Mental Distress Among Younger Veterans Before, During, and After the Invasion of Iraq
Abstract
OBJECTIVE: The purpose of this study was to determine whether patients receiving care from the Department of Veterans Affairs (VA) reported more mental distress as the war in Iraq began or reintensified compared with other respondents to national health surveys. METHODS: Data from the 2000 and 2003 Behavioral Risk Factor Surveillance System (BRFSS) health surveys were analyzed. Unlike in other years, these particular surveys asked respondents whether they were military veterans. As in other years' surveys, these surveys also asked whether respondents used VA medical care. Male respondents were stratified by age and separated into three groups: VA patients, other veterans, and nonveterans. The proportions of respondents who reported five or more recent days of poor mental or physical health were analyzed with chi square tests. RESULTS: Although the number of recent days of poor mental health among nonveterans, other veterans, and older VA patients were stable from 2000 to 2003, younger VA patients in 2003 reported substantially more days of poor mental health in two intervals: during the Iraq war buildup and invasion, and later, when resistance on the ground reintensified. Comparable changes in physical health complaints were not observed. CONCLUSIONS: In times of war, the VA may anticipate more mental health problems among its current patients, particularly younger veterans.
American military personnel who are now returning from combat operations in Iraq and Afghanistan have elevated rates of posttraumatic stress disorder (PTSD), generalized anxiety, major depression, and misuse of alcohol, and an association has been demonstrated between rates of these disorders and the extent of combat exposure (1). As these veterans leave military service, the Department of Veterans Affairs (VA) can anticipate increased demand for mental health care from a significantly younger group than most of its current clientele. Clinical experience also suggests that current war-related events might increase anxiety and mental distress among veterans who have already left military service.
In 2000, younger male VA patients who participated in a national health survey of the general adult population reported a substantially greater number of recent days of mental distress than older VA patients, veterans who were not currently receiving VA care, and nonveterans (2). That survey—the Centers for Disease Control and Prevention's (CDC's) Behavioral Risk Factor Surveillance System (BRFSS) health survey for 2000—included specific questions that elicited estimates of recent days of anxiety, depressed mood, and debilitating fatigue or pain. VA patients between the ages of 18 and 44 years, particularly those living in nonmetropolitan areas, reported more problem days on all these measures than did other respondents. These findings are consistent with previous reports (3) that younger VA patients experience particularly high levels of mental health problems.
Terrorist and military events since 2000 have raised anxiety for many Americans. However, news of combat in the Middle East may increase mental distress most among those who are emotionally predisposed, such as younger VA patients. Given that 33 percent of VA patients who were between 18 and 44 years of age in 2003 had served in Operation Desert Storm, and because the rates of PTSD and other mental health problems tend to be high among Gulf War veterans who receive VA medical care (4), we expected these younger VA patients to be particularly reactive to news of renewed conflict in that region. By comparing BRFSS data from 2000 and 2003, we tested whether Americans reported more mental distress after September 11, 2001, and the onset of combat in the Middle East; whether the difference was greater for VA patients than for nonveterans or veterans who were not receiving VA care; and whether it was greatest for younger patients who had served more recently, many in the same combat theater.
Methods
Survey and sample
Each year the CDC collaborates with all state health departments to administer the BRFSS survey nationwide, by telephone, to large probability samples of adults. Although the BRFSS has many optional questions that only some states administer, its core includes questions asked of all interviewees about current health status, behavioral health risks, insurance coverage, and access to medical care. Some questions change from year to year, but several remain constant, which allows comparisons across years of independent samples of respondents. Deidentified individual response data are available for public download at the BRFSS Web site (www.cdc.gov/brfss/index.htm).
