±15.5 for the entire sample, 57.7±.08 for the nonincarcerated group, and 40.6±1.02 for the incarcerated group. Over the entire sample 38.5% were Caucasian, 7.6% were African American, 2.2% were Hispanic, and 51.7% were of unknown race. Because race is not a required field within the VA database, unknown race was kept as a category in order to avoid a loss of more than 50% of the sample in the data analysis. Among veterans whose race was identified, African Americans were significantly overrepresented in the incarcerated group. The nonincarcerated and incarcerated veterans did not differ in their extent of service-connected disability.
 |
 |
Because records were unduplicated by taking the first discharge in the study period, the largest proportion of the sample was discharged in 1993 (40.9%). The distribution of the sample across other years was 18.2% from 1994, 15.1% from 1995, 12.8% from 1996, and 13.0% from 1997. The rates of incarceration were quite low: .7% in the 1993 cohort, .8% in the 1994 cohort, .7% in the 1995 cohort, .4% in the 1996 cohort, and .3% in the 1997 cohort. Overall results of the chi square test indicated no statistically significant association between year of discharge cohort and risk of incarceration.
In bivariate analyses the incarcerated group was significantly more likely than the nonincarcerated group to have a psychiatric diagnosis. All psychiatric conditions were represented except for bipolar disorder, where incarceration was associated with a lower likelihood of the disorder ( Table 1 ). Similarly, bivariate analyses showed that incarcerated patients were significantly more likely to have a diagnosis of drug abuse, alcohol abuse, or co-occurring disorders.
Table 3 presents two logistic regression models of the risk of incarceration. Diagnostic histories of drug abuse, alcohol abuse, and major depression were significantly related to risk of incarceration in the full model. No other psychiatric diagnoses, demographic variables, or treatment history variables were associated with risk of incarceration. The reduced model had similar results. Neither year of discharge nor diagnosis of schizophrenia or co-occurring disorders was predictive of incarceration in either model. Inpatient substance abuse treatment in the previous six months was associated with an elevated risk of incarceration only in the reduced model.
 |
Discussion
This study examined the differences between VA patients with and without mental health treatment histories and their risk of incarceration. Our analysis of five annual cohorts included all veterans discharged from any medical, surgical, psychiatric, or substance abuse inpatient unit within the VA Connecticut Healthcare System between 1993 and 1997. Our analysis of this large regional sample suggests several conclusions. First, similar to some other studies ( 12 , 17 , 25 ), in this study, although mental illnesses were a significant factor in bivariate analyses, they were generally not independent risk factors for incarceration after adjustment for other factors, especially diagnoses of substance abuse or dependence. Of all the psychiatric disorders, only depression was associated with an increased risk of incarceration in multivariate analyses. The strongest predictors of incarceration in all analyses were diagnoses of alcohol and drug abuse and dependence, along with receipt of inpatient substance abuse care.
Despite the higher risk of incarceration among veterans with depression, severe and persistent mental illness as usually conceptualized (schizophrenia and bipolar disorder) was not predictive of incarceration in these data, after adjustment for potentially confounding factors. It has been suggested that untreated psychiatric symptoms, particularly psychotic symptoms, are an important risk factor for incarceration ( 20 ). In our data, however, the sample was limited to persons who received VA inpatient health care services. Thus the lack of an association may be explained by the ready access to treatment among these veterans, and as a result, fewer untreated symptoms. A recent meta-analysis failed to show a strong relationship between clinical factors and recidivism. Demographic characteristics, criminal history, and deviant lifestyles showed far more predictive value ( 26 ).
Prior studies have demonstrated a robust association between alcohol and drug abuse and incarceration among persons with severe mental illnesses ( 17 , 18 ). Many studies have shown that there is a high prevalence of alcohol and drug abuse within incarcerated populations ( 3 ) and that alcohol and drug abuse is associated with numerous poor outcomes among those with schizophrenia, including involvement with the criminal justice system ( 15 , 27 ). Indeed, many of the outpatient treatment programs that have garnered attention recently are specifically intended for offenders with mental illness and histories of treatment nonadherence, criminal justice involvement, and alcohol and drug abuse ( 19 , 20 , 21 ). Consequently, one might have expected those with co-occurring disorders to have the greatest risk of incarceration.
