Rural and Urban Disparities in Health-Related Quality of Life Among Veterans With Psychiatric Disorders
The Veterans Health Administration (VHA) provides comprehensive mental health services to veterans across the United States through regional delivery networks. Because of its relatively small service population and limited financial resources, many VHA services have been regionalized to reduce administrative costs. Specialty mental health services may be available only in urban referral centers, and access to even routine mental health services may be limited to parent Veterans Affairs (VA) facilities. Travel distances for rural veterans who are remote from referral centers or parent facilities may implicitly restrict veterans' access to mental health services, and restricted access may result in under-utilization of services ( 1 , 2 , 3 ). Because the veteran population experiences a particularly high incidence of mental illness ( 4 ), providing adequate mental health care to rural veterans is especially challenging and important.
We previously demonstrated that rural veterans have lower health-related quality of life than their urban counterparts; these differences in health-related scores were substantial, likely to be clinically significant and to be associated with increased costs of care, and pervasive over a majority of VA's regional service networks ( 5 ). However, rural-urban differences in disease incidence were potential explanations for the differences that we found. Therefore, to further explore rural-urban disparities, we used ICD-9-CM codes to identify veterans with six psychiatric disorders, and we compared health-related quality-of-life scores for rural and urban veterans within these diagnostic categories.
Methods
We conducted a cross-sectional study of health-related quality-of-life scores using the 1999 Large Health Survey of Veteran Enrollees ( 6 ). That survey used a modification of the Medical Outcomes Study 36-item Short Form Health Survey ( 7 ) called the Veterans SF-36. The Veterans SF-36 includes a multi-item scale that assesses health limitations in eight domains: physical activities because of health problems; social activities because of physical or emotional problems; usual role activities because of physical health problems; bodily pain; general mental health—psychological distress and well-being; limitations in usual role activities because of emotional problems; vitality—energy and fatigue; and general health perceptions ( 8 ). The Veterans SF-36 has been widely used, disseminated, and documented as reliable and valid in the VHA ( 9 ).
In late 1999 the survey was administered to a random sample of 1.4 million veteran enrollees who had used VHA services within the prior three years or who had enrolled in VHA in anticipation of using services in the future. Of those, 877,775 responded to the survey and 805,422 responded with usable Veterans SF-36 data. Of these, 136,177 had been diagnosed with one or more of the six common psychiatric disorders of interest—depression, anxiety disorder excluding posttraumatic stress disorder (PTSD), PTSD, alcohol dependence, schizophrenia, and bipolar disorder. From the Veterans SF-36 responses of those with psychiatric diagnoses, we calculated physical (PCS) and mental health (MCS) component summary scores.
For PCS and MCS scores, we used a t score transformation for summary scores and normalized them with a mean of 50 and a standard deviation of 10 in a general U.S. population. Lower scores denote worse health for the summaries, and differences in Veterans SF-36 scores of 2.5 points have been associated with increased morbidity ( 10 ). For example, with the analysis controlling for other diagnoses, depression is associated with an 8-point lower MCS score, and alcohol disorders are associated with a 6.6-point lower score. Lower scores also have been associated with increased resource consumption. For veterans, a 1-point decrease in PCS is associated with an annual $148.20, or 3.2 percent, increased cost of care over the average cost of $4,632 per patient. A 1-point decrease in MCS is associated with an independent annual $86.40, or 1.9 percent, increase in costs of care per patient when age, gender, and ICD-9-CM -defined comorbid disorders are controlled for ( 11 , 12 ). Therefore, population differences in Veterans SF-36 scores can be used to anticipate population differences in morbidity, health care needs, and anticipated health care expenditures.
The survey also collected Social Security number, self-reported demographic data (age, gender, race, maximum educational attainment, and employment status), and zip code of residence. We linked respondents' Social Security numbers to VHA databases to determine diagnostic cohorts, dates of death, and VHA priority level.
Diagnostic cohorts for comparison purposes
We used ICD-9-CM codes recorded in outpatient or inpatient treatment for the three years before the survey to categorize veterans into six psychiatric diagnostic categories ( 13 ). We also used ICD-9-CM codes to calculate comorbidity indices. Mental and physical health comorbidity indices were calculated as the sum of ICD-9 codes for six mental health and 30 medical diagnoses recorded in outpatient or inpatient treatment for the three years before the survey. The indices range from 0 to 6 for mental health and from 0 to 30 for physical health, and they were previously validated ( 13 ). For example, a patient who had ICD-9 codes for two mental health and four physical health conditions would have a mental health comorbidity index of 2 and a physical health comorbidity index of 4.
