High Utilizers of Psychiatric Emergency Services
Abstract
OBJECTIVE: The purpose of this study was to examine the sociodemographic and clinical characteristics of high utilizers of psychiatric emergency services. METHODS: Data were collected over four years for 761 patients who were identified as high utilizers according to three definitions (two standard deviations above the mean number of visits to an urban psychiatric emergency service, six visits in a year, and four visits in a quarter) and for 1,585 nonfrequent utilizers (control group). Univariate analysis of variance and logistic regression models were used to determine group differences. RESULTS: Two distinct groups of high utilizers emerged: high utilizers by quarter and high utilizers by standard deviation. Compared with the control group, the high utilizers were more likely to be homeless, to have developmental delays, to be enrolled in a mental health plan, to have a history of voluntary and involuntary hospitalizations, to be uncooperative, to have personality disorders, to have unreliable social support, and to have a lifetime history of incarceration and detoxification. Compared with the high utilizers by quarter, the high utilizers by standard deviation had more visits and were more likely to have a history of incarceration and psychiatric hospitalization, more likely to be enrolled in mental health plan, and less likely to be homeless. CONCLUSIONS: High utilizers make up a small percentage of individuals who seek care in psychiatric emergency services and disproportionately use resources. It may be helpful to use two definitions of high utilizer to identify patients at different phases of their illness and to guide clinical interventions and mental health policies.
Recent data from the National Hospital Ambulatory Medical Care Survey show a 15 percent increase in psychiatric emergency department visits between 1992 and 2000 (1). This shift in where psychiatric patients are obtaining care is a consequence of deinstitutionalization (2), increasingly limited outpatient resources (2), and an increase in substance abuse (3). It is a proxy measure for failure of the outpatient mental health system to accommodate the increasingly complex service needs of patients (4).
Although failures in the availability or effectiveness of outpatient treatment that result in a single or repeat visit are understandable, multiple return visits to psychiatric emergency services—so-called high utilization—clearly indicate a quality-of-care or access problem in the outpatient arena and result in an increased cost burden on the mental health system. To address this problem, one must clarify the risk factors for repeat visits to psychiatric emergency services. Such an approach would allow identification of types of patients and their service needs, which in turn could lead to improved outpatient services and cost savings.
A number of demographic, clinical, and social characteristics have been identified as predictors of repeat visits to psychiatric emergency services. These characteristics include being a younger male (5,6,7,8), nonwhite (5,8), unmarried (8), and unemployed (8,9); having a psychotic disorder or schizophrenia (7,8,9), substance abuse (5,7), a personality disorder (8), a history of previous hospitalization (5,7), and a need for medications (5); and lack of social support or homelessness (5,6,9).
A major problem in interpreting these results is that there is no standard definition of high utilization beyond the fact that these patients repeatedly visit the emergency department. High utilizers have been defined as individuals with more than one visit in a four-, six-, or 12-month period (10); with more than six visits in an indeterminate period (11); with six or more visits in a 12-month period; and with a visit frequency in the upper tenth percentile (6). Our county public mental health care division uses another criterion, four or more visits in a quarter.
In the study reported here, we focused on high utilizers of psychiatric emergency services in a busy, urban emergency department and attempted to answer three related questions. First, what is the prevalence and overlap of patients defined by three definitions of high utilization? Second, given the definitions, what are the associated patient characteristics? Do the patient characteristics that distinguish the high-utilization group from the control group differ according to the definition of high utilization used to form the group? Finally, is there clinical utility and value in using different definitions?
Methods
Setting
The study took place at Harborview Medical Center's crisis triage unit, a psychiatric emergency service that serves the city of Seattle. The service receives more than 9,000 annual visits and is staffed 24 hours a day by attending psychiatrists, psychiatric residents, nurse practitioners, nurses, and social workers.
