Psychological Distress of Nurses in Taiwan Who Worked During the Outbreak of SARS
Abstract
OBJECTIVES: This study explored whether nurses who were working during the severe acute respiratory syndrome (SARS) crisis showed symptoms of distress. This study also examined whether nurses experienced stress from being conscripted to work in higher-risk units. METHODS: This study was conducted in Taiwan during the peak of the SARS outbreak in 2003. Participants were recruited from nursing staff in a community hospital. Participants were divided into three groups: those who originally worked in units with a high risk of SARS exposure (N=65), those who had been involuntarily conscripted into such units because of manpower demands (N=21), and those who worked in units with a low risk of SARS exposure (N=45). Participants were evaluated with two questionnaires: the Impact of Event Scale and the 90-item Symptom Checklist-Revised. RESULTS: The results showed that 11 percent of the nurses surveyed had stress reaction syndrome. The symptoms of psychological stress reactions included anxiety, depression, hostility, and somatization. The highest rate of stress reaction syndrome was observed in the group that originally worked in a high-risk unit, and the conscripted group experienced the most severe distress on average. CONCLUSIONS: These findings suggest that the psychological distress of nurses who worked during the SARS outbreak was moderate. The distress was more prominent among the two groups of nurses who were working with patients with SARS.
With more than 8,000 cases and 900 deaths during the 2003 outbreak, severe acute respiratory syndrome (SARS) has become a major international public health problem. The evolving nature and inherent scientific uncertainties of SARS outbreaks raised considerable fear, much like in the beginning of the AIDS epidemic. One very important SARS-related concern is that the occupational exposure faced by health care workers is potentially life threatening. At the peak of the outbreak most SARS cases involved hospital-acquired infections (1), and one Hong Kong study reported that as many as half the documented SARS cases involved health care workers (2). Nurses, the first line of health care workers, often experience the greatest occupational stress.
In addition, the SARS epidemic called for the involuntary conscription of health care workers, many of whom did not specialize in infectious diseases, to care for SARS patients, because of an insufficient number of eligible personnel to handle the sudden increase in workload. This outbreak also may have led to psychological conflicts between health care workers' responsibility to care for the ill and their right to protect themselves from a potentially lethal virus.
Thus SARS should be considered to be a disease that presents a combination of occupational stresses for health care workers. In light of a possible recurrence of a SARS outbreak or the emergence of similar highly contagious and lethal diseases, it is important to understand the nature of psychological distress of health care professionals who work with such diseases. This study explored whether nurses who were working during the SARS crisis experienced symptoms of distress. This study also examined whether nurses experienced psychological distress from being conscripted into higher-risk units.
Methods
This study used a cross-sectional and case-control design and was conducted in the Kaohsiung Municipal Hsiao-Kang hospital—a 460-bed general hospital in southern Taiwan—during mid-May 2003, at the peak of the SARS outbreak. During this period the hospital quarantined 27 patients who presented with suspected symptoms of SARS. Among these patients, eight probable cases and ten suspected cases were confirmed by Taiwan's Center for Disease Control. The research protocol was approved by the institutional review board of Kaohsiung Medical University in Taiwan, and written informed consent was obtained before data collection.
A total of 184 nurses working with patients in wards or emergency units in the hospital were invited to enter this study. Eighty-five nurses who worked in units with a higher risk of exposure to the SARS virus—including the emergency unit, intensive care unit, and general medical ward—were designated as the high-risk group. Thirty nurses who were conscripted from units with a lower risk of exposure to SARS into higher-risk units were designated as the conscripted group. Very few nurses in the hospital were conscripted voluntarily; most were assigned by drawing lots, and none opted out of the assignment. All the nurses in our conscripted group were conscripted involuntarily. Sixty-nine nurses who were working in units with a lower risk of SARS and who were not conscripted were designated as the control group.
Nurses were invited to participate in this study instead of being enrolled through random sampling. The response rate was 77 percent for the high-risk group (65 of 85 nurses), 70 percent for the conscripted group (21 of 30 nurses), and 61 percent for the control group (42 or 69 nurses). All participants completed the Impact of Event Scale (IES) (3) and the 90-item Symptom Checklist-Revised (SCL-90-R) (4,5). Data on participants' demographic characteristics and work history were also collected.
