Psychiatrists' Ascertained Treatment Needs for Mental Disorders in a Population-Based Sample
Estimation of treatment needs for prevalent medical conditions is fundamental for policy development, budget allocation, and services organization. There is a growing concern about the high prevalence of mental disorders and the amount of unmet treatment needs in the population ( 1 ). However, need for treatment is not just a function of symptoms and severity but also duration, disability, and risk of relapse, compounded by the degree of surrounding support. Thus prevalence estimates are not an ideal proxy for service needs. Lifetime prevalence results do not measure current need. Also, a need for services may exist even when there is no current diagnosis, so that the meaningfulness of even point or period prevalence estimates is questionable.
Epidemiologic studies have used a proxy measure based on 12-month prevalence of mental disorders in the population, which is typically coupled with functional status of those with a disorder to estimate service needs. Two comprehensive psychiatric epidemiology efforts, the Epidemiologic Catchment Area (ECA) study and the National Comorbidity Survey (NCS), have been criticized for providing discordant prevalence estimates and for not considering the issue of clinical significance ( 2 ). Furthermore, with advances in psychiatric treatment, including different choices in psychopharmacology and psychotherapy, determination of needs for specific treatment modalities has become a complex issue in psychiatric epidemiology. Even after considerable efforts in this area, the question remains open: how much need for mental health services exists in the population, and how much of this need is being met?
Instead of using proxy measures, we used a population-based epidemiologic sample for this study. The sample was interviewed by psychiatrists who directly assessed the treatment needs of each participant. We defined need as the requirement for treatment as decided by experts in the field ( 3 ), and combining a population-based epidemiologic design with a thorough clinical assessment, we measured it directly. By using sampling weights we were able to estimate the prevalence of services needs for mental disorders by specific treatment modality. Using information collected on service utilization, we also assessed the prevalence of unmet needs in the population. Such estimates should inform service planning and public policy regarding resource allocation for mental illness. We hypothesized that estimates of prevalence of disorder would be higher than estimates of need for treatment and that there is a large contingent of unmet needs for mental health treatment in the population.
Methods
The original ECA study included two waves of interviews in the early 1980s at five sites across the United States. At the Baltimore site, a sample of 4,238 household residents was created with probability estimates to represent the target population of the 175,211 residents of East Baltimore. In the first wave, a total of 3,481 participants (82% of 4,238 designated) were interviewed with the Diagnostic Interview Schedule (DIS) ( 4 ). In a blind, independent follow-up called the Clinical Reappraisal study, psychiatrists examined a subsample of 810 participants from the total 3,481 (23%), which was stratified to include participants with specific DIS diagnoses of a mental disorder, as well as a random sample of the population ( 5 ).
In the early 1990s the Baltimore ECA follow-up study recontacted and interviewed participants from the original Baltimore ECA sample. The median period between the original and follow-up studies was 12.6 years. Of those known to be alive at the time of follow-up, 1,920 individuals (73%) were reinterviewed with the DIS. For this study, a stratified probability sample was generated from the Baltimore ECA follow-up study. Board-certified psychiatrists interviewed each person included in the final sample, using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) ( 6 ). Each psychiatrist completed a standard one-week SCAN training course at a World Health Organization training center. The mean time to complete the SCAN assessment was 116 minutes, and the interviews were conducted between 1993 and 1999. The psychiatrists were blind to the DIS diagnosis until the SCAN was completed. All available DIS information from the ECA study and the follow-up was reviewed after the SCAN interview, and a section on diagnosis, course of treatment, and treatment at the time of the interview was completed during the psychiatrist examination. This section included treatment history and a direct assessment of the need for treatment, tailored for each disorder, and was completed by the interviewing psychiatrist ( 7 ).
Weight calculations for the SCAN sample
Sampling weights were calculated for the original ECA study beginning with a weight related to the probability of selection, followed by an adjustment for nonresponse based on the full cross-classification of age, race, and sex and the census data for the original population. In the Baltimore ECA follow-up, the SCAN sample was selected according to four probability categories, each with a separate sampling weight. The selection process was designed to oversample persons who screened positive for current or lifetime disorders but included a random-sampling component that allowed weighting back to the general population. Category 1 included participants who received a DIS diagnosis in the first ECA wave, category 2 included those who received a DIS diagnosis in the ECA follow-up study, category 3 included those selected to the Clinical Reappraisal study without a DIS diagnosis in wave 1, and category 4 included persons who neither had a DIS diagnosis nor had participated in the Clinical Reappraisal study. These sampling weights were then used to adjust the prior weights from wave 1 to produce population-based estimates of prevalence. Standard errors for the weighted estimates were calculated with a bootstrapping procedure available in Stata software; the process was applied 10,000 times for each estimate ( 8 ). These weights accounted for unequal selection probability to the SCAN sample, and the weighted results represent the population, as compared with unweighted estimates that better represent the sample itself ( 9 ).