However, with our data, substance use disorders were the strongest and the only independent predictors of incarceration. There was no effect of co-occurring disorders on incarceration independent of the main effect of having a substance use disorder. These results are consistent with other studies that have demonstrated a high prevalence of substance use disorders among inmates without mental illness ( 28 , 29 ). Whether persons with mental illness are arrested mostly on drug charges remains unknown; however, such a finding would suggest that offenders with mental illness share common risk factors with offenders without mental illness. Thus an open question is whether, in treated samples like ours, mental illness alone increases the likelihood of incarceration or if alcohol and drug abuse or dependence represents the overriding risk factor of incarceration among offenders with serious mental illness and those without. Because drug abuse is associated with numerous psychiatric comorbidities ( 30 ), the high prevalence of reported mental illnesses within correctional institutions could primarily reflect the risk imposed by alcohol and drug abuse rather than by schizophrenia and other serious mental illnesses.
Surprisingly, our results did not show an independent link between personality disorders (specifically, antisocial personality disorder) and incarceration. Given the expected association between antisocial personality disorder and illegal conduct, these results suggest that incarceration with these disorders may also be mediated by substance abuse and dependence, at least in treated populations. Alternatively, given the overall low prevalence of diagnosed personality disorders within our sample (2.1%), it is possible that personality disorders were underreported in this administrative data set. This assumption is buttressed by findings showing an association between childhood conduct problems and acts of serious violence among adults with schizophrenia ( 31 , 32 ).
A common claim derived from the criminalization hypothesis of mental illness is that widespread closure of mental health beds has resulted in increased incarceration among persons with severe mental illness ( 33 ). Our study, however, does not appear to support this assertion. In 1996, 80% of the VA inpatient psychiatric beds were closed in Connecticut ( 24 ), a pattern that was repeated to a more modest degree over the next several years across the VA system nationally. A limited number of studies have demonstrated that these closures were not associated with increased incarceration, state hospital inpatient service use, suicide, or cost among veterans with mental illnesses ( 34 , 35 , 36 ). It has been hypothesized that the increased availability of outpatient services may account for the lack of increased inpatient demand across state systems and the absence of worse outcomes among veterans during this period of system change ( 35 , 37 ). This study adds support to these findings, because there was no statistically significant change in the proportion of veterans incarcerated during the study period, even though the baseline cohort could have been expected to have the highest risk because no patients were excluded as a result of prior hospitalization. In contrast, the general population of Connecticut during the same period experienced a steady increase in incarceration rates ( 38 ).
Although persons with schizophrenia were overrepresented in the incarcerated sample on bivariate analysis, our results do not suggest that schizophrenia or other related severe mental illnesses were significant independent risk factors for incarceration. Instead, our results are consistent with criminological models suggesting that alcohol and drug abuse are largely responsible for incarceration risk ( 20 , 26 , 39 ). Programs designed to prevent incarceration of people with mental illness should perhaps focus on alcohol and drug abuse treatment as the central component in addition to management of the symptoms of the psychiatric disorder. Because drug abuse represents not only the pathological process of addiction but also an illegal behavior, interventions for persons in the criminal justice system with drug abuse and with or without mental illness optimally would be aimed at recidivism reduction ( 20 , 40 ). Such models favor a conceptualization of alcohol and drug abuse as problematic behaviors instead of secondary products of mental illnesses and therefore invest in various methods of legal leverage to attain community tenure. Given the shared risk factors for incarceration among mentally ill and non-mentally ill offenders, these criminological models may prove fruitful in reducing incarceration among populations with severe mental illness.
Several limitations of this study require comment. The study was limited to patients hospitalized in the VA Connecticut health care system and thus includes an older male population with access to free health care services. It remains unknown whether our results can be generalized to other populations. Second, all sociodemographic and diagnostic measures were based on administrative data rather than primary surveys or structured diagnostic interviews. Third, our study lacked measures of symptomatology and severity of psychopathology. A distinctive strength of the study was the opportunity to link health system and criminal justice data.