The 15-item self-administered IES has been widely used to measure stress reactions after various stressful events (6). Each item was administered by using 4-point frequency scales (0, not at all; 1, rarely; 3, sometimes; 5, often). The scale measures experiences that occurred during the past week. Possible scores on the IES range from 0 to 75, with higher scores indicating more severe stress reactions. Although a diagnosis of posttraumatic stress disorder (PTSD) cannot be based entirely on an IES score, scores above 35 are considered to be highly predictive of PTSD and to have the lowest apparent total misclassification error rate (7). In the study reported here, participants with scores of 35 or above were defined as having stress reaction syndrome. We also computed scores for two IES subscales: intrusion, consisting of seven items, and avoidance, consisting of eight items. Although a validation study has not been done for the IES specifically for the Taiwanese population, the IES has been widely used in Taiwan to assess symptoms after stress (8,9).
The SCL-90-R is a self-report rating scale designed to measure general psychopathology associated with the constructs of somatization, obsessive-compulsive symptoms, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Participants used this scale to rate 90 statements on the severity of symptoms that they may have experienced during the previous week. The SCL-90-R is a 5-point scale of distress, ranging from 0, not at all distressed, to 4, extremely distressed. The Global Severity Index (GSI) is the average score of items from the total scale of the SCL-90-R and from its subscales; possible scores on the GSI range from 0 to 4. The validity of the SCL-90-R in Taiwan has been established (10).
Although the nurses' scores on three subscales of the SCL-90R—obsessive-compulsive disorder, phobic anxiety, and paranoid ideation—indicated that their distress was characterized by anxiety and extreme worry about personal harm, the scores for the subscales are not reported here for two reasons. First, several obsessive-compulsive disorder subscale items measure behaviors that are normal under the circumstances of an outbreak of an infectious disease (for example, repeated hand-washing). Second, the subscales for phobic anxiety and paranoid ideation measure fears and worries that are, by definition of these disorders (that is, phobia and paranoia), unreasonable and baseless, which would also not be the case in these circumstances.
One-way analysis of variance tests or chi square analyses were used to compare demographic data and work history across the three groups. Bivariate correlations were calculated by using Pearson's correlation (for continuous variables) or Spearman's correlation (for categorical variables). To control for the confounding effect of demographic variables, analyses of covariance (ANCOVAs) followed by post hoc least-significant-difference comparisons were conducted to compare symptoms across the three groups of nurses. The alpha criterion for significance was .05 or less.
Results
The demographic and work characteristics of the three groups are shown in Table 1. Compared with the other groups, nurses in the high-risk group tended to be older (F=3.4, df=2, 125, p<.05) and had worked longer as a nurse (F=9.5, df=2, 125, p<.001). More women in the conscripted group were married (χ2=10, df=2, p<.01) and were mothers (χ2= 7.3, df=2, p<.05). Because high correlations were found between the number of months worked as a nurse and age (r=.79, p<.001) and between marital status and being a mother (rho=.69, p<.001), only the number of months worked as a nurse and marital status were included as covariates in the ANCOVAs.
Altogether, 14 nurses (11 percent) were found to have stress reaction syndrome. The distribution of cases was highest in the high-risk group (11 nurses, or 17 percent), followed by the conscripted group (two nurses, or 10 percent) and the control group (one nurse, or 2 percent). Compared with nurses who did not have stress reaction syndrome, those with stress reaction syndrome were found to present more severe symptoms as measured by GSI scores (t=2.9, df=126, p<.01) and by the scores of four symptom profiles of the SCL-90-R—anxiety (t=3.8, df=126, p<.001), depression (t=2.9, df=126, p<.01), hostility (t=2.9, df=126, p<.01), and somatization (t=2.1, df=126, p<.05).