Defining diagnosis, need for treatment, and use of services
To compare prevalence measures with the estimates of need for treatment, we report on lifetime diagnosis of five prevalent psychiatric disorders included in the study: alcohol dependence, major depression, panic disorder, agoraphobia, and social phobia. Lifetime prevalence was based on psychiatrists' ascertained diagnoses. Need for treatment was rated separately for each disorder. Categories of need were tailored for each disorder ( Table 1 ) to allow estimates for each modality of treatment. The categories of use of services were also specific for each disorder and matched the categories of treatment need. In this analysis participants were categorized as having their need for treatment met if any use of service was recorded in the presence of need for treatment.
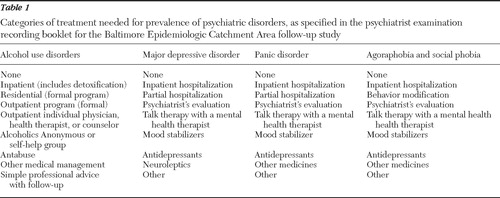 |
The definition of need was based on the psychiatrist's assessment. The psychiatrists, all practicing clinicians and board certified or eligible for board certification, were instructed to formulate a treatment plan for each diagnosis for each participant on the basis of the assumption that they were developing a treatment prescription for each client presenting in their clinic. Psychiatrists were expected to take all aspects of each participant's presentation into account after conducting a thorough and comprehensive psychiatric examination that included a personal history, medical and psychiatric history, personality assessment, and mental state examination.
Although we did not provide psychiatrists either an algorithm or a structured procedure to follow, this needs assessment was a close approximation to typical clinical procedure. It should be recognized that the treatment prescriptions reflect psychiatric practice in one U.S. academic department (Johns Hopkins University, where all the psychiatrists were trained and practiced) and could differ in an alternative location.
Results
The SCAN sample included 816 participants. Probability category 1 included 171 participants (21%), probability category 2 included 438 participants (54%), probability category 3 included 123 participants (15%), and probability category 4 included 84 participants (10%). Sample characteristics are summarized in Table 2 .
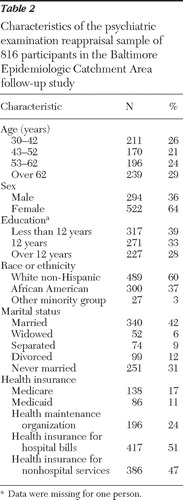 |
Population prevalence of need for any mental health services, based on sample weights, was determined to be 28.7%±2.7%, and the sample prevalence of need was 35.8 %±1.7%. As predicted, the weights corrected for oversampling of persons with a mental disorder, and the weighted prevalence was lower than the sample prevalence. Among the disorders studied, alcohol dependence presented the highest amount of need in the population, 13.6%±1.9%. This finding amounts to 90% of the sample with alcohol dependence (13.59 of 15.06). This was followed by 73% of those with major depression, or 10.5%±2.1% of the general population. For the remaining disorders in the general population, social phobia was prevalent in 5.2%±.9%, panic disorder in 5.2%±1.6%, and agoraphobia in 3.2%±.9%.
The treatment modality most needed for alcohol dependence was self-help groups, such as Alcoholics Anonymous, which were needed by 7.8%±1.6% of the population. Excluding psychiatrists' evaluations, we found that the highest treatment need for depression was psychotherapy, needed by 7.6%±1.8%, followed closely by 7.1%±1.7% needing antidepressant medication. Besides an evaluation by a psychiatrist, we found that the highest need for social phobia and agoraphobia treatment was behavioral modification interventions and antidepressant medication for panic disorder. Table 3 presents both the sample prevalence and the weighted estimates for each modality of treatment need by disorder.
