Pharmacists' Role in Depression Care: A Survey of Attitudes, Current Practices, and Barriers
Depression constitutes a major public health challenge in industrialized countries. Major depressive disorder is highly prevalent, recently estimated at 6.6% in the United States ( 1 ). The disorder has a severe impact on those affected ( 2 ) and on economic resources, such as lost productivity ( 3 ). Despite the availability of effective treatment, current depression care is far from optimal ( 1 ), including inadequate recognition, diagnosis, and treatment by care providers; stigma toward those with the condition; and patients' lack of knowledge about their disorder and poor medication adherence ( 4 ).
One element in improving depression care could be to expand the role of nonclinical community professionals who come into contact with people with depression. The European Alliance Against Depression (EAAD) is one example where this approach is piloted ( 5 ). Our study, which is part of EAAD, focuses on pharmacists, who are an underutilized health care resource ( 6 , 7 ) and should be considered in the care of patients with depression ( 8 , 9 ). They have frequent contact with such patients, considering that up to 20% of the prescriptions that pharmacists fill include an antidepressant ( 8 ). Pharmacists often maintain a trusting relationship with patients, who typically visit only one pharmacy ( 10 ); they also have expertise in medication management and are easily available to consumers ( 8 ). This position enables pharmacists to provide several services important to depression care for which primary care providers often lack time, such as providing patient education and support, enhancing medication adherence, monitoring treatment effectiveness, and identifying adverse effects ( 11 ).
This potential role of pharmacists in the care of depression relates to the advocated increase in pharmacists' scope of practice and to the emergence of an area of care designated as "pharmaceutical care" ( 12 ). This concept proposes a changing role for pharmacists, moving from the traditional medication-oriented dispensing role toward a patient-centered model of practice ( 13 ). In this model, pharmacists assume responsibility for therapeutic outcomes, such as adherence ( 14 ), and use their medication-related expertise to assist patients ( 15 ), such as by patient education, medication monitoring, and increased collaboration with prescribing physicians ( 16 ). In the specific context of depression care, the pharmacist can perform several useful roles, described next.
A first set of roles for pharmacists could be to provide information to the patient about depression and antidepressant medication and to support medication adherence. Patients with depression often inadequately understand antidepressant medication and harbor many unfounded beliefs related to it, which is key to their general low adherence ( 17 ). They appear to have a substantial need for information about depression and its medication and ongoing, strong encouragement for antidepressant adherence ( 18 ), which general practitioners may have more limited opportunity than pharmacists to provide ( 8 ). Pharmacists can provide information about antidepressants, address common misconceptions, and assess patients' understanding, and they have been shown to influence patients' attitudes toward depression ( 19 ) and toward antidepressants ( 10 , 20 , 21 ), to enhance adherence ( 20 , 22 , 23 ), and to improve treatment outcomes ( 13 , 22 ). Furthermore, physicians are reported to be comfortable with pharmacists' providing patient education ( 24 ).
A second set of roles for pharmacists could be to monitor patients diagnosed as having depression, particularly regarding medication adherence ( 10 , 25 ), medication effectiveness ( 22 , 23 ), and the presence of side effects ( 9 , 11 ). Patients who do not respond to treatment or present severe side effects should be referred back to their prescribing physician ( 9 ). Maintaining a trusting relationship and documenting the patient's medication history, for example by electronic patient records ( 16 ), are prerequisites to this role ( 18 ) and in fact begin as soon as a patient becomes a customer at the pharmacy. Furthermore, for pharmacists to monitor patients, collaboration and communication with general practitioners are needed ( 8 , 12 ). Current links between pharmacists and general practitioners, however, are generally poor. In a study from the United Kingdom on depression management, half of surveyed pharmacists reported little or no contact with general practitioners, and one in three reported some (practical and informal) contact ( 8 ). We expect the same for Belgium, where pharmacists work relatively independently from general practitioners, who treat most patients with diagnoses of depression (involved in the care of 85% of this group of patients) ( 26 ).
The above-mentioned pharmacists' roles are related to service provision to patients with a diagnosis of depression who contact their pharmacist for antidepressants. However, the pharmacist's role may also extend to patients who are not aware of or do not seek help for depression. On recognition of symptoms of untreated depression, the pharmacist may suggest that patients visit their general practitioner for further evaluation ( 9 ).