Date of death
The VA's Beneficiary Identification and Records Locator Subsystem is a centralized data set that stores veterans' dates of death. We linked our data to this data set to identify veterans who died between 1999 and 2003.
Veterans' priority levels
Priority levels range from 1 to 7 (although there are now eight priority levels, at the time of the survey there were seven), are specific to an individual veteran, and are associated with severity of service-related disabilities, special status, and income level. Veterans with priority levels 1 through 6 tend to be more disabled, poorer, and more reliant on VHA for health care services and to have lower mean MCS and PCS scores than veterans with a priority level of 7 ( 9 ). Because priority level could confound observed differences in rural-to-urban comparisons, we included priority levels in our regression model.
We used zip code of residence to calculate two variables, residential area and census region.
Rural or urban residence
To identify veterans as living in a rural or an urban setting, we used Rural-Urban Commuting Area (RUCA) codes developed by the Health Resources and Services Administration's Federal Office of Rural Health Policy, the Department of Agriculture's Economic Research Service, and the WWAMI Rural Health Research Center at the University of Washington School of Medicine ( 14 ). We used the Washington State Department of Health's RUCA consolidation system ( 15 ) to classify and compare urban veterans (those in areas of 50,000 persons or more, corresponding to U.S. Bureau of the Census's defined urbanized areas; RUCA code 1.0) with rural veterans (those in small towns and isolated rural areas that consist of towns with populations below 10,000, their commuter sheds, and other isolated rural areas; RUCA codes 7.0, 7.3, 7.4, 8.0, 8.3, 8.4, 9.0, 9.1, 9.2, 10.0, 10.3, 10.4, and 10.5).
Census region
To correct for regional variation across the United States, we used zip code data in our regression analyses to determine the major U.S. census region—northeast, south, midwest, and west—in which each veteran respondent resided. Because census region could confound observed differences in rural-to-urban comparisons, we included census region in our regression model.
Zip code data were not available for 38,313 veterans, or 4.4 percent of respondents. In addition, zip code data did not match RUCA codes for 18,893 veterans, or 2.2 percent of respondents, leaving a total of 748,216 respondents for analysis. Of these, 148,989 lived in rural settings, 421,523 lived in urban settings, and 177,704 lived in suburban settings. Because we were interested in comparing rural with urban veterans, we limited our analysis to only rural and urban groups, of which 128,352 respondents had been diagnosed with one or more of the six psychiatric disorders of interest.
Statistical analysis
We calculated the incidences of six common psychiatric disorders in the rural and urban veteran population and compared them by using odds ratios. Within each psychiatric diagnostic category, we compared unadjusted mean PCS and MCS scores using analysis of variance. We conducted multivariate analysis using ordinary least-squares regression to examine the association of rural-urban status with the Veterans SF-36 with controls for age, gender, VA priority status, comorbidity indices, and U.S. census region. Multivariate analysis was limited to the 128,352 respondents from urban or rural residence settings with one or more of the six psychiatric diagnoses.
Results
All psychiatric disorders except non-PTSD anxiety disorders were more prevalent in urban than rural settings; differences were statistically significant for all diagnoses except non-PTSD anxiety disorders ( Table 1 ). However, across all mental disorders examined, veterans who lived in rural settings had lower PCS and MCS scores, denoting worse physical and mental health-related quality of life. Differences in PCS scores ( Figure 1 ) were substantial, ranging between 2.27 for schizophrenia and 3.39 for alcohol dependence (p<.001 for all categories). These differences were associated with expected additional annual health care costs of between $336 (or a 7.3 percent increase over the average annual cost) and $502 (or a 10.9 percent increase over the average annual cost) per veteran.