The BRFSS routinely asks whether respondents received health care services from VA facilities during the past year. Unlike other years, in 2000 and 2003 the BRFSS also asked whether the respondents were military veterans. This additional information allowed us to compare VA patients, veterans who were not receiving VA care, and nonveterans in the samples for these years. Within each group we stratified respondents into three age categories: 18 to 44 years, 45 to 64 years, and 65 years or older. Because few female respondents were veterans (about 1 percent), we limited our analyses to males. The 2000 BRFSS included 71,620 males who could be categorized by age and by veteran and VA-patient status. There were 49,701 nonveterans (31,796 aged 18 to 44 years, 14,179 aged 45 to 64 years, and 3,726 aged 65 years or older), 18,796 veterans who were not receiving VA care (3,673 aged 18 to 44 years, 8,560 aged 45 to 64 years, and 6,563 aged 65 years or older), and 3,123 VA patients (447 aged 18 to 44 years, 1,250 aged 45 to 64 years, and 1,426 aged 65 years or older).
The 2003 BRFSS included 98,559 males who could be categorized: 67,403 nonveterans (37,414 aged 18 to 44 years, 24,020 aged 45 to 64 years, and 5,969 aged 65 years or older), 25,238 veterans not under VA care (3,935 aged 18 to 44 years, 11,078 aged 45 to 64 years, and 10,225 aged 65 years or older), and 5,918 VA patients (482 aged 18 to 44 years, 2,286 aged 45 to 64 years, and 3,150 aged 65 years or older). In the 2000 sample, 84 percent of males were white (81 percent of those aged 18 to 44 years, 86 percent of those aged 45 to 64 years, and 89 percent of those aged 65 years or older). In the 2003 sample, 78 percent were white (73 percent of those aged 18 to 44 years, 81 percent of those aged 45 to 64 years, and 84 percent of those aged 65 years or older). Race distributions were comparable across groups.
Measures
Here we consider only two primary questions asked in the core BRFSS: Immediately after providing informed consent, study participants were asked, "Thinking now about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?" and "Thinking now about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?" Although our focus was on changes in mental distress from 2000 to 2003, we also examined physical distress as a control measure to assess for potential sampling or population response differences from one year to another.
Inspection of the data for each year indicated that for either variable, about two-thirds of respondents reported no problem days, whereas progressively smaller proportions reported one, two, or three days. However, for either variable in either year, at least 15 percent of respondents reported five or more problem days. We therefore defined respondents who gave an estimate of at least five days on a variable as high-distress patients for that measure.
Analyses
Proportions of respondents with high levels of distress were analyzed with chi square tests to assess differences between years, overall and within each group and age category. In a second set of analyses, we also split the data for each year according to the dates on which respondents were interviewed. We defined three periods—January through April, May through August, and September through December—which in 2003 corresponded roughly to the military buildup and invasion of Iraq, a relatively low-conflict period after the apparent end of combat, and the emergence of the insurgency with renewed conflict, respectively. Including part of the year as a factor enabled us to compare each period with the corresponding period in 2000 as a type of control. We hypothesized that the first period in 2003 might be particularly stressful for younger VA patients who were being exposed to news of the impending combat.
The BRFSS uses a complex stratified sampling design, with multiple primary sampling units in each state. A weighting variable is derived to correct for variations in sampling coverage and to estimate population values. To ensure proper variance estimates, we used SUDAAN software (www.rti.org/sudaan) for the analysis of complex survey designs. Proportions of high-distress respondents were analyzed with chi square tests, computed by using SUDAAN's Crosstab procedure, applying the BRFSS sampling design and weighting variable (weighted means were also computed with the Descript procedure). All significance tests were two-tailed. This work was approved by both our local VA research and development committee and by Dartmouth Medical School's committee for the protection of human subjects.
Results
The proportions of men who reported at least five days of poor mental health in the previous month, broken down by group, age category, and year, are shown in Figure 1. Generally, mental distress was greatest among younger men and among VA patients; Vietnam-era VA patients (aged 45 to 64 years) reported particularly high levels. From 2000 to 2003, the percentages in each combination of group and age were consistent, with one exception: VA patients aged 18 to 44 years evidenced a dramatic increase, from 17.5 percent in 2000, which was no higher than for other men their age, to 28.9 percent in 2003, the highest that year, higher than for the Vietnam-era VA patients (N=446,786 for all analyses, χ2=5.57, df=1, p<.05). For these younger men, the weighted average of poor mental health days increased from 3.6 in 2000 to 5.7 in 2003, the highest average for any combination of age and group in either year.