Sample
This retrospective study used data from the psychiatric emergency service's quality assurance database. Permission to use this database for analysis and publication was granted by the University of Washington's human subjects committee. Data were obtained for 17,481 unique individuals who made 31,731 visits to the crisis triage unit from July 1999 to July 2003. Most individuals (90.6 percent) had between one and three visits during this period (N=15,851). A total of 761 patients (4.4 percent) were identified as high utilizers by at least one of three definitions: patients with visits at least two standard deviations above the mean number of visits (selected because standard deviation units are the most common measure of variability); patients with six or more visits in a single year (selection on the basis of previous studies [5,11]); and patients with four or more visits in one quarter (selected on the basis of the definition by our county). Another 869 patients had four to six visits to the crisis triage unit in the four-year period and were thus eliminated from further analysis because they did not meet any of our high-utilizer criteria.
Assessments
On each visit clinicians completed a previously validated assessment form (12), providing demographic information and ratings of presenting psychiatric symptoms, which were computed across multiple visits. The ratings used a scale of 0 to 6, with 0 indicating lack of symptoms and higher scores indicating greater severity of symptoms. The demographic variables included gender, age, race, employment status, residence status, enrollment status in a regional mental health plan, and developmental disability status.
The clinical psychiatric variables included anxiety, depression, hostility, homicidality, psychosis, suicidality, uncooperativeness, and alcohol and drug abuse. Severity of medical illness was computed as a percentage of visits rated as moderate to severe illness, defined as serious problems such as advanced diabetes, heart disease, or life-threatening problems, such as sepsis, cancer, and AIDS. Functional ratings included functioning in activities of daily living, role functioning, outpatient treatment involvement, alcohol- or drug-related problems, and lack of a social support system. The six-point severity ratings are items used in the Psychiatric Assessment Form (13), which include a behaviorally anchored set of descriptors for each pair of points. For each symptom and functioning ratings we used the mean of the scores from multiple visits.
The clinicians' diagnoses were computed as percentages across multiple visits and included ten diagnostic syndromes. Self-reported clinical lifetime history included psychiatric hospitalizations, involuntary psychiatric treatments, incarcerations, and history of substance abuse treatments, detoxification, and sobering, also computed as percentages across multiple visits. Administrative and service variables, obtained from our automated medical record system, included the source of the patients' referral to the crisis triage unit, referral for hospitalization, and time spent in the crisis triage unit.
Statistical analyses
For group differences between the utilization groups, chi square analyses with correction for continuity were used for categorical data, and analyses of variance were used for continuous data. Because of the large number of statistical tests, only results for which p was below .001 were considered statistically significant. For a significant group effect (p<.001), post hoc tests, using a Bonferroni correction to the alpha level (p<.001), were conducted to determine which group differences were responsible for the significance.
To summarize our findings, logistic regressions were performed to find the most salient and independently significant variables that discriminated the utilization groups. Only variables that were statistically significant in the bivariate comparisons were tested in the models. Using a p value of below .001 for statistical significance, we examined the full model with all terms, along with models arrived at by both backwards and forwards elimination procedures. The final models presented contain only terms significant at p<.001 from all three modeling procedures.
Results
Prevalence and overlap of definitions of high utilization
The mean±SD number of visits to the crisis triage unit for all the patients in the sample during the four-year period was 1.8±2.3. A total of 761 individuals (4.4 percent) were identified as high utilizers. A total of 557 patients with seven or more visits met the criterion for high utilizers by standard deviation. A total of 419 patients met the criterion of six or more visits in a year (high utilizers by year), and 520 patients met the criterion of four or more visits in one quarter (high utilizers by quarter). Patients could meet criteria for any combination of the above definitions. On the basis of these definitions, we collapsed the seven observed combinations of high utilization groups into three groups. In addition, we identified a group of control patients, or crisis triage unit patients who were not high utilizers of services. The four comparison groups were as follows. Patients classified as high utilizers by all three definitions (N=300, or 1.7 percent) had at least seven visits, six of which occurred within a single year and four within a single quarter. The mean number of visits for this group was 13.9±7.7. Patients classified as high utilizers by standard deviation (N=257, or 1.5 percent) had at least seven visits in the four years. A total of 156 patients met the two-standard-deviations criterion alone, 62 met the two-standard-deviations and six-per-year criteria, and 39 met the two-standard-deviations and four-per-quarter criteria. The mean number of visits for this group was 8.3±1.7. Patients classified as high utilizers by quarter (N=204, or 1.2 percent) had at least four visits in a single quarter. A total of 147 patients met the four-visits-per-quarter criterion alone, and 34 patients met the four-visits-per-quarter criteria and also met the criteria for six-per-year. Because only 23 patients met the sole criteria for six-per-year, we incorporated this group into the four-visits-per-quarter classification, because their average number of visits (6.0) was closer to the mean number of visits for this group, than the other two groups. The mean number of visits for this group was 5.0±.8. Finally, patients with one to three visits within the four-year period were the control patients. To avoid an imbalance because of the large sample (N=15,851), we selected a random sample of 10 percent for study (N=1,585). This sample size was about double the size of the combined groups of high utilizers and was considered a good-sized control group.
