Racial Differences in the Treatment of Veterans With Bipolar Disorder
Abstract
OBJECTIVES: The authors examined whether African Americans, compared with whites, received guideline-concordant care for bipolar I disorder. METHODS: A retrospective analysis was conducted of data for patients who received a diagnosis of bipolar I disorder in fiscal year 2001 and received care in facilities in the Department of Veterans Affairs (VA) mid-Atlantic region. Indicators of guideline-concordant care were based on prescription data and data on utilization of inpatient and outpatient services from VA databases. RESULTS: A total of 2,316 patients with a diagnosis of bipolar I disorder were identified. Their mean age was 52 years; 9.4 percent (N=218) were women, and 13.1 percent (N=303) were African American. Overall, mood stabilizers were prescribed for 74.6 percent (N=1,728) of the patients; 67.1 percent (N=1,554) had an outpatient mental health visit within 90 days after the index diagnosis, and 54.3 percent (N=1,258) had an outpatient visit within 30 days after discharge from a psychiatric hospitalization. Multivariate logistic regression analyses with adjustment for sociodemographic and facility factors revealed that African Americans were less likely than whites to have an outpatient follow-up visit within 90 days after the index diagnosis. Race was not associated with receipt of mood stabilizers or use of outpatient services after a hospital discharge. CONCLUSIONS: Although a majority of patients received guideline-concordant care for bipolar disorder, potential gaps in continuity of outpatient care may exist for African-American patients.
Bipolar disorder is a chronic illness associated with functional impairment and significant health care costs (1,2). Without adequate treatment, a 25-year-old person with bipolar disorder can expect to lose 14 years of instrumental role functioning and nine years of life (3). Hence, eliminating potential gaps in the receipt of guideline-concordant care for this condition is highly important.
Despite the existence of practice guidelines for the appropriate treatment of bipolar disorder (4,5,6), outcomes for this illness remain suboptimal (2,7). Evidence suggests that racial and ethnic minority groups, particularly African Americans, are less likely than whites to receive adequate care for mental disorders (8,9,10), even within the context of apparent equal access to care—for example, within health care services provided by the Department of Veterans Affairs (VA) (9,10).
Disparities in the receipt of guideline-concordant care by patients with a diagnosis of bipolar disorder have not been adequately explored (7). Bipolar disorder presents a unique challenge in attempts to improve care (7) because of the cyclical nature of the disorder's manic and depressive episodes, which lead to poor treatment adherence, substance abuse, and subsequent social instability, all of which may disproportionately affect African Americans compared with whites (11).
Therefore, the implementation of indicators to identify potential gaps in guideline-concordant care for mental disorders is an important step toward reducing disparities in care for bipolar disorder, as well as other health conditions (12,13). If African-American patients are experiencing gaps in processes or outcomes of care, then providers should consider treatment strategies that redress these gaps. The purpose of the study reported here was to determine whether African Americans are less likely than whites to receive adequate pharmacotherapy and outpatient care for bipolar disorder (14).
Methods
Setting and study population
We conducted a retrospective cohort study using data from the VA National Patient Care Database. We identified patients who received a diagnosis of bipolar I disorder in fiscal year (FY) 2001 and who received care at one of ten facilities in the VA Stars and Stripes Healthcare Network (the VA's regional Integrated Service Network 4, or VISN 4) located in the mid-Atlantic region of the United States. VISN 4 includes Pennsylvania and Delaware and parts of Maryland, West Virginia, New York, and Ohio. All patients in VISN 4 with either one inpatient visit or two outpatient visits associated with an ICD-9 diagnosis of bipolar I disorder (ICD-9 codes 296.0x, 296.1x, 296.4x, 296.5x, 296.6x, 296.7x, and 296.8-296.82, inclusive) were included. The date of the first inpatient or outpatient visit with an ICD-9 diagnosis of bipolar I disorder to occur in FY 2001 was considered the index diagnosis date. To maximize the specificity of the diagnoses and limit inclusion of rule-out diagnoses, we limited the sample to patients with either one inpatient visit or two outpatient visits on separate dates that were associated with a diagnosis of bipolar I disorder. This strategy was based on a previously established algorithm for identifying patients with a serious mental illness (15). The study methods were reviewed and approved by local institutional review boards. Participants were not required to provide informed consent, because we conducted a secondary analysis of existing data.