Conclusions
The arrest and incarceration of persons with mental illness have garnered deserved public and professional concern. Such concerns have endured for the past 25 years, since the modern induction of the criminalization hypothesis by Abramson ( 41 ). Substance use disorders, as suggested by this study, may be the primary risk factors for incarceration. Thus unique conceptual models that explore recidivism factors outside of traditional mental illness symptoms might prove useful in that they take into account known predictive models used in correctional services. The hypothesis that reductions in inpatient mental health services have increased the risk of incarceration among people with mental illness was not confirmed by our findings. Services for offenders with mental illness should therefore focus on broader approaches that can reduce risk factors, such as drug abuse, unstable housing, and unemployment, which threaten community tenure and appear to be the most likely risk factors for incarceration by persons with mental illness.
Acknowledgments and disclosures
The authors thank the Connecticut Department of Correction for its assistance in this project.
The authors report no competing interests.
1. Lamb H, Weinberger L: Persons with severe mental illness in jails and prisons: a review. Psychiatric Services 49:483–492, 1998Google Scholar
2. Thompson M, Reuland M, Souweine D: Criminal justice/mental health consensus: improving responses to people with mental illness. Crime and Delinquency 49:30–51, 2003Google Scholar
3. Teplin L: Psychiatric and substance abuse disorders among male urban jail detainees. American Journal of Public Health 84:290–293, 1994Google Scholar
4. Teplin L: The prevalence of severe mental disorder among male urban jail detainees: comparison with the Epidemiologic Catchment Area Program. American Journal of Public Health 80:663–669, 1990Google Scholar
5. Ditton L: Bureau of Justice Statistics Report: Mental Health and Treatment of Inmates and Probationers. Washington, DC, US Department of Justice, Bureau of Justice Statistics, 1999Google Scholar
6. James DJ, Glaze LE: Mental Health Problems of Prison and Jail Inmates. Washington, DC, US Department of Justice, Bureau of Justice Statistics, 1999Google Scholar
7. Health care reform for Americans with severe mental illnesses: report of the National Advisory Mental Health Council. American Journal of Psychiatry 150:1447–1465, 1993Google Scholar
8. Kessler R, Demler O, Frank R, et al: Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine 352:2515–2523, 2005Google Scholar
9. Lafayette J, Frankle W, Pollock A, et al: Clinical characteristics, cognitive functioning, and criminal histories of outpatients with schizophrenia. Psychiatric Services 54:1635–1640, 2003Google Scholar
10. Mcguire J, Rosenheck R, Kasprow W: Health status, service use, and costs among veterans receiving outreach services in jail or community settings. Psychiatric Services 54:201–207, 2003Google Scholar
11. Muntaner C, Wolyniec P, Mcgrath J, et al: Arrest among psychotic inpatients: assessing the relationship to diagnosis, gender, number of admissions, and social class. Social Psychiatry and Psychiatric Epidemiology 33:274–282, 1998Google Scholar
12. Quanbeck C, Stone D, McDermott B, et al: Relationship between criminal arrest and community treatment history among patients with bipolar disorder. Psychiatric Services 56:847–852, 2005Google Scholar
13. Swanson J, Van Dorn R, Monahan J, et al: Violence and leveraged community treatment for persons with mental disorders. American Journal of Psychiatry 163:1404–1411, 2006Google Scholar
14. Erickson S: A retrospective examination of outpatient commitment in New York. Behavioral Sciences and the Law 23:627–645, 2005Google Scholar
15. Swartz M, Swanson J, Hiday V, et al: Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Psychiatric Services 155:226–231, 1998Google Scholar
16. Hunt G, Bergen J, Bashir M: Medication compliance and comorbid substance abuse in schizophrenia: impact on community survival 4 years after a relapse. Schizophrenia Research 54:253–264, 2002Google Scholar
17. Pandiani J, Rosenheck R, Banks S: Elevated risk of arrest for Veteran's Administration behavioral health service recipients in four Florida counties. Law and Human Behavior 27:289–297, 2003Google Scholar