Across all men in the BRFSS samples, the proportion of respondents with high levels of mental distress increased modestly but significantly from 14.7 percent in 2000 to 16.0 percent in 2003 (χ2=16.33, df=1, p<.001), which represents a 9 percent increase. Among all men aged 18 to 44 years, the increase was from 17.7 to 19.1 percent (χ2=7.78, df=1, p<.01); among those aged 45 to 64 years, the increase was from 13.0 percent to 14.6 percent (χ2=9.97, df=1, p<.01); and among those aged 65 years or older, the increase was from 7.5 percent to 8.0 percent (difference not significant). When we broke down each age category by group, the year-to-year differences were less than 12 percent, with one exception: the 65 percent increase for VA patients aged 18 to 44 years reflects the fact that their levels of mental distress did not differ from those of other men in their age category in 2000 but were substantially higher in 2003.
Analyses of the proportions of men reporting at least five days of poor physical health had rather different results. The number of problem days was consistently greater among older men and among VA patients and was highest among Vietnam-era VA patients. The overall proportion increased from 14.8 percent in 2000 to 16.1 percent in 2003 (χ2=16.74, df=1, p<.001), which also represents a 9 percent increase. However, in this case no combination of age category by group showed any year-to-year changes outside a 13 percent range. Among all men aged 18 to 44 years, the increase was from 11.0 percent to 12.4 percent (χ2=11.06, df=1, p<.001); among those aged 45 to 64 years, the increase was from 17.4 percent to 18.8 percent (χ2=6.01, df=1, p<.05); and among those aged 65 years or older, the increase was from 23.2 percent to 23.6 percent (difference not significant). However, for VA patients aged 18 to 44 years, a marginal decline was noted, from 20.1 percent in 2000 to 19.5 percent in 2003, which suggests that the increase in mental distress levels in this group did not arise from a general propensity to report more problem days in 2003.
In a second set of analyses, we also separated respondents according to the part of the year in which they were interviewed (January to April, May to August, or September to December). These analyses tested whether reported distress was associated with different phases of Operation Iraqi Freedom in 2003 (during the buildup and invasion, immediately after President Bush announced that the war was over, and when the insurgency subsequently intensified), using the same intervals in 2000 for comparison.
Only one variable (mental health) and only one combination of group and age category (VA patients aged 18 to 44 years) showed substantial year-to-year differences in distress associated with particular parts of the year. The percentages of all men aged 18 to 44 years who reported high levels of mental distress are shown in Figure 2. Among VA patients aged 18 to 44 years who were interviewed between January and April, the proportion reporting high levels of mental distress was 21.1 percent in 2000 but 36.1 percent in 2003, representing a 72 percent increase, although the statistical significance of the difference was marginal (χ2=2.74, df=1, p<.10). The weighted average number of poor mental health days per month increased from 4.0 in 2000 to 7.1 in 2003. Among VA patients aged 18 to 44 years who were interviewed between September and December, the proportion reporting high levels of mental distress was 16.2 percent in 2000 but 32.1 percent in 2003, representing a 99 percent increase (χ2=4.35, df=1, p<.05). The weighted average number of poor mental health days increased from 3.4 in 2000 to 6.0 in 2003.
Although several other combinations of age category by group showed significant year-to-year changes for mental distress in certain periods—nonveterans aged 18 to 44 years who were interviewed between May and August evidenced an increase of 12 percent (p<.05), nonveterans aged 45 to 64 years who were interviewed between September and December evidenced an increase of 20 percent (p<.05), and nonveterans aged 65 years or older who were interviewed between September and December evidenced a decrease of 32 percent (p<.05)—no changes were of the same magnitude as those for the younger VA patients.