Data collection
We ascertained prescription data by using drug class codes from the VA Pharmacy Benefits Management Database (version 3.0) for the date of the index bipolar disorder diagnosis and for a period during FY 2001 and 2002 of up to 12 months after the diagnosis date. Outpatient visits to a mental health specialist during the period from the index diagnosis up to 12 months later were identified in the VA National Patient Care Database outpatient clinic files for FY 2001 and 2002 and were categorized by using VA clinic stop codes. Telephone contacts with mental health specialists were also ascertained. Use of inpatient services from the date of the index diagnosis up to 12 months later was ascertained from the VA National Patient Care Database patient treatment file. Psychiatric inpatient visits were identified on the basis of the record of the bed-section type at discharge. Complete lists of drug class, outpatient clinic stop, and inpatient bed-section codes used in this study are available from the authors.
Demographic data at the time of the index diagnosis were collected from the VA National Patient Care Database and included race or ethnicity, age, gender, marital status, and results of an income-based means test, which was used as a proxy for socioeconomic status. Missing demographic data were filled in whenever possible by using the most frequent value recorded for other inpatient and outpatient visits during FY 1998 to 2001 (16).
We also ascertained medical and substance use disorder diagnoses from the VA National Patient Care Database by using ICD-9 codes recorded for inpatient and outpatient visits in FY 2001. We calculated the total number of medical conditions by using a previously established algorithm (17,18). The number of medical conditions was based on Agency for Healthcare Research and Quality clinical classifications and included the following conditions: hypertension, congestive heart failure, peripheral vascular disease, stroke, ischemic heart disease, diabetes, hyperlipidemia, pancreatitis, thyroid disorders, obesity, hepatitis, lower back pain, arthritis, hip problems, chronic obstructive pulmonary disease, asthma, lung cancer, prostate cancer, skin cancer, spinal cord injury, other accidents or injuries, renal failure, gastric-related disorders, benign prostatic hyperplasia, HIV infection, headache, dementia, Alzheimer's disease, Parkinson's disease, multiple sclerosis, and anemia. Substance use disorder diagnoses were identified by using ICD-9 codes 291.00-291.99, 303.00-303.93, and 305.00-305.99 for alcohol psychosis, abuse, or dependence and codes 292.00-292.99 and 304.00-304.99 for drug psychosis, abuse, or dependence.
Guideline-concordant care
We selected three key indicators of guideline-concordant care for bipolar disorder that were similar to those previously developed by Suppes and colleagues (19) and Unutzer and colleagues (20). The indicators reflect appropriate psychiatric treatment for the vast majority of patients with a diagnosis of bipolar I disorder, regardless of whether their current episode diagnosis was a manic, depressive, or mixed episode and regardless of age group (such as mid-life or late-life). These indicators can be used to monitor the receipt of guideline-concordant care in routine care settings. The indicators listed below were used.
Prescription of a mood stabilizer for bipolar disorder. We examined whether patients received a prescription for a recommended mood stabilizer for bipolar disorder at any time during the one-year period. We identified appropriate pharmacotherapy for bipolar disorder on the basis of clinical practice guidelines of the American Psychiatric Association (APA) (4,5) and the VA (6), both of which give identical recommendations for pharmacotherapy. Recommended "bipolar-specific" mood stabilizer pharmacotherapy was defined as any prescription for lithium, divalproex, valproic acid, carbamazepine, or lamotrigine that occurred from the time of the index bipolar disorder diagnosis up to 12 months later. However, because atypical antipsychotic medications may also be considered recommended treatments for acute mania, a second version of this indicator—"any mood stabilizer"—was created. This category included any prescription for lithium, divalproex, valproic acid, carbamazepine, lamotrigine, or any second-generation antipsychotic medication (such as olanzapine, aripiprazole, quetiapine, risperidone, ziprasidone, or clozapine) that occurred from the date of the index bipolar disorder diagnosis up to 12 months later.
Mental health outpatient visit within 90 days from initial visit. Unutzer and colleagues (20) defined inadequate follow-up care for bipolar disorder as a gap between outpatient mental health visits (defined as a visit to a psychiatrist, psychologist, or other mental health professional) of more than 90 days and defined adequate follow-up care as a visit that occurred at or within 90 days after a previous visit.