The implementation of these potential pharmacists' roles may be hindered by barriers. Several barriers have been reported in providing pharmaceutical care in general, including barriers at the system level (vague role description, interprofessional conflicts, inadequate remuneration of pharmacists for this task, lack of information about or relationship with the patient, time constraints, and lack of privacy in the pharmacy) and at the pharmacist level (lack of professionalism, discomfort during patient interactions, and insufficient skills to communicate about sensitive issues) ( 16 , 27 ). Specifically, patient education is not yet a routine task performed by pharmacists, but it is delivered ad hoc in some cases ( 16 ) and at the patient's initiation ( 28 ). This risks pharmaceutical care to be provided mainly at the request of the patient, because such requests are known to influence care providers ( 29 ).
Overall, however, pharmacists are already successfully involved in pharmaceutical care for patients with chronic physical diseases such as asthma, diabetes, or hypertension ( 11 ). The same potential holds for the care of patients with mental illnesses, such as depression, but despite the high number of such patients seen by pharmacists, this role is yet to be established ( 9 , 12 ). Some first studies report on pharmacists' attitudes, current practices, and barriers regarding the care of patients with mental illnesses in general. In a study in the United Kingdom nearly half of pharmacists expressed being more interested and more likely to perform pharmaceutical care activities for patients with a mental illness compared with a physical illness, whereas less than 20% reported the reverse ( 30 ). In a Canadian study, community pharmacists, despite generally positive attitudes, reported feeling more uncomfortable discussing symptoms and medications with patients who had mental illnesses than with patients who had cardiovascular problems ( 19 ). Patients with mental illnesses therefore received fewer pharmacy services than patients with cardiovascular problems.
However, no such studies have been carried out specifically on pharmacists' involvement in providing depression care, despite depression being the most common mental illness. It is important, however, to be aware of pharmacists' attitudes and perceived barriers to providing depression care because these are likely to influence the extent to which this new role will be adopted ( 31 , 32 ). This study therefore explored pharmacists' attitudes, current practices, and perceived barriers concerning depression care.
Our main research questions were as follows: what are the current attitudes, practices, and perceived barriers of pharmacists in regard to providing depression care? Is there a discrepancy between these attitudes and current practices? Is there a difference in providing this role for patients with depression in comparison with patients with other, physical conditions? Which pharmacists' characteristics and which perceived barriers are associated with providing depression care? To what degree do pharmacists currently cooperate with general practitioners and other partners in providing depression care? What is the desired level of cooperation?
Methods
Survey instrument
A survey instrument was constructed to address the research questions. One section dealt with pharmacists' role in depression care. On the basis of previous research ( 19 ) we delineated a set of nine potential roles: two prerequisites (maintaining a trusting relationship and knowing the patient's medication history), two on providing information (about the disorder and about its medication), one on support, three on monitoring (side effects, adherence, and referring patients to their doctor), and one on detection. We investigated the attitude toward these roles ("to what extent do you agree you should provide …") as well as current practice in taking up these roles ("to what degree do you currently provide …"). Attitude items were assessed on a 5-point Likert scale with responses ranging from strongly disagree to strongly agree. Practice items were assessed on a 4-point Likert scale ranging from "I provide … to no patients" to "I provide … to all patients." No "undecided" option was available for practice items, because these items concerned facts, not attitudes. All items were formulated both in reference to depression and to other, physical diseases. Participants were also asked to indicate perceived barriers (from a list including pharmacist-, patient-, and system-level barriers) in taking up these roles.
In the second section pharmacists were asked with which partners they wanted to collaborate in the depression care of an individual patient and what the current level of cooperation was with these partners (using a 5-point Likert scale ranging from 1, indicating no cooperation, to 5, discussing how to deal with individual patients). Perceived barriers to this cooperation were listed. In addition, the following background characteristics were gathered: age, gender, occupational experience, pharmacist's function in the pharmacy, and personal and professional experience with depression. Professional experience was measured by the estimated frequency at which pharmacists saw patients with depression in their practice (on a 5-point Likert scale ranging from 1, never, to 5, daily). To ascertain pharmacists' personal experience with people with depression, an item asked whether they had ever encountered people with depression in their personal environment.