The few significant changes for physical distress were also not of the same magnitude: among nonveterans aged 18 to 44 years who were interviewed between September and December, 10.2 percent reported high levels of physical distress in 2000, and 12.7 percent reported high levels of physical distress in 2003 (p<.001). Among veterans aged 18 to 44 years who were not under VA care and who were interviewed between September and December, 8.8 percent had high levels of physical distress in 2000, and 13.2 percent had high levels of physical distress in 2003 (p<.05). Among veterans aged 65 years or older who were not under VA care and who were interviewed between May and August, 18.1 percent reported high levels of distress in 2000, and 22.1 percent reported high levels of distress in 2003 (p<.05). Although these changes were statistically significant, the levels of physical distress were far lower than the levels of mental distress reported by younger VA patients in 2003. In short, substantially higher proportions of 18- to 44-year-old VA patients who were interviewed during the military buildup and invasion of Iraq, or later as the insurgency emerged and American casualties increased, reported high numbers of days of poor mental health.
Discussion
Among male VA patients aged 18 to 44 years who participated in BRFSS surveys, those in the 2003 survey were substantially more likely than the 2000 respondents to report at least five days of poor mental health during the month before the interview. Older VA patients, other veterans who were not under VA care, and nonveterans were also compared across years, but there were no significant differences between these groups. Generally, older men were less likely to acknowledge as many problem days, which is consistent with much of the research on generational differences in reporting mental health concerns (5,6). Nevertheless, among men aged 45 years or older, VA patients were more likely than other groups to report days of mental health problems. In both years the Vietnam-era veterans who were receiving VA care were substantially more likely to report a high number of problem days. Thus it is noteworthy that younger VA patients did not differ from other men in their age category in 2000, but in 2003 the proportion who reported more mental health problem days exceeded the level for Vietnam-era patients.
That the proportion reporting high numbers of problem days did not also increase for Vietnam-era patients may indicate a sort of ceiling effect for this measure. Alternatively, this finding may suggest that news of the current conflict was more emotionally salient to younger veterans who had served in the same combat theater, which would be consistent with other studies indicating that perceived similarity to victims increases a remote observer's distress in response to news of traumatic events (7).
In 2003 younger VA patients experienced the greatest number of poor mental health days during the first and last thirds of the year. The first period involved the buildup and launching of Operation Iraqi Freedom, which was televised widely, perhaps inducing considerable anticipatory anxiety among these veterans (8). With the occupation of Iraq, hostilities subsided during the summer months. However, during the last third of the year, U.S. casualties increased between the suicide bombing of the Baghdad United Nations headquarters in late August and the capture of Saddam Hussein in December. The reality of a protracted war and its casualties may have first become apparent to the post-Vietnam veterans at that time.
The 2000 and 2003 BRFSS samples were selected independently, but we do not think our findings arise from sampling differences. Demographic characteristics of respondents were similar over time, and the number of recent days of poor physical health did not differ across years. Increased mental distress was unique to younger VA patients. Younger patients previously have been found to have high levels of mental health problems and so may have been particularly emotionally vulnerable to news of combat operations. Under the assumption that perhaps one-third of the younger VA patients in the BRFSS sample were involved in Operation Desert Storm a decade earlier, their increased mental distress in 2003 may reflect empathy for the struggles that the active military now faced in Iraq.
Conclusions
As the conflict in Iraq continues, the VA may anticipate more mental health problems among its current patients, particularly younger veterans. Policy makers estimating the costs of war should include these casualties in their projections.
Acknowledgments
Two Department of Veterans Affairs programs funded this research: The Veterans' Rural Health Initiative and the Research Enhancement Award Program (REAP; grant REA 03-098).
Dr. West is affiliated with the Department of Veterans Affairs (VA) Outcomes Group Research Enhancement Awards Program (REAP), VA Medical Center (11Q), White River Junction, Vermont 05009 (e-mail, [email protected]). Dr. Weeks is affiliated with the VA Outcomes Group REAP and the VA National Center for Patient Safety field office in White River Junction and with the department of psychiatry and community and family medicine of Dartmouth Medical School in Hanover, New Hampshire.