Mental health outpatient visit within 30 days after discharge from a psychiatric hospitalization. Similarly, Unutzer and colleagues (20) defined adequate outpatient follow-up care after an inpatient psychiatric stay as an outpatient mental health visit at or within 30 days after the date of discharge from an inpatient psychiatric admission. We applied this indicator to the data for the patient's last psychiatric hospitalization in FY 2001.
We created two versions of each of the outpatient care indicators. One version included outpatient mental health visits only, and the second version included both outpatient mental health visits and telephone contacts with a mental health specialist.
Statistical analyses
Analyses were performed with SAS, version 8.2. For all analyses, we excluded patients who died by the end of FY 2002 and patients with missing or unknown demographic data, such as missing race or marital status data. We also excluded patients of races or ethnicities other than white or African American, given that very few patients in the sample were not members of one of these two groups.
Descriptive statistics and bivariate analyses by racial group were performed for each indicator. Multivariate logistic regression analysis was performed to determine whether race was independently associated with receipt of guideline-concordant care for bipolar disorder, with adjustment for patient factors such as age, gender, marital status, means test results, number of comorbid conditions, and presence of a substance use disorder. For the multivariate analyses, the outcome was the probability of receiving acceptable care, as indicated by receipt of a mood stabilizer and an outpatient visit within 90 days from an initial visit or within 30 days of hospital discharge. In these analyses, we adjusted for the fixed effect of the VA facility that was the site of care. Given that the quality and use of outpatient care may vary widely in different VA facilities, we examined the association between race, site, and guideline-concordant outpatient care by conducting a post hoc bivariate analysis in which sites were stratified into three groups by the percentage of the patients treated at the facility in FY 2001 who were white—more than 95 percent, 80 percent to 95 percent, and less than 80 percent.
Results
A total of 2,736 patients in VISN 4 had either one inpatient diagnosis or two outpatient diagnoses of bipolar I disorder during FY 2001. Of these patients, 2,316 were either white or African American, were alive at the end of FY 2002, and had all demographic data necessary for inclusion in the study. This remaining sample did not differ from the overall sample in distribution of demographic variables. The 2,316 patients had a mean±SD age of 52±12 years (range=19 to 89 years); 23.6 percent (N=547) were aged 60 years or older, 13.1 percent (N=303) were African American, and 9.4 percent (N=218) were female. In addition, 32.2 percent (N=746) were married, 37.5 percent (N=869) had more than three comorbid medical conditions, 24.1 percent (N=558) had two comorbid medical conditions, 22.4 percent (N=519) had one comorbid medical condition, and 32.4 percent (N=750) had a substance use disorder. The patient sample (N=2,316) was similar in demographic characteristics to the overall United States veteran patient population with bipolar disorder, in which the mean age was 52 years, the proportion of female patients was 11 percent, and the proportion of African-American patients was 12 percent (21).
Prescription of mood stabilizers
As Table 1 shows, a majority of the patients (74.6 percent) received bipolar-specific pharmacotherapy, and 84.4 percent received any mood stabilizer. No significant difference between African Americans and whites was found in the rate of receipt of bipolar-specific pharmacotherapy. The results of the bivariate and multivariate analyses also showed that African Americans and whites had similar rates of receipt of any mood stabilizer.
Outpatient follow-up care
As Table 1 shows, 67.1 percent of the patients had an outpatient visit within 90 days of the initial visit, and 71.1 percent had an outpatient visit or a telephone contact within 90 days. Bivariate analyses revealed that African Americans and whites had similar rates of outpatient follow-up care within 90 days and similar rates of either outpatient care or telephone contact. However, after adjustment for patient and facility factors in the multivariate analysis, African Americans were less likely to receive adequate outpatient care within 90 days after the index visit (Table 1). This finding was upheld even when telephone contacts were included in calculating the rate of outpatient follow-up care.