The mean±SD IES and SCL-90-R scores for the three groups are presented in Table 2. The difference between the three groups was significant in the scores of the total IES (F=3.84, df=2, 124, p<.05), the intrusion subscale of the IES (F=3.49, df=2, 124, p<.05), the avoidance subscale of the IES (F=4.2, df=2, 124, p<.05), and the depression subscale of the SCL-90-R (F=3.13, df=2, 123, p<.05). The difference between the three groups was not significant for the scores of several subscales of the SCL-90-R: GSI, hostility, and psychoticism symptoms. Post hoc comparisons revealed that, compared with nurses in the control group, nurses in the conscripted group experienced more severe symptoms as measured by IES total scores, by the IES subscales of intrusion and avoidance, and by the SCL-90-R subscales of depression and hostility. Post hoc comparisons also revealed that, compared with nurses in the high-risk group, nurses in the conscripted group experienced more severe symptoms as measured by the IES intrusion subscale and by the SCL-90-R subscales of depression and psychoticism. Nurses in the high-risk group also experienced more severe symptoms than the control group as measured by the IES avoidance subscale.
Discussion
The results revealed that characteristics of SARS-related stress reaction syndrome included anxiety, depression, hostility, and somatization. Eleven percent of the nurses were found to have stress reaction syndrome, the highest rate of which was found in the group originally working in a higher-risk unit. Nevertheless, in some dimensions the conscripted group presented more severe psychological symptoms than the high-risk group.
The risk of psychological stress reaction varies according to the type of stressful event. One well-designed epidemiologic study evaluated the risk of PTSD in four classes of traumatic events—assaultive violence (21 percent), sudden unexpected death of a close friend or relative (14 percent), other injury or shocking experience (6 percent), and learning of trauma to others (2 percent)—and found a mean lifetime prevalence of PTSD of 9 percent for any class of trauma (11). Although differences in methodology, case-definition, and sampling method limit the applicability of a direct comparison of our data to the above study, the overall rate of stress reaction syndrome that we found among nurses in all three groups (11 percent) and among nurses who originally worked in units with a higher risk of SARS (17 percent) could be regarded as moderate.
An intriguing finding from our study is that a higher proportion of participants in the high-risk group had stress reaction syndrome, whereas psychopathology was more severe among nurses in the conscripted group. It is possible that personal coping strategies, individual vulnerability, a buffer effect of training and experience, and nurses' willingness to provide care might explain the discrepancy. All the nurses in the conscripted group were conscripted involuntarily. These nurses may have experienced more psychological conflict between professional obligation and evasion of life-threatening situations and a great deal of uncertainty about infection control measures, self-protection, and reward, which may have affected their willingness to work (12). On the other hand, nurses in the high-risk group had worked in the most demanding units, such as the emergency unit or acute medical wards, for some time. Compared with nurses in the conscripted group, nurses in the high-risk group had more experience working under pressure and were used to the potential exposure to possible occupational hazards; hence nurses in the high-risk group probably were more resilient to a high-stress environment. Also, nurses in the high-risk group received training for infection control during the initial stages of the SARS outbreak. Therefore, a high level of training, professional experience, and good social support might have buffered the average severity of symptoms among nurses in the high-risk group (13,14). However, nurses in the high-risk group experienced more psychological distress than those in the control group.
Several caveats about the methods of this study need to be mentioned. First, even though previous studies indicate that the IES is useful for measuring stress reactions after a range of traumatic events and is valuable for detecting individuals who require treatment (15,16), the case definition of stress reaction syndrome in this study that is based on a score of 35 or higher on the IES does not necessarily represent a diagnosis of PTSD or acute stress disorders. Second, nonrandom sampling in this study might raise the possibility of selection bias. Third, data from a relatively small study sample limit our ability to provide a clear statistical comparison of these three groups. Finally, our cross-sectional design limited the inference of causation between this type of occupational risk and psychological distress. The study could be improved if we could adopt a within-design study format to evaluate the distress level of all nurses before and after providing care.
Conclusions
On the basis of our findings, we recommend that nurses who work with highly contagious patients be given extensive training, adequate compensation, and meaningful reassurance to reduce their stress reactions—for example, offering continuous education on infection control and self-protection to promote professional expertise, providing a periodic health assessment to reassure nurses of their physical well-being, and screening at-risk nurses for distress so that psychological intervention can be provided.
The authors are affiliated with the department of psychiatry at Kaohsiung Medical University Chung-Ho Memorial Hospital, Number 100, Tzyou 1st Road, Kaohsiung City, 807, Taiwan (e-mail, [email protected]). Dr. Chen and Ms. Wu are also with Kaohsiung Municipal Hsiao-Kang Hospital in Taiwan.