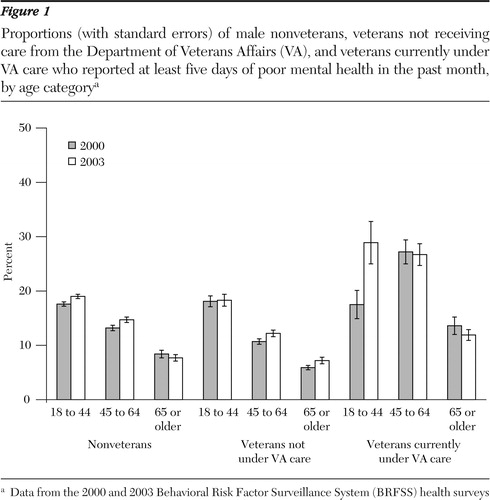
Figure 1. Proportions (with standard errors) of male nonveterans, veterans not receiving care from the Department of Veterans Affairs (VA), and veterans currently under VA care who reported at least five days of poor mental health in the past month, by age categorya
a Data from the 2000 and 2003 Behavioral Risk Factor Surveillance System (BRFSS) health surveys
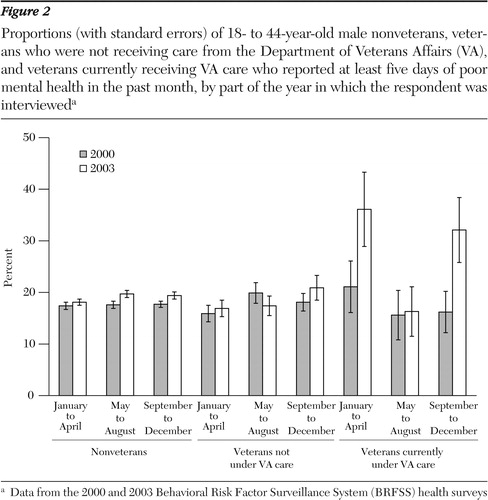
Figure 2. Proportions (with standard errors) of 18- to 44-year-old male nonveterans, veterans who were not receiving care from the Department of Veterans Affairs (VA), and veterans currently receiving VA care who reported at least five days of poor mental health in the past month, by part of the year in which the respondent was intervieweda
a Data from the 2000 and 2003 Behavioral Risk Factor Surveillance System (BRFSS) health surveys
1. Hoge CW, Castro CA, Messer SC, et al: Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine 351:13–22,2004Crossref, Medline, Google Scholar
2. West A, Weeks WB: Reports of physical and mental distress in a national health survey are highest among younger non-metropolitan VHA patients. Journal of Rural Health, in pressGoogle Scholar
3. Kazis LE, Miller, DR, Clark, J, et al: Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Archives of Internal Medicine 158:626–632,1998Crossref, Medline, Google Scholar
4. Natelson BH, Tiersky L, Nelson J: The diagnosis of posttraumatic stress disorder in Gulf veterans with medically unexplained fatiguing illness. Journal of Nervous and Mental Disease 189:795–796,2001Crossref, Medline, Google Scholar
5. Lebowitz BD, Pearson JL, Schneider LS, et al: Diagnosis and treatment of depression in late life: consensus statement update. JAMA 278:1186–1190,1997Crossref, Medline, Google Scholar
6. Sarkisian CA, Lee-Henderson MH, Mangione CM: Do depressed older adults who attribute depression to "old age" believe it is important to seek care? Journal of General Internal Medicine 18:1001–1005,2003Google Scholar
7. Wayment HA: It could have been me: vicarious victims and disaster-focused distress. Personality and Social Psychology Bulletin 30:515–528,2004Crossref, Medline, Google Scholar
8. Ahern J, Galea S, Resnick H, Vlahov D: Television images and probable posttraumatic stress disorder after September11: the role of background characteristics, event exposures, and peri-event panic. Journal of Nervous and Mental Disease 192:217–226,2004Crossref, Medline, Google Scholar