Posthospitalization follow-up care
Of the 2,316 patients, 553 (23.8 percent) had at least one psychiatric hospitalization during the study period. Data from three sites were excluded from the remaining analyses because these sites did not have any patients who were hospitalized during the study period. As shown in Table 1, of the 553 patients with a psychiatric hospitalization, 54.3 percent had an outpatient visit within 30 days after their discharge date. When telephone contacts were included in calculating the rate of outpatient care, the percentage of patients with an outpatient visit within the acceptable time frame rose to 73.6 percent. African Americans were less likely than whites to have an outpatient visit within 30 days after their discharge from a psychiatric hospitalization. However, differences in use of outpatient services were reduced and no longer significant when telephone contacts were included. After adjustment for patient and facility factors in the multivariate analysis, the association between race and receipt of an outpatient visit within 30 days after discharge from a psychiatric hospitalization was no longer significant, regardless of whether telephone contacts were included (Table 1).
For the indicators of outpatient service use, we determined whether receipt of guideline-concordant care varied by facility and race. A post hoc bivariate analysis in which sites were stratified by the percentage of white patients at the facility revealed that guideline-concordant outpatient follow-up care was worse at the facilities with the greatest proportion of white patients than at the facilities with fewer white patients (Figure 1). In contrast, the proportion of patients receiving follow-up care after discharge from a psychiatric hospitalization was greater at sites with the greatest proportion of white patients (Figure 2).
Discussion
A majority of VA patients in the study sample received guideline-concordant pharmacotherapy for bipolar I disorder. Nonetheless, our findings indicate that many patients did not receive adequate follow-up outpatient care, suggesting that greater efforts are needed to improve continuity of care. African-American patients were less likely than white patients to receive adequate outpatient care after their index diagnosis visit, although no significant racial differences were found in use of pharmacotherapy or receipt of outpatient follow-up care after hospitalization.
The lack of association between race and access to pharmacotherapy may be related to previous findings of higher rates of prescribing of antipsychotic medications for African-American patients with mental disorders compared with white patients. For example, previous research suggested that African-American patients were more likely than their white counterparts to receive antipsychotic medications for the treatment of new-onset mania (22).
Nonetheless, we were surprised to find that African Americans were no less likely than whites to receive an outpatient visit within 90 days after the index visit, although the analysis with adjustment for facility factors showed that African Americans were less likely to receive this care. Our post hoc analysis revealed that the receipt of guideline-concordant care differed markedly by facility and that care was less likely to be provided in facilities with a lower proportion of African Americans. Such facilities tended to be located in areas that were more rural, compared with the facilities with higher proportions of African-American patients, which tended to be in urban areas. Thus any differences in care by race were initially masked by unadjusted facility-level differences. A majority of African Americans were receiving care at sites that performed well on the indicators of guideline-concordant care overall; however, such care may not have been equally available for all racial groups within these sites. African Americans may have been less likely than whites to receive adequate outpatient care in these urban facilities because of unmeasured system-level characteristics, such as lack of culturally competent service providers.
Our overall findings also suggest that telephone contacts may help reduce disparities in care after hospitalization for patients with bipolar disorder, regardless of the patient's race. Telephone contacts are becoming an increasingly popular and effective mechanism for promoting continuity of care for mental disorders. Moreover, telephone contacts may actually help some patients "open up" with providers with whom they would otherwise remain guarded. Our own clinical observations with this population suggest that in some cases such patients are more likely to communicate with someone regarding their mental illness over the phone than in person.
This study had some limitations that warrant consideration. Our results are based on a secondary analysis of administrative data, which restricts our ability to determine why gaps in guideline-concordant care for bipolar disorder exist. For example, we cannot determine whether these gaps might be related to provider or system-level cultural competence or to patients' lack of transportation. We were also unable to assess monitoring of drug toxicity levels as potential indicators of receipt of guideline-concordant care, because laboratory data on a national level were unavailable and unreliable at the time of this study. In addition, because we limited the sample to patients with either one inpatient diagnosis or two outpatient diagnoses of bipolar I disorder, we missed patients who might have received an incorrect diagnosis. Evidence suggests that African Americans have historically been more likely to receive a diagnosis of schizophrenia rather than a mood disorder when a mood disorder diagnosis is warranted, and this pattern of misdiagnosis may further increase African American's risk of receiving inadequate treatment (23,24). Thus, particularly with regard to the African-American subpopulation, our estimates of receipt of guideline-concordant care may be conservative, because we evaluated only the care received by patients with confirmed diagnoses.