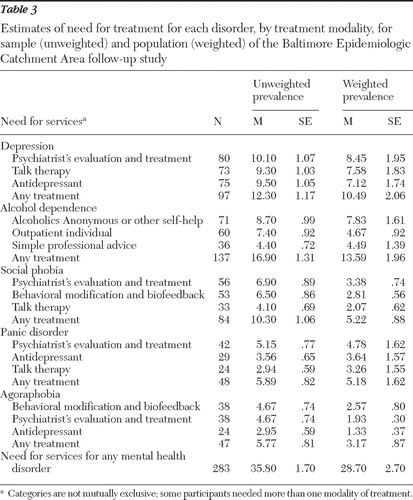 |
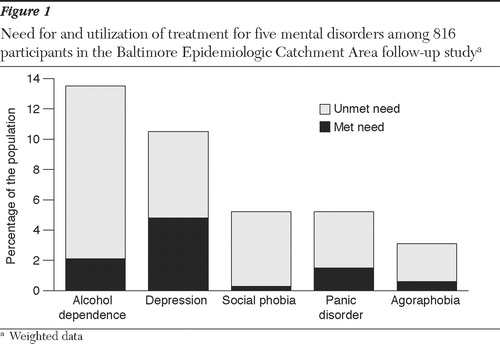
The level of treatment needs being met by service utilization varied across disorders ( Figure 1 ). Depression had the highest level of met need (46.7%), followed by panic disorder (29.3%). Social phobia was the disorder with the lowest proportion of met needs (7.9%) followed by alcohol dependence (15.4%). Overall, only 29.3% of the need for treatment for these five prevalent mental disorders was being met in the community.
Discussion and conclusions
This is the only study in the literature in which need for treatment has been directly estimated by psychiatrists in a general population sample. We determined that 28.7% of the population was in need of some modality of mental health services for five common mental disorders. The estimates of need for treatment were similar, but not identical, to the estimates of lifetime prevalence for the disorder. Less than a third of the estimated need for treatment was met.
These results should be examined in the context of the two large psychiatric epidemiologic studies: the five-site ECA study and the NCS. These studies have been criticized for providing discordant prevalence estimates and for not considering the issues of medical necessity or clinical significance ( 2 ). Our estimates of the prevalence of need fell between those from these two large studies, and our need-for-treatment estimates are closer to the prevalence estimates than we expected. According to our results, prevalence data approximated treatment needs for alcohol dependence and agoraphobia, they were a fair proxy for depression and social phobia, and they underestimated the need for treatment of panic disorder. Given this pattern, the relationship between prevalence and treatment needs varied across disorders, and prevalence data could be used with caution to approximate treatment needs in a population.
This study needs to be interpreted with the following limitations. First, this is not a cost-benefit analysis about mental health services. The data as such do not allow consideration of the cost associated with providing care. Second, although there is a growing concern about the undertreatment of mental disorders ( 10 ), we were not able to assess the issue of adequate care, and the fact that we classified any use of services as met need led to a conservative estimate of the percentage of needs met. Third, the data were collected some time ago, during the mid- and late 1990s; however, no major change in treatment options has appeared since then—selective serotonin reuptake inhibitors (SSRIs) had been introduced in the early 1990s. Fourth, the procedure to assess needs was based on psychiatrists' ascertainment after their receipt of detailed information; thus it is possible that the measure is too sensitive and could lead to overestimation of needs.
The Camberwell Needs for Care Survey applied a similar approach to measure the need for treatment in the general population ( 11 ). In that study 10% of the population was identified as having a need for the treatment of a psychiatric condition. This result differs from ours possibly in that Bebbington and colleagues used a scale to assess need, whereas we used a direct assessment by a clinician. The Camberwell survey also found that less than half of all needs were met ( 11 ). A study on the original Baltimore ECA sample estimated that 14% of the population met criteria for need for mental health services ( 12 ); however, that study again used a proxy measure of need that is likely less sensitive to more subtle need when compared with clinicians' direct assessment. That study also reported that only half of the need was met ( 10 ). The higher estimates of met needs in both of these surveys, compared with our finding that only around 30% of need was met, are compatible with the hypothesis that these measures are more appropriate for a more severe level of need.