After comparing all four groups on all variables, we observed only three differences between the high-utilizer group that met all three definitions and the high-utilizer group by standard deviation: the number of visits over the four-year period (13.9 compared with 8.3), the percentage of patients who reported living independently at all visits (7 percent compared with 18 percent), and the average level of social support (less versus more). Thus these two groups were combined and the analyses were recalculated with three groups: the control group, high utilization by quarter, and high utilization by standard deviation per year. High-utilizer visits accounted for 23 percent of all visits (7,298 visits).
High utilizers' characteristics and comparisons
Comparisons of demographic and lifetime clinical characteristics are presented in Table 1. The groups differed in gender (there was a larger proportion of females in the control group), unemployment rate (the high utilizers by quarter were significantly more likely to be unemployed than the control patients), the percentage of patients who were enrolled in the public mental health system (the high utilizers by standard deviation were the most likely to be enrolled), and rates of developmental disability, homelessness, and independent living (all lowest in the control group). The control group had lower rates of lifetime psychiatric hospitalization, involuntary psychiatric hospitalization, incarceration, and detoxification compared with both high-utilizer groups as well as a lower rate of history of substance abuse treatment and sobering compared with the high utilizers by standard deviation. The high utilizers by quarter had lower rates of psychiatric hospitalizations and incarceration than the high utilizers by standard deviation.
Comparisons of psychiatric diagnoses are presented in Table 2. Patients in the control group were more likely to receive a diagnosis of depression or anxiety and less likely to receive a diagnosis of schizophrenia than those in the high-utilizer group and had a significantly higher rate of adjustment disorder but a lower rate of borderline personality disorder, any personality disorder, or a comorbid substance-related diagnosis than the high utilizers by standard deviation.
Visit characteristics are presented in Table 3. The high utilizers by standard deviation had on average the most visits (11 visits), followed by the high utilizers by quarter (five visits) and the controls (1.6 visits). The control patients spent one hour less in the crisis triage unit per visit than did patients in the two high-utilizer groups. Patients in the control group had a lower rate of involuntary admissions (11 percent compared with 15 percent) and were more likely to be brought in by the police or by family or friends than the high utilizers.
The mean ratings of symptoms and functioning are presented in Table 4. Although the control group had more severe depression and anxiety symptoms than the high utilizers by standard deviation, the control group also had less severe hostility, less psychosis and uncooperativeness, better functioning, fewer alcohol and drug problems, and better social support systems than both high-utilizer groups.
The logistic regression analyses that discriminated the control patients from the high utilizers by quarter began with the 23 variables that were statistically different between the groups. The final model contained seven independently and uniquely significant variables (Table 5). Compared with the control group, the high utilizers by quarter were 6.1 times as likely to be homeless at some point; 4.3 times as likely to be developmentally disabled; 2.5 times as likely to have a history of psychiatric hospitalization or an involuntary hospitalization and to be enrolled in the county public mental health system; and 1.5 times as likely to be rated as being uncooperative and having unreliable social support.
The logistic regression analyses that discriminated the control group from the high utilizers by standard deviation began with 30 variables that were statistically different between the groups. The final model contained nine variables (Table 5). Compared with the control group, the high utilizers by standard deviation were more than six times as likely to have had an episode of homelessness, personality disorder, or developmental disability and to be enrolled in the county public mental health system. The high utilizers by standard deviation were also more than three times as likely to have had a psychiatric hospitalization, an episode of detoxification, or an involuntary hospitalization; 2.4 times as likely to have been incarcerated; and slightly but significantly more likely to be rated uncooperative.