A first version of the survey was piloted in a group of pharmacists not participating in the main study, and content and face validity were discussed with experts of the National Board of Pharmacists.
Survey sample
The survey was mailed to a random sample of 200 of the 305 pharmacies in the region of Bruges-Ieper (Belgium) in May 2005. All pharmacies were community based; hospital pharmacies are uncommon in Belgium. The survey, including a postage-paid reply envelope, could be filled out by any licensed pharmacist in the pharmacy to which the survey was mailed. Formal ethical permission was not required for this study, but the covering letter asked for consent and stressed anonymity and confidentiality. After one month a reminder was sent.
Data analysis
Statistical analyses were carried out with SAS version 9.1. Descriptive statistics were calculated. Discrepancy scores between attitude and current practice with regard to each role were obtained by subtracting the current practice score (level of realization) for a role from the related item measuring the attitude toward the same role (level of importance). Discrepancy occurred when a role was viewed as more important than it was being realized in practice. With discrepancy scores potentially ranging from 0 to 4, a score of at least 3 was regarded as a high discrepancy ( 33 ). The total depression care score was obtained by summing the nine role scores (current practice), and its reliability (internal consistency) was assessed by Cronbach's alpha. The relations of pharmacists' characteristics, perceived barriers, and level of partner cooperation to the total depression care score (interval variable) were determined by analysis of variance and to individual role scores (ordinal variables) by chi square tests.
Results
A total of 69 pharmacists, 36 (52%) men and 33 (48%) women completed the survey, representing a 35% response rate. Their ages ranged from 25 to 67 years (mean±SD of 45.2± 11.1), which resembles the mean age (42.1) of the total population of pharmacists in the study region. Most of the responses (N=62, or 90%) came from pharmacist-owners, with another 10% from adjunct-pharmacists. Responding pharmacists had been practicing for a range of one year to 43 years, with a mean of 19.3±11.5 years in practice. Most pharmacists had extensive professional and personal experience with patients with depression: 52 (75%) saw such patients at least weekly, including 27 (39%) who saw them daily and 56 of 68 (82%) who reported having encountered people with depression in their personal environment.
Pharmacists' attitude toward their potential role in depression care was very positive ( Table 1 ): for all nine roles, at least 85% (N=59) agreed that they should provide this service. Current practice was rather low, however: most pharmacists reported providing each of several roles to few or no patients. The lowest score was observed for providing information on depression, with 83% (N=57) providing information to few or no patients. Consequently, for most roles a discrepancy was observed. The scores with the highest discrepancy were observed for providing information on depression (26, or 38% of respondents, had a high discrepancy score), monitoring adherence to depression medication (N=25 of 68, or 37%), providing information on depression medication (N=24, or 35%), and maintaining a trusting relationship with patients with depression (N=19, 28%). On the other hand, a high level of current practice was observed for knowing the patient's medication history, advising the patient to consult a doctor, and providing support to patients.
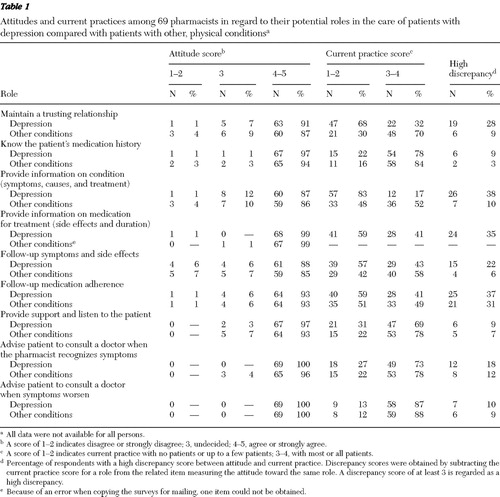 |
The comparison of care provision for patients with depression and for patients with other, physical conditions showed several differences. For every role pharmacists' attitude toward providing it was equally or more positive in regard to patients with depression than for patients with other conditions. However, every role was being realized in practice to a higher degree with patients with conditions other than depression. Consequently, compared with depression, all items on other conditions had lower discrepancy between attitude and practice. The largest differences were observed on maintaining a trusting relationship, which 70% of pharmacists (N=48) provided to most or all patients with other conditions compared with only 32% (N=22) to patients with depression, and on providing information on the condition (N=36, or 52%, compared with N= 12, or 17%).