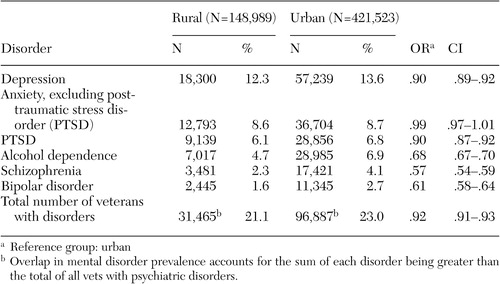 |
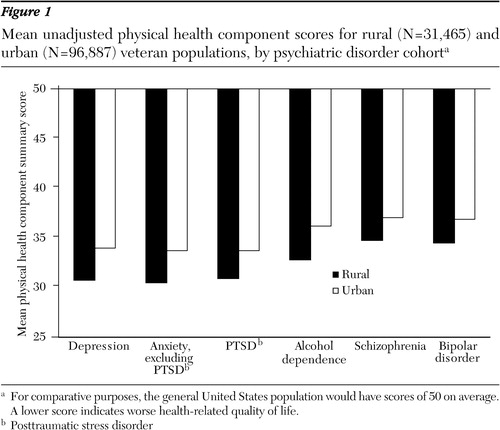
a For comparative purposes, the general United States population would have scores of 50 on average. A lower score indicates worse health-related quality of life.
Differences in MCS scores ( Figure 2 ) were modest, ranging between .74 for schizophrenia and 1.96 for PTSD (p<.005 for all diagnoses). The differences that we found would be associated with anticipated increased annual costs per veteran of between $64 and $169 (1.4 to 3.7 percent greater costs).
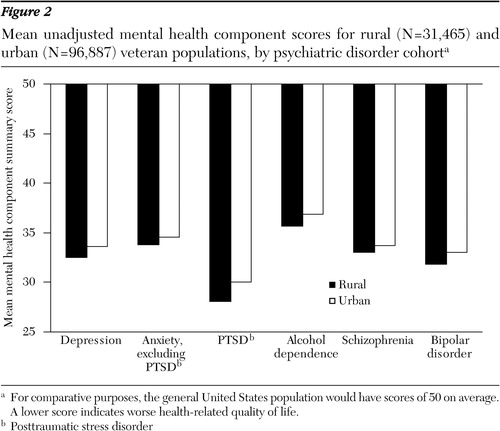
a For comparative purposes, the general United States population would have scores of 50 on average. A lower score indicates worse health-related quality of life.
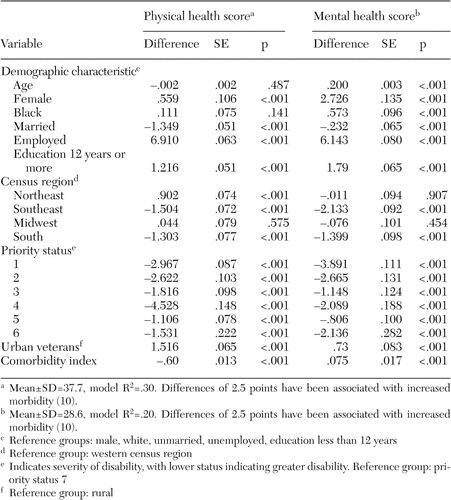
Rural-urban quality-of-life disparities found in unadjusted data persisted after the multivariate analysis controlled for other factors ( Table 2 ). The mean adjusted PCS score for all psychiatrically diagnosed respondents was 37.7, or 1.3 standard deviations lower than U.S. age-adjusted norms; the mean MCS score was 28.6, or 2.4 standard deviations lower than U.S. age-adjusted norms. Veterans who were male, unemployed, lived in the southern or southeastern U.S. census region, and who had fewer than 12 years of education had lower PCS and MCS scores. In comparison with priority 7 status, all other priority levels were associated with lower PCS and MCS scores. Finally, after the analysis corrected for other variables, rural status was associated with a 1.5-point lower PCS score and a .7-point lower MCS score. These variables explained 30 percent of the variance of the physical health component scores and 20 percent of the variance seen in mental health component scores.
 |
Discussion
We found that although the incidence of six major psychiatric disorders was lower among rural veterans, rural veterans with these disorders had greater disease burden, as demonstrated by lower health-related quality-of-life scores, when compared with their urban counterparts. For PCS summary scores, the differences were substantial; for MCS summary scores, the relationship, although present, was less dramatic. These rural-urban disparities persisted after the analysis corrected for age, gender, employment status, priority level, comorbidity, and the U.S. census region in which the veteran lived.