Also, we may not have identified all mental health utilization, because we used only VA data, and some patients may have sought care outside the VA. However, for a serious mental illness such as bipolar disorder, the vast majority of the patients in this study were likely to have received VA care because of the generous pharmacotherapy benefits, including nominal prescription copayments, and because these patients are required to see a VA provider in order to obtain medications through the VA. Finally, the generalizability of this study may be limited to patients treated within the VA system. However, it should be noted that individuals with severe or chronic mental disorders often receive care from publicly funded health care providers, such as the VA or Medicaid-funded providers. Thus, the VA patient population may include a disproportionately greater number of patients with bipolar disorder compared with the general patient population of the United States.
Despite these limitations, to our knowledge, this study is the first to focus on differences by race in the receipt of guideline-concordant care in routine treatment for bipolar disorder. Moreover, the dissemination of guideline-concordant care for bipolar disorder beyond controlled clinical environments has not been fully evaluated. Potential users of information, including consumers and purchasers, want a "bottom-line" conclusion about overall quality to inform decision-making processes regarding health care options (25). More recently, policy makers have advocated that potential disparities in quality of care be monitored (14) in order to benchmark performance across different provider organizations and inform resource allocation to reduce disparities in care. Developing and refining measures of use and quality of care constitute one of the first steps in improving efficiencies and patient outcomes. Such progress can inform the selection of specific interventions and more general approaches to health maintenance that have the potential to reduce costs and minimize adverse outcomes for patients with bipolar disorder.
Conclusions
This study had a number of important research and policy implications. First, in examining treatment of bipolar disorder, we applied measures of guideline-concordant care that can be used in future activities to monitor and improve the quality of care. In addition, we found that potential gaps may exist in the receipt of guideline-concordant outpatient care for bipolar disorder among African Americans. Subsequent initiatives that focus on improving the quality of care overall for bipolar disorder should therefore aim at on understanding the patient-, provider-, and system-level determinants of potential gaps in guideline-concordant outpatient care and on eventually redressing such gaps. Finally, as health care providers and policy makers call for additional efforts to monitor the quality of mental health care (25), greater efforts to implement and further refine indicators for specific conditions such as bipolar disorder are needed to ultimately improve outcomes for these patients.
Acknowledgments
This research was supported by the Health Services Research and Development Service of the Veterans Health Administration, Department of Veterans Affairs (VA) (IIR 02-283-2; A. Kilbourne, principal investigator). This work was also completed with the support of the Center for Health Equity Research and Promotion of the VA Pittsburgh Healthcare System (M. Fine, principal investigator) and the VA Mental Illness Research Education and Clinical Center awarded to the VA Pittsburgh Healthcare System and the Philadelphia VA Medical Center (I. Katz, principal investigator). Dr. Kilbourne is funded by a Career Development Award Merit Review Entry Program from the VA Health Services Research and Development program (MRP02269).
Dr. Kilbourne, Dr. Haas, Mr. Elder, and Dr. Good are affiliated with the Department of Veterans Affairs (VA) Pittsburgh Healthcare System. Dr. Kilbourne and Dr. Haas are also affiliated with the department of psychiatry at the University of Pittsburgh, with which Dr. Pincus is affiliated. Dr. Good is also with the department of medicine at the University of Pittsburgh, and Dr. Pincus is also with RAND-University of Pittsburgh Health Institute. Dr. Bauer is with the VA Providence Medical Center and the department of psychiatry and human behavior at Brown University in Providence, Rhode Island. Mr. Han is with the School of Medicine at the University of Pennsylvania in Philadelphia. Dr. Shad is with the department of psychiatry at the University of Texas Southwestern Medical Center in Dallas. Dr. Conigliaro is with the College of Medicine at the University of Kentucky in Lexington. Send correspondence to Dr. Kilbourne at the VA Pittsburgh Center for Health Equity, Research and Promotion, Mailstop 151-C, Building 28, Room 1A-116, University Drive C, Pittsburgh, Pennsylvania 15240. Data from this research were presented at AcademyHealth's annual research meeting, held June 7 to 11, 2004, in San Diego.