The main perceived barrier to providing depression care ( Table 2 ) was a lack of education in mental health issues (reported by 50 pharmacists, or 73% of the sample). Other frequently reported barriers were lack of time with individual patients (N=39, or 57%), lack of information about patients and their treatment (N=37, or 54%), lack of privacy in the pharmacy (N=32, or 46%), and difficulties in communicating with patients with depression (N=26, or 38%).
 |
The internal consistency of the total depression care scale was good (Cronbach's α =.76). No pharmacists' characteristics were significantly associated with providing depression care. However, pharmacists who indicated a lack of privacy in the pharmacy as a perceived barrier had a significantly lower score on total depression care (F=7.16, df=1 and 62, p=.01) and on the item about providing support ( χ2 =6.17, df=1, p=.013) compared with those who did not indicate this barrier. Furthermore, in comparison with pharmacists who reported a low cooperation level with general practitioners, those who reported high cooperation scored significantly higher on the items about maintaining a trusting relationship ( χ2 =3.86, df=1, p=.05) and providing information about depression ( χ2 = 6.48, df=1, p=.01) and about its medication ( χ2 =6.75, df=1, p=.009).
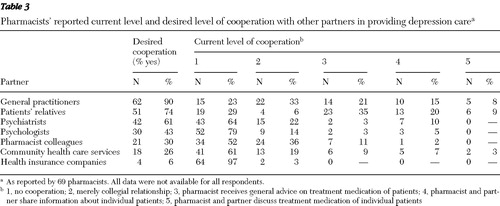
Concerning cooperation in the care of patients with depression, pharmacists' desired partners ( Table 3 ) were mainly general practitioners (N=62, or 90% of respondents) and the patients' relatives (N=51, or 74%). The current level of cooperation was rather low: 56% (N=37) of pharmacists did not collaborate with general practitioners or merely maintained a collegial relationship, receiving no advice or not sharing information about individual patients. The most frequent perceived barriers ( Table 4 ) were that cooperation across professions was unusual (N=38, or 55% of respondents) and that information was hard to get (N=36, or 52%).
 |
 |
Discussion
Pharmacists in this study generally endorsed a very positive attitude toward their potential role in depression care and had ample opportunity to act accordingly, as most had frequent contact with patients with depression. Their general willingness and the importance they perceived in this potential new role shows that depression care was acceptable to these pharmacists, which is promising for the future development of this role. However, fulfilling specific roles of care was more difficult when patients had depression in comparison with patients with other, physical conditions. This finding specific to depression care is in line with findings of two earlier studies on pharmaceutical care for mental illness in general ( 19 , 30 ).
Discrepancy scores between pharmacists' attitudes and current practice regarding their potential roles illuminated this finding. For patients with depression, much more than for patients with other, physical conditions, pharmacists perceived the nine specific roles of care as more important than they actually put into practice. This indicates difficulties in providing depression care, especially in regard to providing information on depression (medication), monitoring medication adherence, and maintaining a trusting relationship with the patient. Because fulfilling pharmacists' potential roles was shown to be possible when patients had conditions other than depression, we suspect specific barriers in performing these roles for patients with depression.
The most important perceived barrier reported in this study was a lack of education in mental health issues; this topic is not sufficiently covered in pharmacists' regular curriculum ( 16 ). If pharmacists are to take up a role in depression care, training programs are needed to acquire necessary knowledge and skills in providing information on depression and on antidepressant medication. Such role-specific training has proved to enhance the implementation of pharmacists' new roles ( 32 ). Furthermore, the participation of patients with a mental illness in such training has been shown to improve pharmacists' attitudes toward this group of patients ( 34 ) and may facilitate maintaining a trusting relationship with them.