For rural mental health care providers, these findings offer supportive evidence that living in a rural setting is associated with greater impairment, as defined by poorer quality of life. Various factors contributed to the rural-urban disparities that we found. Although primary care at rural VA centers has been shown to be of equal or better quality than that in urban settings ( 16 ), it is possible that quality of mental health care in rural areas may be different from that in urban areas. Alternatively, the differences that we found may be mediated through rural veterans' limited access to care. Others have found that the quality of mental health care, as defined by treatment concordant with clinical guidelines, was compromised for patients with depression in rural areas who had fewer visits because of greater distance to care ( 17 ). Likewise, clinical outcomes, as defined by suicide attempt and hospitalization rates, were worse among patients with depression from rural settings compared with urban patients, at least in part because the former group was able to access fewer specialty mental health services ( 18 ). We have also demonstrated that rural veterans used fewer VHA and Medicare services than their urban counterparts ( 19 ). It seems likely that restricted access to mental health care in rural settings may be a mediating factor for poorer quality of life among veterans with psychiatric disorders.
The smaller rural-urban differences in quality-of-life scores for mental health versus physical health also are not surprising. Others have found that strong social supports serve as positive, moderating factors against depression ( 20 , 21 , 22 , 23 ) and that rural residents are more likely to have and seek social supports ( 24 , 25 ). The social and emotional advantages of rural living may not be similarly translated into physical quality-of-life advantages. Specifically, in rural areas the lack of municipal services, including public transportation and municipal recreational resources, may worsen the physical health of rural residents compared with urban residents, independent of an individual's socioeconomic status ( 26 , 27 , 28 ). However, in our cross-sectional analysis, it was impossible to determine whether those with lower health-related quality of life congregate in more rural settings or whether rural living results in lower health-related quality of life.
Implications
Our findings have important implications for the mental health resource needs of veterans in rural areas. Others have demonstrated that lower health-related quality-of-life scores are associated with greater health care service needs in the general population ( 29 ). The differences that we found suggest that rural veterans with psychiatric diagnoses will generate health care costs from 2 to 4 percent higher than their urban counterparts on the basis of MCS scores and from 7 to 11 percent higher on the basis of PCS scores. The combination of lower scores, greater anticipated service needs, and higher anticipated costs suggests that policy makers should be cautious when comparing costs and utilization of care for those with mental disorders across rural and urban settings.
Increasing the number of mental health care access points may help meet mental health care needs. Within VHA, this balance could be achieved in several ways. First, VHA could dedicate more resources to rural mental health care delivery—through development of additional programs in rural VHA medical centers, augmented reimbursement for rural delivery systems, broader use of distance technology, or collaboration with the community to enhance non-health care issues that might contribute to worse quality of life. VHA has invested heavily in distance technology to improve access to mental health services for rural veterans. Tele-mental health care delivery already takes place at 228 sites, including 120 community-based outpatient clinics ( 30 ). Since the survey, VHA has also markedly increased the number of primary care access points for all veterans, including those in rural settings, through the establishment of outpatient clinics. Recently, VHA mandated that 10 percent of the workload in outpatient clinics be dedicated to mental health care.
Indeed, linking mental health and primary care within the same clinics has proven successful in other settings ( 31 ). However, mental health providers experience disincentives to rural practice as well, including professional isolation and limited access to supervision ( 32 ). Enticing rural mental health clinicians, who are already in high demand ( 33 ), to practice in these clinics may be challenging. In addition, VHA might consider the development of a coordinated federal or state health care benefit for veterans who live in rural settings. Veterans are likely to be enrolled in Medicare ( 34 ). A coordinated federal benefits package for rural veterans could take advantage of existing non-VHA infrastructure in rural settings, thereby improving access to care without expanding infrastructure, at least for older veterans with mental health disorders or veterans whose disabilities qualify them for Medicare. In addition, many chronically mentally ill veterans may qualify for community mental health services through state Medicaid programs. Finally, VHA might partner independently with community mental health centers to provide psychiatric services for rural veterans through outsourcing or space- or staff-sharing agreements.