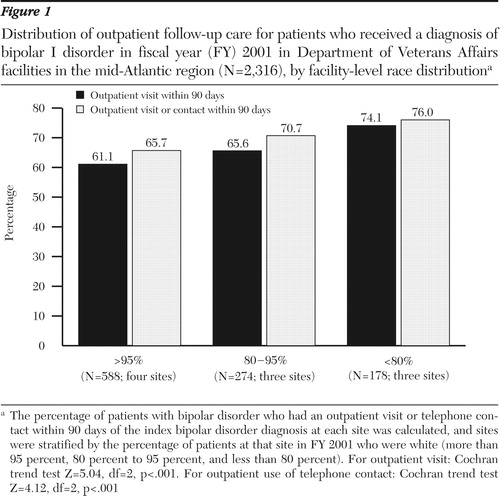
Figure 1. Distribution of outpatient follow-up care for patients who received a diagnosis of bipolar I disorder in fiscal year (FY) 2001 in Department of Veterans Affairs facilities in the mid-Atlantic region (N=2,316), by facility-level race distributiona
a The percentage of patients with bipolar disorder who had an outpatient visit or telephone contact within 90 days of the index bipolar disorder diagnosis at each site was calculated, and sites were stratified by the percentage of patients at that site in FY 2001 who were white (more than 95 percent, 80 percent to 95 percent, and less than 80 percent). For outpatient visit: Cochran trend test Z=5.04, df=2, p<.001. For outpatient use of telephone contact: Cochran trend test Z=4.12, df=2, p<.001
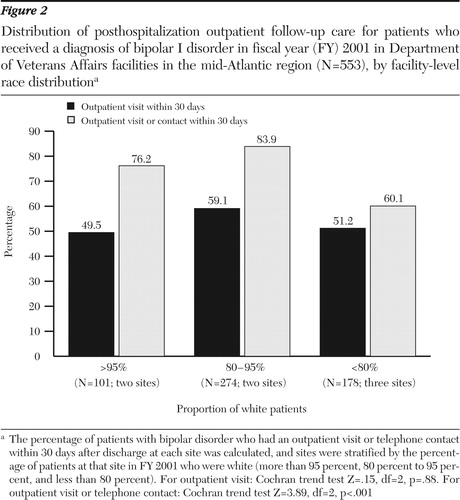
Figure 2. Distribution of posthospitalization outpatient follow-up care for patients who received a diagnosis of bipolar I disorder in fiscal year (FY) 2001 in Department of Veterans Affairs facilities in the mid-Atlantic region (N=553), by facility-level race distributiona
a The percentage of patients with bipolar disorder who had an outpatient visit or telephone contact within 30 days after discharge at each site was calculated, and sites were stratified by the percentage of patients at that site in FY 2001 who were white (more than 95 percent, 80 percent to 95 percent, and less than 80 percent). For outpatient visit: Cochran trend test Z=.15, df=2, p=.88. For outpatient visit or telephone contact: Cochran trend test Z=3.89, df=2, p<.001
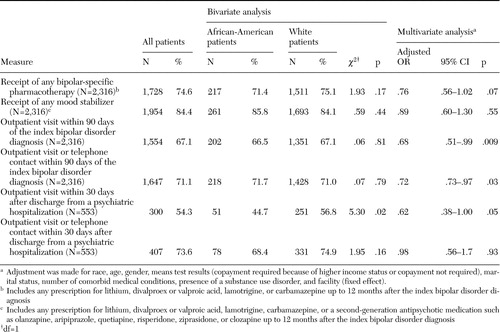 |
Table 1. Measures of quality of care for African-American and white patients who received a diagnosis of bipolar I disorder in fiscal year (FY) 2001 in Department of Veterans Affairs facilities in the mid-Atlantic region
1. Bauer MS, Kirk G, Gavin C, et al: Determinants of functional outcome and healthcare costs in bipolar disorder: a high-intensity follow-up study. Journal of Affective Disorders 65:231–241,2001Crossref, Medline, Google Scholar
2. Wells KB, Miranda J, Bauer MS, et al: Overcoming barriers to reducing the burden of affective disorders. Biological Psychiatry 52:655–675,2002Crossref, Medline, Google Scholar
3. Medical Practice Project: A State-of-the-Science Report for the Office of the Assistant Secretary for the United States Department of Health, Education and Welfare. Baltimore, Policy Research, 1979Google Scholar
4. American Psychiatric Association: Practice Guideline for the Treatment of Patients With Bipolar Disorder. American Journal of Psychiatry 151(Dec suppl), 1999Google Scholar
5. American Psychiatric Association: Practice Guideline for the Treatment of Patients With Bipolar Disorder (revision). American Journal of Psychiatry 159:S1-S50, 2002Google Scholar
6. Bauer MS, Callahan AM, Jampala C, et al: Clinical practice guidelines for bipolar disorder from the Department of Veterans Affairs. Journal of Clinical Psychiatry 60:9–21,1999Crossref, Medline, Google Scholar
7. Bauer M, Unutzer J, Pincus HA, et al: Bipolar disorder. Mental Health Services Research 4:225–229,2002Crossref, Medline, Google Scholar
8. US Department of Health and Human Services: Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md, US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, 2001.Google Scholar