Only four variables were significant in the final logistic regression analyses discriminating the high utilizers by quarter and the high utilizers by standard deviation. The high utilizers by standard deviation were almost three times as likely to have a history of incarceration and about 2.5 times as likely to have a history of psychiatric hospitalization and be enrolled in the county public mental health system but were less likely to have been homeless compared with the high utilizers by quarter.
Clinical utility of using different definitions
By using different definitions, two distinct groups of patients were identified, the acute and the chronic groups. The patients with four visits in three months—that is, high utilizers in a quarter—and the patients with two standard deviations above the mean number of visits, or at least seven visits in the four-year period, clearly had different demographic, clinical, and social characteristics, as presented in Table 1,2, 3,4,5.
Discussion
High service utilizers made up a small percentage of individuals who were evaluated in the crisis triage unit but utilized a disproportionate share of resources. Their visits accounted for almost a quarter of all visits. After small subgroups and overlapping definitions were eliminated, two distinct groups emerged: high utilizers by quarter (patients with four visits in three months) and high utilizers by standard deviation (patients with two standard deviations above the mean number of visits, or at least seven visits in the four-year period). These two groups were similar in terms of characteristics that distinguished them from the control group. They were more likely to be homeless; to have a history of developmental delay; to be enrolled in the regional mental health plan; to have a history of psychiatric hospitalizations, uncooperativeness, personality disorders, or unreliable social support; and to have a lifetime history of incarceration and detoxification. Of note, they had the same rates of bipolar disorder, dementia, or substance-related disorder; the same likelihood of being hospitalized after their emergency visit; similar outpatient treatment involvement; and similar likelihood of homicide or suicide.
However, despite these similarities, some important differences were noted. Patients defined by the two-standard-deviation definition of utilization had more visits to the crisis triage unit over the four-year period compared with the four-visits-per-quarter group (5,11) and were more likely to have a history of incarceration and psychiatric hospitalization and to be enrolled in a regional mental health plan and were less likely to be homeless. These characteristics depict two different kinds of high utilizers. One group (high utilizers by standard deviation) was more chronically mentally ill, was more likely to have housing services (less homelessness) and involvement with the public mental health system, and had more severe and aberrant behavior, alternately leading to hospitalization or prompting incarceration. Despite enrollment in the county mental health system, these patients continue to use psychiatric emergency services, which might be related to the refractoriness of their illness, although disruption in the use of outpatient resources by incarceration might also contribute to their recidivism.
In contrast, high utilizers defined by the four-visits-per-quarter definition seem to be acutely sick and may have a cluster of visits or a "bed episode" during which they tend to be homeless, unemployed, and not likely to be enrolled in the mental health plan. This relatively smaller group of patients (less than one-third of high utilizers) may represent a transitional group of patients who are on the way to becoming more chronically ill and whose illness is becoming more treatment refractory. Alternatively, these patients might be experiencing the first onset of a mental disorder and may have used psychiatric emergency services before appropriate referrals (5) were made or in an acute and time-limited exacerbation of a chronic illness—for example, during a therapist' absence or transition, or during a transition into new housing. Another possibility is that their illness was misdiagnosed—for example, they may have had a dual diagnosis or a medical illness that was not yet recognized as such.
Although we confirmed some of the characteristics of high utilizers found in previous studies, such as a history of psychiatric hospitalizations (5,7), homelessness, inadequate social support (5,6,9), and personality disorders (8), we did not find that age, race, and primary substance use distinguished high utilizers from nonfrequent utilizers. Although chronically ill high utilizers (high utilizers by standard deviation) were more likely to have a comorbid substance-related diagnosis in the logistic regression, this variable was not found to be an independent risk factor. However, substance-related diagnoses might explain why high utilizers spent almost one hour longer in the crisis triage unit—possibly they were "sobering up." Finally, although high utilizers were twice as likely to have schizophrenia, schizophrenia was not found to be an independent risk factor for high utilization. These data suggest that social and lifetime clinical history rather than symptom severity are independent risk factors for high use of psychiatric emergency services.