Limitations
Our study has several limitations. First, it used a cross-sectional database that was limited to self-report of functional status, and the survey was conducted seven years ago, in 1999. Therefore, we were not able to examine trends over time. Although the sample was very large and the differences were important, the VA health care delivery system has changed over the past several years. Therefore, studies using more recent, longitudinal cohort data are needed to determine whether our findings persist. Second, our study stratified results by rural setting as defined by RUCA codes. The study compared neither the quality of VHA care in rural and urban settings nor the relationship between access to that care and health-related quality of life. Additional studies are required to address whether rural veterans' health-related quality-of-life scores might be enhanced by access to care.
Third, we were not able to examine environmental, economic, or social factors that may contribute to lower health-related quality-of-life scores that we found in rural settings. For instance, the differences that we found may be facilitated by restricted access to care in rural settings. It is possible that, because of the long distance to care for many veterans in rural settings, only those with the greatest health care needs were enrolled in the VHA system and were therefore part of the survey. Fourth, our study was limited to veterans—a population likely to be older, poorer, and sicker than the general population. Because of the paucity of women and absence of children in our data set, generalization of our findings to the entire U.S. population may be limited. Finally, our study may underestimate differences between rural and urban veterans; the "floor effect" ( 35 ) that exists at the low score levels that we saw may mitigate the true differences that exist.
Conclusions
Despite these limitations, the findings shed light on health care-related quality of life in the rural population, highlight potential disparities in health care needs, and underscore challenges of mental health care delivery to rural populations. These results strongly suggest that administrators should anticipate greater health care demands from the mentally ill rural veteran population and pursue innovative strategies, including coordination of federal health benefits, to meet their physical and mental health care needs.
Acknowledgments
The research reported here was supported by the Veterans' Rural Health Initiative and by grant REA 03-098 from the Department of Veterans Affairs, Veterans Health Administration (VHA), Health Services Research and Development Service. The authors thank VHA's Office of Quality and Performance for providing the data for analysis. Dr. Wallace was supported by a VA Health Services Research and Development Advanced Career Development Award.
1. Rosenheck R, Stolar M: Access to public mental health services: determinants of population coverage. Medical Care 36:503-512, 1998Google Scholar
2. McCarthy JF, Blow FC: Older patients with serious mental illness: sensitivity to distance barriers for outpatient care. Medical Care 42:1073-1080, 2004Google Scholar
3. Tessler R, Rosenheck R, Gamache G: Declining access to alcohol and drug abuse services among veterans in the general population. Military Medicine 170:234-238, 2005Google Scholar
4. Wilson NJ, Kizer KW: The VA health care system: an unrecognized national safety net. Health Affairs 16(4):200-204, 1997Google Scholar
5. Weeks WB, Kazis LE, Shen Y, et al: Differences in health-related quality of life in rural and urban veterans. American Journal of Public Health 94:1762-1767, 2004Google Scholar
6. Kazis L, Ren X, Skinner K, et al: Initial Results From the 1999 Large Health Survey of Veteran Enrollees. Presented at VA Health Services Research and Development, Washington, DC, Feb 14-16, 2001Google Scholar
7. Ware J, Bayliss M, Rogers W, et al: Differences in 4-year health outcomes for elderly and poor, chronically ill patients treated in HMO and fee-for-service systems. JAMA 176:1039-1047, 1996Google Scholar
8. Ware JE Jr, Sherbourne CD: The MOS 36-item short form health survey (SF-36): conceptual framework and item selection. Medical Care 30:473-483, 1992Google Scholar
9. Perlin J, Kazis L, Skinner K, et al: Health Status and Outcomes of Veterans: Physical and Mental Component Summary Scores, Veterans SF-36, 1999 Large Health Survey of Veteran Enrollees. Washington, DC, Veterans Health Administration Office of Quality and Performance, 2000Google Scholar