9. Copeland LA, Zeber JA, Valenstein M, et al: Racial disparity in the use of atypical antipsychotic medications among veterans. American Journal of Psychiatry 160:1817–1822,2003Link, Google Scholar
10. Charbonneau A, Rosen AK, Ash AS, et al: Measuring the quality of depression care in a large integrated health system. Medical Care 41:669–680,2003Medline, Google Scholar
11. Kilbourne AM, Bauer M, Pincus HA, et al: Clinical, psychosocial, and treatment factors in minority patients with bipolar disorder. Bipolar Disorders 7:89–97,2005Crossref, Medline, Google Scholar
12. Institute of Medicine: Crossing the Quality Chasm. Washington, DC, National Academy Press, 2001Google Scholar
13. Institute of Medicine: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC, National Academy Press, 2002Google Scholar
14. Lurie N, Jung M, Lavizzo-Mourey R: Disparities and quality improvement: federal policy levers. Health Affairs 24(2):354–364,2005Google Scholar
15. Lurie N, Popkin M, Dysken M, et al: Accuracy of diagnoses of schizophrenia in Medicaid claims. Hospital and Community Psychiatry 43:69–71,1992Abstract, Google Scholar
16. Kressin NR, Chang BH, Hendricks A, et al: Agreement between administrative data and patients' self-reports of race/ethnicity. American Journal of Public Health 93:1734–1739,2003Crossref, Medline, Google Scholar
17. Yu W, Ravelo A, Wagner TH, et al: Prevalence and costs of chronic conditions in the VA health care system. Medical Care Research and Review 60(3 suppl):146S-167S,2003Google Scholar
18. Kilbourne AM; Cornelius J, Pincus HA, et al: Burden of medical comorbidities among individuals with bipolar disorder. Bipolar Disorders 6:368–373,2004Crossref, Medline, Google Scholar
19. Suppes T, Swann AC, Dennehy EB, et al: Texas Medication Algorithm Project: development and feasibility testing of a treatment algorithm for patients with bipolar disorder. Journal of Clinical Psychiatry 62:439–447,2001Crossref, Medline, Google Scholar
20. Unutzer J, Simon G, Pabiniak C, et al: The use of administrative data to assess quality of care for bipolar disorder in a large staff model HMO. General Hospital Psychiatry 22:1–10,2000Crossref, Medline, Google Scholar
21. Blow FC, McCarthy JF, Valenstein M: Care in the VHA for Veterans with Psychosis: FY99. First Annual Report on Veterans With Psychoses. VA National Serious Mental Illness Treatment Research and Evaluation Center. Nov 2000Google Scholar
22. Fleck DE, Hendricks WL, DelBello MP, et al: Differential prescription of maintenance antipsychotics to African American and white patients with new-onset bipolar disorder. Journal of Clinical Psychiatry 63:658–664,2002Crossref, Medline, Google Scholar
23. Kilbourne AM, Haas GL, Mulsant B, et al: Concurrent psychiatric diagnoses by age and race among persons with bipolar disorder. Psychiatric Services 55:931–933,2004Link, Google Scholar
24. Lawson WB: Clinical issues in the pharmacotherapy of African-Americans. Psychopharmacology Bulletin 32:275–281,1996Medline, Google Scholar
25. Hermann RC, Rollins CK: Quality measurement in health care: a need for leadership amid a new federalism. Harvard Review of Psychiatry 11:215–219,2003Crossref, Medline, Google Scholar