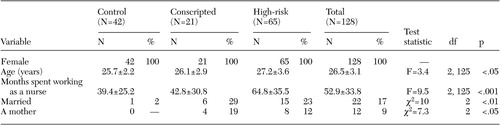 |
Table 1. Demographic data and work history of groups of nursing professionals who worked in Taiwan during the outbreak of severe acute respiratory syndrome in 2003
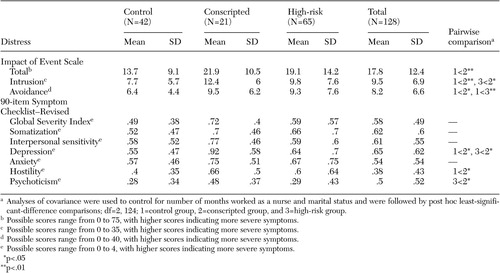 |
Table 2. Symptom presentations among groups of nurses who worked in Taiwan during the outbreak of severe acute respiratory syndrome in 2003
1. WHO issues consensus document on the epidemiology of SARS. Weekly Epidemiological Record 78:373–375, 2003Medline, Google Scholar
2. Lee N, Hui D, Wu A, et al: A major outbreak of severe acute respiratory syndrome in Hong Kong. New England Journal of Medicine 348:1986–1994, 2003Crossref, Medline, Google Scholar
3. Horowitz M, Wilner N, and Alvarez W: Impact of Event Scale: a measure of subjective stress. Psychosomatic Medicine 41:209–218, 1979Crossref, Medline, Google Scholar
4. Derogatis LR, Cleary PA: Factorial invariance across gender for the primary symptom dimensions of the SCL-90. British Journal of Social and Clinical Psychology 16:347–356, 1977Crossref, Medline, Google Scholar
5. Derogatis LR, Lipman RS, Covi L: SCL-90: an outpatient psychiatric rating scale—preliminary report. Psychopharmacology Bulletin 9:13–28, 1973Medline, Google Scholar
6. Sundin EC, Horowitz MJ: Horowitz's Impact of Event Scale evaluation of 20 years of use. Psychosomatic Medicine 65:870–876, 2003Crossref, Medline, Google Scholar
7. Neal LA, Busuttil W, Rollins J, et al: Convergent validity of measures of post-traumatic stress disorder in a mixed military and civilian population. Journal of Traumatic Stress 7:447–455, 1994Crossref, Medline, Google Scholar
8. Chang CM, Lee LC, Connor KM, et al: Posttraumatic distress and coping strategies among rescue workers after an earthquake. Journal of Nervous Mental Disease 191:391–398, 2003Crossref, Medline, Google Scholar
9. Hsu CC, Chong MY, Yang P, et al: Posttraumatic stress disorder among adolescent earthquake victims in Taiwan. Journal of the American Academy of Child Adolescent Psychiatry 41:875–881, 2002Crossref, Medline, Google Scholar
10. Tsai MT, Wen JK, Lin HN, et al: Application of self-rating symptom scales to psychiatric outpatients. Bulletin of Chinese Society of Neurology and Psychiatry 4:13–22, 1978Google Scholar
11. Breslau N, Kessler RC, Chilcoat HD, et al: Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry 55:626–632, 1998Crossref, Medline, Google Scholar
12. Tzeng HM: SARS infection control in Taiwan: investigation of nurses' professional obligation. Outcomes Management 7:186–193, 2003Medline, Google Scholar
13. Dyregrov A, Kristoffersen JI, Gjestad R: Voluntary and professional disaster-workers: similarities and differences in reactions. Journal of Traumatic Stress 9:541–555, 1996Crossref, Medline, Google Scholar
14. Weisaeth L: A study of behavioural responses to an industrial disaster. Acta Psychiatrica Scandinavica 355(suppl):13–24, 1989Google Scholar
15. Joseph S: Psychometric evaluation of Horowitz's Impact of Event Scale: a review. Journal of Traumatic Stress 13:101–113, 2000Crossref, Medline, Google Scholar
16. Sundin EC, Horowitz MJ: Impact of Event Scale: psychometric properties. British Journal of Psychiatry 180:205–209, 2002Crossref, Medline, Google Scholar