Although high utilizers identified by two different definitions were highly similar in terms of clinical and symptom severity ratings, these definitions seem to capture patients on two different trajectories or at two distinct phases of their illness (acute versus chronic) and thus may be useful in guiding clinical intervention and mental health policies that affect programs and funding. For high utilizers defined by the four-visits-per-quarter definition, who may be in transition before becoming more chronically ill (or experiencing the first onset of a mental disorder), interventions based either in psychiatric emergency services or an outpatient crisis intervention service could focus on resolving the acute episode and providing links to outpatient services to prevent them from becoming more chronically ill.
For high utilizers who had the larger number of visits to the emergency department and who may already be linked up with outpatient services, efforts need to be made to review the services they receive, determine what role incarceration plays in interrupting their continuity of care, and determine whether more intensive or different kinds of outpatient services would reduce their use. Future studies would need to replicate our findings with the two-standard-deviation definition of high utilization, given that standard deviation is relative to the size of patient sample. However the most frequently used criterion—six visits per year—is not very different from our definition of standard deviation (seven visits per four-year period).
Our study was limited by its retrospective study design, interrater variability, use of information not verified by hospital records or laboratory findings, and use of an automated hospital database. Despite these limitations, the unique aspects of our study include its use of three definitions of high utilization, the large sample, analysis of data collected over a four-year period, comparisons with a control group, and description of a variety of clinical, social, and service characteristics that have not been previously published.
Conclusions
This study showed that in a four-year period, high utilizers of services made up about 4 percent of individuals seeking care in the psychiatric emergency service, and yet these individuals accounted for 23 percent of all visits. By using different definitions of high utilization—four-visits-per-quarter and two standard deviations above the mean number of visits—two distinct subpopulations of high utilizers were identified: persons with more chronic, persistent, and severe mental illness—who tend to be enrolled in public mental health plans, have housing, and have aberrant behavior leading to hospitalization or incarceration—and those who are acutely ill, who have a cluster of visits during which they tend to be homeless, unemployed, and not likely be enrolled in a mental health plan. These two definitions may be useful in identifying patients who are on different trajectories or at different phases of their illness and ultimately guiding clinical interventions and mental health policies tailored to their respective group needs.
The authors are affiliated with the department of psychiatry and behavioral sciences of the University of Washington at Harborview Medical Center in Seattle. Send correspondence to Dr. Roy-Byrne at Box 359911, Psychiatry, Harborview Medical Center, 325 Ninth Avenue, Seattle, Washington 98104 (e-mail, [email protected]).
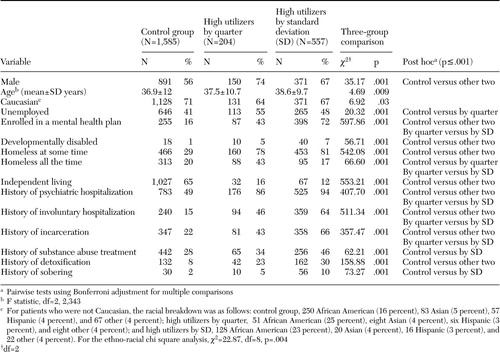 |
Table 1. Demographic characteristics of patients utilizing psychiatric emergency services, by high-utilization group
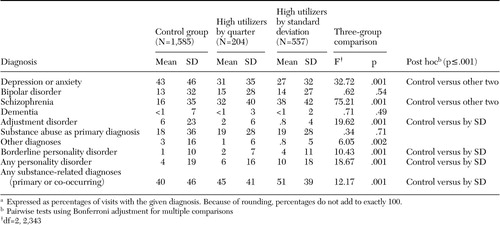 |
Table 2. Primary psychiatric diagnoses in a sample of patients utilizing psychiatric emergency services, by high-utilization groupa
aExpressed as percentages of visits with the given diagnosis. Because of rounding, percentages do not add to exactly 100.