Other important perceived barriers were a lack of time for individual patients, a lack of privacy in the pharmacy, and a lack of information about patients and their medication, which is consistent with previous research on mental illness in general ( 8 , 19 ). Increasing the collaboration with general practitioners may tackle the information barrier and improve pharmacists' provision of information to patients, to which cooperation with general practitioners was significantly related. In this study, the current level of such cooperation was rather low, primarily because it is not customary between these professions. This especially impedes pharmacists in following up with patients about depression symptoms and medication—information that is needed from general practitioners and to whom pharmacists need to provide feedback. Involving local general practitioners in training programs for pharmacists on depression may be one way to increase cooperation and break down barriers ( 32 ). Increased general practitioner-pharmacist collaboration, however, will need to consider the issue of patient confidentiality.
Further research is needed to confirm the results of this exploratory study in larger samples. Further, it should address patients' and other care providers' perceptions of pharmacists' role in depression care, the impact of pharmacists' involvement in depression care, and ways to resolve barriers to it.
This study has some methodological limitations. First, survey responses were self-reported. Second, the survey response rate was relatively low, although comparable with that of similar studies ( 19 ), which may have biased the results. Participating pharmacists may have been relatively more interested in or positive toward the topic of depression. Finally, generalizability of the results may be limited to health systems in which pharmacists operate relatively independently from primary care, as in Belgium.
Conclusions
Pharmacists' willingness to take up a role in depression care is high, but its realization in practice is impeded by several barriers, such as a lack of training in mental health issues and absence of a culture of cooperation with general practitioners. These findings indicate that an important community resource—pharmacists—is currently underused to meet the needs of patients with depression. For pharmacists to effectively take up depression care these barriers need to be addressed. Specific training programs for pharmacists on providing depression care, preferably involving general practitioners and patients, are therefore needed. The results of this study may be useful to inform such training programs.
Acknowledgments and disclosures
This study is part of the European Alliance Against Depression (EAAD) project and is financed by the European Commission and the Province of West-Flanders (Belgium). Special thanks go to Annemie Zwaenepoel, R.Ph., for her enthusiastic support of this study.
The authors report no competing interests.
1. Kessler R, Berglund P, Demler O, et al: The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 289: 3095–3105, 2003Google Scholar
2. Moussavi S, Chatterji S, Verdes E, et al: Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370:851–858, 2007Google Scholar
3. Stewart W, Ricci J, Chee E, et al: Cost of lost productive work time among US workers with depression. JAMA 289:3135–3144, 2003Google Scholar
4. Goldman L, Nielsen N, Champion H: Awareness, diagnosis and treatment of depression. Journal of General Internal Medicine 14:569–580, 1999Google Scholar
5. Hegerl U, Wittmann M, Arensman E, et al: The 'European Alliance Against Depression (EAAD)': a multifaceted, community-based action programme against depression and suicidality. World Journal of Biological Psychiatry 9:51–58, 2008Google Scholar
6. Beney J, Bero L, Bond C: Expanding the role of outpatient pharmacists: effects on health services utilization, costs, and patient outcomes. Cochrane Database of Systematic Reviews 2:336, 2000Google Scholar
7. Planas L, Kimberlin C, Segal R, et al: A pharmacist model of perceived responsibility for drug therapy outcomes. Social Science and Medicine 60:2393–2403, 2005Google Scholar
8. Badger F, Kingscote-Davies T, Nolan P: The pharmacist's role in the medicinal management of depression. Nursing Standard 16:33–40, 2002Google Scholar
9. Wells B: Underrecognition and undertreatment of depression: what is the pharmacist's culpability? Pharmacotherapy 19: 1237–1239, 1999Google Scholar
10. Brook O, van Hout H, Nieuwenhuyse H, et al: Impact of coaching by community pharmacists on drug attitude of depressive primary care patients and acceptability to patients: a randomized controlled trial. European Neuropsychopharmacology 13:1–9, 2003Google Scholar