18. Clark R, Ricketts S, McHugo G: Legal system involvement and costs for persons in treatment for severe mental illness and substance use disorders. Psychiatric Services 50:641–647, 1999Google Scholar
19. Lamberti J, Weisman R, Faden D: Forensic assertive community treatment: preventing incarceration of adults with severe mental illness. Psychiatric Services 55:1285–1293, 2004Google Scholar
20. Lamberti J: Understanding and preventing criminal recidivism among adults with psychotic disorders. Psychiatric Services 58:773–781, 2007Google Scholar
21. Lurigio A: Persons with serious mental illness in the criminal justice system: background, prevalence, and principles of care. Criminal Justice Policy Review 11:312–328, 2000Google Scholar
22. Griffin P, Steadman H, Petrila J: The use of criminal charges and sanctions in mental health courts. Psychiatric Services 53:1285–1289, 2002Google Scholar
23. Junginger J, Claypoole K, Laygo R, et al: Effects of serious mental illness and substance abuse on criminal offenses. Psychiatric Services 57:879–882, 2006Google Scholar
24. Rosenheck R, Frisman L, Essock S: Impact of VA bed closures on use of state psychiatric services. Journal of Behavioral Health Services and Research 28:58–66, 2001Google Scholar
25. Prince J: Incarceration and hospital care. Journal of Nervous and Mental Disease 194:34–39, 2006Google Scholar
26. Bonta J, Law M, Hanson K: The prediction of criminal and violent recidivism among mentally disordered offenders: a meta-analysis. Psychological Bulletin 123:123–142, 1998Google Scholar
27. Swartz M, Wagner H, Swanson J, et al: Substance use in persons with schizophrenia: baseline prevalence and correlates from the NIMH CATIE study. Journal of Nervous and Mental Disease 194:164–172, 2006Google Scholar
28. Mumola C: Substance Abuse and Treatment, State and Federal Prisoners, 1997: Bureau of Justice Statistics Special Report. Washington, DC, US Department of Justice, Office of Justice Programs, 1999Google Scholar
29. Webster T, Garrity C, Narevic E, et al: Prisoners with substance abuse and mental health problems: use of health and health services. American Journal of Drug and Alcohol Abuse 31:1–20, 2005Google Scholar
30. Regier D, Farmer D, Rae B, et al: Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. JAMA 264:2511–2518, 1990Google Scholar
31. Swanson J, Swartz M, Van Dorn R, et al: A national study of violent behavior in persons with schizophrenia. Archives of General Psychiatry 63:490–499, 2006Google Scholar
32. Swanson J, Van Dorn R, Swartz M, et al: Alternative pathways to violence in persons with schizophrenia: the role of childhood antisocial behavior problems. Law and Human Behavior, in pressGoogle Scholar
33. Fisher W, Silver E, Wolff N: Beyond criminalization: toward a criminologically informed framework for mental health policy and services research. Administration and Policy in Mental Health and Mental Health Services Research 33:544–557, 2006Google Scholar
34. Desai M, Rosenheck R: Trends in discharge disposition, mortality, and service use among long-stay psychiatric patients in the 1990s. Psychiatric Services 54:542–548, 2003Google Scholar
35. Rosenheck R, Banks S, Pandiani J: Does closing inpatient beds in one public mental health system result in increased use of hospital services in other systems? Mental Health Services Research 2:183–189, 2000Google Scholar
36. Rosenheck R, Banks S, Pandiani J, et al: Bed closures and incarceration rates among users of Veterans Affairs mental health services. Psychiatric Services 51:1282–1287, 2000Google Scholar
37. Desai R, Rosenheck R: The interdependence of mental health service systems: the effects of VA mental health funding on veterans' use of state mental health inpatient facilities. Journal of Mental Health Policy and Economics 3:61–67, 2000Google Scholar
38. Total Supervised Population. Hartford, Conn, Connecticut Department of Correction, 2006Google Scholar
39. Andrews D, Bonta J: Psychology of Criminal Conduct. Dayton, Ohio, Anderson, 2006Google Scholar
40. Skeem J, Louden J: Toward evidence-based practice for probationers and parolees mandated to mental health treatment. Psychiatric Services 57:333–342, 2006Google Scholar
41. Abramson MF: The criminalization of mentally disordered behavior: possible side-effect of a new mental health law. Hospital and Community Psychiatry 23:101–105, 1972Google Scholar