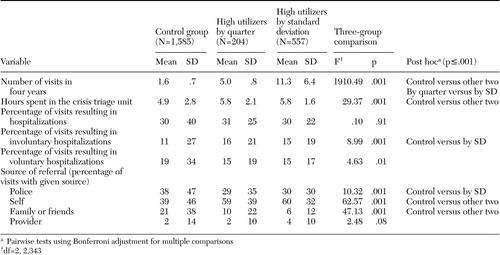 |
Table 3. Characteristics of clinical visits to a psychiatric emergency service, by high-utilization group
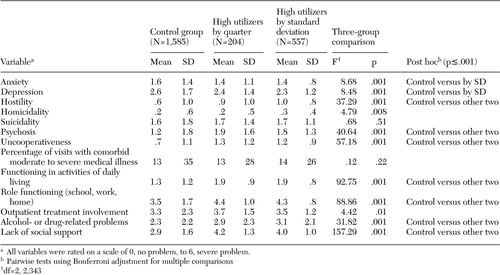 |
Table 4. Mean ratings of symptoms and functioning at admission to the crisis triage unit among high utilizers of a psychiatric emergency service
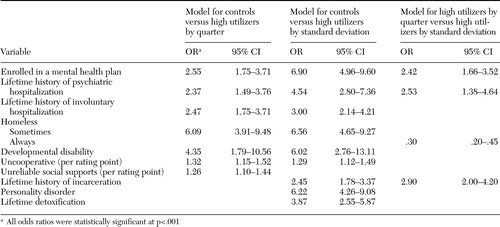 |
Table 5. Logistic regression results for patients utilizing psychiatric emergency services
1. Hazlett S, McCarthy M, Londner M, et al: Epidemiology of adult psychiatry visits to US emergency departments. Academic Emergency Medicine 11:193–195,2004Crossref, Medline, Google Scholar
2. Lamb H, Bachrach L: Some perspectives on deinstitutionalization. Psychiatric Services 52:1039–1045,2001Link, Google Scholar
3. Schiller M, Shumway M, Batki S: Patterns of substance use among patients in an urban psychiatric emergency service. Psychiatric Services 51:113–115,2000Link, Google Scholar
4. Wingerson D, Russo J, Ries R, et al: Use of psychiatric emergency services and enrollment status in a public managed mental health care plan. Psychiatric Services 52:1494–1501,2001Link, Google Scholar
5. Arfken C, Zeman L, Yeager L, et al: Case-control study of frequent visitors to an urban psychiatric emergency service. Psychiatric Services 55:295–301,2004Link, Google Scholar
6. Saarento O, Hakko H, Jaukamaa M: Repeated use of psychiatric emergency out-patient services among new patients: a 3-year follow-up study. Acta Psychiatrica Scandinavica 98:276–282,1998Crossref, Medline, Google Scholar
7. Spooren D, De Bacquer D, Van Heeringen K, et al: Repeated psychiatric referrals to Belgian emergency departments: a survival analysis of the time interval between first and second episodes. European Journal of Emergency Medicine 4:61–67,1997Crossref, Medline, Google Scholar
8. Sullivan P, Bulik C, Forman S, et al: Characteristics of repeat users of a psychiatric emergency service. Hospital and Community Psychiatry 44:376–380,1993Abstract, Google Scholar
9. Dhossche D, Ghani S: A study on recidivism in the psychiatric emergency room. Annals of Clinical Psychiatry 10:59–67,1998Crossref, Medline, Google Scholar
10. Ellison J, Blum N, Barsky A: Repeat visitors in the psychiatric emergency service: a critical review of the data. Hospital and Community Psychiatry 37:37–41,1986Abstract, Google Scholar
11. Ellison J, Blum N, Barsky A: Frequent repeaters in a psychiatric emergency service. Hospital and Community Psychiatry 40:958–960,1989Abstract, Google Scholar
12. Roy-Byrne P, Russo J, Rabin L, et al: A brief medical necessity scale for mental disorders: reliability, validity, and clinical utility. Journal of Behavioral Health Services and Research 25:412–424,1998Crossref, Medline, Google Scholar
13. Roy-Byrne P, Dagadakis C, Ries R, et al: A psychiatrist-rated battery of measures for assessing the clinical status of psychiatric inpatients. Psychiatric Services 46:347–352,1995Link, Google Scholar