10. Kazis L, Ren X, Lee A, et al: Health status in VA patients: results from the veterans' health study. American Journal of Medical Quality 14:28-37, 1999Google Scholar
11. Kazis L, Skinner K, Rogers W, et al: Health Status of Veterans: Physical and Mental Component Summary Scores (SF-36V): 1998 National Survey of Ambulatory Care Patients Mid-Year Executive Report. Washington, DC, Veterans Health Administration Office of Quality and Performance, 1998Google Scholar
12. 1998 Cost Data. Austin, Tex, Department of Veterans Affairs Allocation Resource Center, 1998Google Scholar
13. Selim A, Fincke G, Ren X, et al: The Comorbidity Index in Measuring and Managing Health Care Quality. Gaithersburg, Md, Aspen Publishers, 2002Google Scholar
14. Rural Urban Commuting Area Code, vol 2004. Washington, DC, US Department of Agriculture Economic Research Service, 2001Google Scholar
15. ZIP Code RUCA Approximation Methodology, vol 2004. Seattle, Wash, WWAMI Rural Health Research Center, 2004Google Scholar
16. Weeks WB, Yano EM, Rubenstein LV: Primary care practice management in rural and urban Veterans Health Administration settings. Journal of Rural Health 18:298-303, 2002Google Scholar
17. Fortney J, Rost K, Zhang M, et al: The impact of geographic accessibility on the intensity and quality of depression treatment. Medical Care 37:884-893, 1999Google Scholar
18. Rost K, Zhang M, Fortney J, et al: Rural-urban differences in depression treatment and suicidality. Medical Care 36:1098-1107, 1998Google Scholar
19. Weeks WB, Bott DM, Lamkin RP, et al: Veterans Health Administration and Medicare outpatient health care utilization by older rural and urban New England veterans. Journal of Rural Health 21:165-171, 2005Google Scholar
20. Newsom JT, Schulz R: Social support as a mediator in the relation between functional status and quality of life in older adults. Psychology and Aging 11:34-44, 1996Google Scholar
21. Oxman TE, Berkman LF, Kasl S, et al: Social support and depressive symptoms in the elderly. American Journal of Epidemiology 135:356-368, 1992Google Scholar
22. Schaefer C, Coyne JC, Lazarus RS: The health-related functions of social support. Journal of Behavioral Medicine 4:381-406, 1981Google Scholar
23. Pinquart M, Sorenson S: Influences of socioeconomic status, social network, and competence on subjective well-being in later life: a meta-analysis. Psychology and Aging 15:187-224, 2000Google Scholar
24. Romans SE, Walton VA, Herbison GP, et al: Social networks and psychiatric morbidity in New Zealand women. Australian and New Zealand Journal of Psychiatry 26:485-492, 1992Google Scholar
25. Farmer JE, Clark MJ, Sherman AK: Rural versus urban social support seeking as a moderating variable in traumatic brain injury outcome. Journal of Head Trauma Rehabilitation 18:116-117, 2003Google Scholar
26. Pickett KE, Pearl M: Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. Journal of Epidemiology and Community Health 55:111-122, 2001Google Scholar
27. Thomson H, Kearns A, Petticrew M: Assessing the health impact of local amenities: a qualitative study of contrasting experiences of local swimming pool and leisure provision in two areas of Glasgow. Journal of Epidemiology and Community Health 57:663-667, 2003Google Scholar
28. Cubbin C, Hadden WC, Winkleby MA: Neighborhood context and cardiovascular disease risk factors: the contribution of material deprivation. Ethnicity and Disease 11:687-700, 2001Google Scholar
29. Parkerson G, Broadhead W, Tse C: Health status and severity of illness as predictors of outcomes in primary care. Medical Care 33:53-66, 1995Google Scholar
30. Department of Veterans Affairs Office of Care Coordination: VHA Telemental Health. Available at www.va.gov/occ/telemental/telementalhealth.asp. Accessed Sept 21, 2005Google Scholar
31. Lambert D, Hartley D: Linking primary care and rural psychiatry: where have we been and where are we going? Psychiatric Services 49:965-967, 1998Google Scholar
32. Roberts LW, Battaglia J, Epstein RS: Frontier ethics: mental health care needs and ethical dilemmas in rural communities. Psychiatric Services 50:497-503, 1999Google Scholar
33. Merwin E, Hinton I, Dembling B, et al: Shortages of rural mental health professionals. Archives of Psychiatric Nursing 17:42-51, 2003Google Scholar
34. Wright S, Petersen L, Lamkin R, et al: Increasing use of Medicare services by veterans with acute myocardial infarction. Medical Care 37:529-537, 1999Google Scholar
35. Bindman AB, Keane D, Lurie N: Measuring health changes among severely ill patients. The floor phenomenon. Medical Care 28:1142-1152, 1990Google Scholar