11. Boudreau D, Capoccia K, Sullivan S, et al: Collaborative care model to improve outcomes in major depression. Annals of Pharmacotherapy 36:585–591, 2002Google Scholar
12. American College of Physicians-American Society of Internal Medicine: Pharmacist scope of practice. Annals of Internal Medicine 136:79–85, 2002Google Scholar
13. Brook O, van Hout H, Nieuwenhuyse H, et al: Effects of coaching by community pharmacists on psychological symptoms of antidepressant users: a randomized controlled trial. European Neuropsychopharmacology 13:347–354, 2003Google Scholar
14. Fjortoft N, Zgarrick D: An assessment of pharmacists' caring ability. Journal of the American Pharmacists Association 43:483–487, 2003Google Scholar
15. Farris K, Schopflocher D: Between intention and behaviour: an application of community pharmacists' assessment of pharmaceutical care. Social Science and Medicine 49:55–66, 1999Google Scholar
16. Pronk M, Blom L, Jonkers R, et al: Community pharmacy and patient-oriented activities: the Dutch case. Patient Education and Counseling 46:39–45, 2002Google Scholar
17. Demyttenaere K: Compliance and acceptance in antidepressant treatment. International Journal of Psychiatry in Clinical Practice 5:S29–S35, 2001Google Scholar
18. Bungay M, Adler D, Rogers W, et al: Description of a clinical pharmacist intervention administered to primary care patients with depression. General Hospital Psychiatry 26:210–218, 2004Google Scholar
19. Phokeo V, Sproule B, Raman-Wilms L: Community pharmacists' attitudes toward and professional interactions with users of psychiatric medication. Psychiatric Services 55:1434–1436, 2004Google Scholar
20. Brook O, van Hout H, Stalman W, et al: A pharmacy-based coaching program to improve adherence to antidepressant treatment among primary care patients. Psychiatric Services 56:487–489, 2005Google Scholar
21. Rickles NM, Svarstad BL, Statz-Paynter JL, et al: Pharmacist telemonitoring of antidepressant use: effects on pharmacist-patient collaboration. Journal of the American Pharmacists Association 45:344–353, 2005Google Scholar
22. Adler D, Bungay M, Wilson I, et al: The impact of a pharmacist intervention on 6-month outcomes in depressed primary care patients. General Hospital Psychiatry 26: 199–209, 2004Google Scholar
23. Finley P, Rens H, Pont J, et al: Impact of a collaborative pharmacy practice model on the treatment of depression in primary care. American Journal of Health-System Pharmacy 59:1518–1526, 2002Google Scholar
24. Ranelli P, Biss J: Physicians' perceptions of communication with and responsibilities of pharmacists. Journal of the American Pharmacists Association 40:625–630, 2000Google Scholar
25. Bultman D, Svarstad B: Effects of pharmacist monitoring on patient satisfaction with antidepressant medication therapy. Journal of the American Pharmacists Association 42:36–43, 2002Google Scholar
26. Bruffaerts R, Bonnewyn A, Van Oyen H, et al: Service use for mental disorders in Belgium: results of the Esemed study [in Dutch]. Tijdschrift voor Geneeskunde 60: 790–799, 2004Google Scholar
27. Planas L, Kimberlin C, Segal R, et al: A pharmacist model of perceived responsibility for drug therapy outcomes. Social Science and Medicine 60:2393–2403, 2005Google Scholar
28. Schommer J, Wiederholt J: Pharmacists' perceptions of patients' needs for counseling. American Journal of Hospital Pharmacy 51:478–485, 1994Google Scholar
29. Kravitz R, Bell R, Azari R, et al: Direct observation of requests for clinical services in office practice: what do patients want and do they get it? Archives of Internal Medicine 163:1673–1681, 2003Google Scholar
30. Cates M, Burton A, Wolley T: Attitudes of pharmacists toward mental illness and providing pharmaceutical care to mentally ill. Annals of Pharmacotherapy 39:1450–1455, 2005Google Scholar
31. Matheson C, Bond C, Mollison J: Attitudinal factors associated with community pharmacists' involvement in services for drug misusers. Addiction 94:1349–1359, 1999Google Scholar
32. Sheridan J, Strang J, Taylor C, et al: HIV prevention and drug treatment services for drug misusers: a national study of community pharmacists' attitudes and their involvement in service specific training. Addiction 92:1737–1748, 1997Google Scholar
33. Van Audenhove C, Van Humbeeck G, Spruytte N, et al: The Care Perception Questionnaire: an instrument for the assessment of the perspective of patients, family members, and professionals on psychiatric rehabilitation. European Journal of Psychological Assessment 17:120–129, 2001Google Scholar
34. Bell J, Johns R, Rose G, et al: A comparative study of consumer participation in mental health pharmacy education. Annals of Pharmacotherapy 40:1759–1765, 2006Google Scholar