Why do people not seek mental health services? Studies point to beliefs such as perceived lack of efficacy of treatment, thoughts that the problem will go away by itself eventually, the feeling that the problem can be handled without outside help, and the belief that anyone should be able to cope with these difficulties ( 13 , 14 ). Furthermore, external factors ( 15 ), such as societal pressures, stigma, and lack of comprehensive insurance coverage for mental health, are likely to play a role in the large amount of unmet need found in the population ( 16 , 17 , 18 , 19 ).
Whatever factor is keeping people from seeking mental health services, these estimates confirm that there is a substantial need for mental health services in the general population and that most individuals who would benefit from treatment are not receiving any type of mental health services.
Acknowledgments and disclosures
This research was supported by grants MH-47447, MH-50616, and K23-MH-64543 from the National Institute of Mental Health.
The authors report no competing interests.
1. Demyttenaere K, Bruffaerts R, Posada-Villa J, et al: Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 291:2581–2590, 2004Google Scholar
2. Narrow WE, Rae DS, Robins LN, et al: Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys' estimates. Archives of General Psychiatry 59:115–123, 2002Google Scholar
3. Bebbington PE, Brugha TS, Meltzer H, et al: Neurotic disorders and the receipt of psychiatric treatment. Psychological Medicine 30:1369–1376, 2000Google Scholar
4. Robins LN, Helzer JE, Croughan J, et al: National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Archives of General Psychiatry 38:381–389, 1981Google Scholar
5. Folstein MF, Romanoski AJ, Nestadt G, et al: Brief report on the clinical reappraisal of the Diagnostic Interview Schedule carried out at the Johns Hopkins site of the Epidemiological Catchment Area Program of the NIMH. Psychological Medicine 15:809–814, 1985Google Scholar
6. Wing JK, Babor T, Brugha T, et al: SCAN: Schedules for Clinical Assessment in Neuropsychiatry. Archives of General Psychiatry 47:589–593, 1990Google Scholar
7. Eaton WW, Anthony JC, Romanoski A, et al: Onset and recovery from panic disorder in the Baltimore Epidemiologic Catchment Area follow-up. British Journal of Psychiatry 173:501–507, 1998Google Scholar
8. Stata, version 8. College Station, Tex, Stata Corp, 2000Google Scholar
9. Samuels J, Eaton WW, Bienvenu OJ III, et al: Prevalence and correlates of personality disorders in a community sample. British Journal of Psychiatry 180:536–542, 2002Google Scholar
10. Hirschfeld RM, Keller MB, Panico S, et al: The National Depressive and Manic-Depressive Association Consensus Statement on the Undertreatment of Depression. JAMA 277:333–340, 1997Google Scholar
11. Bebbington PE, Marsden L, Brewin CR: The need for psychiatric treatment in the general population: the Camberwell Needs for Care Survey. Psychological Medicine 27:821–834, 1997Google Scholar
12. Shapiro S, Skinner EA, Kramer M, et al: Measuring need for mental health services in a general population. Medical Care 23:1033–1043, 1985Google Scholar
13. Wells JE, Robins LN, Bushnell JA, et al: Perceived barriers to care in St Louis (USA) and Christchurch (NZ): reasons for not seeking professional help for psychological distress. Social Psychiatry and Psychiatric Epidemiology 29:155–164, 1994Google Scholar
14. Kessler RC: Psychiatric epidemiology: selected recent advances and future directions. Bulletin of the World Health Organization 78:464–474, 2000Google Scholar
15. Badawi M, Kramer M, Eaton W: Use of mental health services by households in the United States. Psychiatric Services 47:376–380, 1996Google Scholar
16. Weisner C, Matzger H, Tam T, et al: Who goes to alcohol and drug treatment? Understanding utilization within the context of insurance. Journal of Studies on Alcohol 63:673–682, 2002Google Scholar
17. Kessler RC, Frank RG, Edlund M, et al: Differences in the use of psychiatric outpatient services between the United States and Ontario. New England Journal of Medicine 336:551–557, 1997Google Scholar
18. Cooper-Patrick L, Gallo JJ, Powe NR, et al: Mental health service utilization by African Americans and Whites: the Baltimore Epidemiologic Catchment Area Follow-Up. Medical Care 37:1034–1045, 1999Google Scholar
19. Andrews G, Henderson S, Hall W: Prevalence, comorbidity, disability and service utilization: overview of the Australian National Mental Health Survey. British Journal of Psychiatry 178:145–153, 2001Google Scholar



