Treatable Comorbid Conditions and Use of VA Health Care Services Among Patients With Dementia
Abstract
OBJECTIVE: Although dementia is a progressive degenerative disease, treatable comorbid symptoms, such as pain, aggression, depression, and psychosis, occur among more than 60 percent of patients with dementia. Compared with age-matched controls, patients with dementia use 70 percent more health services and account for 50 percent more managed care costs. This prospective study examined the longitudinal relationship between use of health care services and treatable comorbid conditions among patients with dementia. METHODS: Ninety-nine patient-caregiver dyads from the Michael E. DeBakey Veterans Affairs (VA) Medical Center in Houston, Texas, completed a one-time interview. Patients' VA records were reviewed one year later to examine the relationships between the study variables and three types of service use: inpatient medical stays, outpatient medical visits, and outpatient psychiatric visits. RESULTS: Pain was positively associated with all types of service use. Depression was associated with outpatient psychiatric visits. Psychosis and aggression were not significantly associated with future use of health care services. CONCLUSIONS: The results of this study confirm previous findings that pain and depression are associated with increased use of health care services. Although the other treatable comorbid symptoms, with the exception of pain, are associated with increased service use, their impact varies depending on the type of services provided. Interventions to improve the assessment and treatment of comorbid symptoms, especially pain, among patients with dementia may reduce service needs and thus reduce medical care costs.
Dementia is a progressive degenerative disease that has a substantial impact on health care costs. Patients with dementia use 70 percent more health services (1) and cost managed care organizations 50 percent more than age-matched controls (2). One significant factor contributing to this difference in health care costs is the fact that more than 60 percent of persons with dementia have treatable comorbid psychosocial symptoms, including pain, aggression, psychosis (hallucinations or delusions), and depression (3,4,5,6).
Aggression, depression, and psychosis are associated with elevated rates of service use (7); negative medical dispositions, including earlier institutionalization (8,9); increased caregiver burden (10); and decreased quality of life (11). Comorbid dementia and psychiatric symptoms such as depression and psychosis were found to have a significant impact on the number of annual medical inpatient and psychiatric outpatient visits (3). In addition, aggression has been shown to affect a number of factors that are probably associated with use of health care services, including injuries to self and others (12,13), as well as admissions to hospitals or nursing homes (14,15,16).
Little information exists about the impact of pain on use of health care services among patients with dementia. Approximately 30 percent of the direct annual cost of dementia may be associated with aggression, depression, and psychosis (17). Collectively, these psychosocial symptoms warrant the attention of clinicians and researchers, both for their impact on patients and their families and for their influence on the cost and use of health care services. Furthermore, because these psychosocial symptoms are treatable, it is possible to modify their impact.
The purpose of the prospective study reported here was to examine the relationships of pain, aggression, depression, and psychosis to use of health care services among patients with dementia. We hypothesized that depression, psychosis, aggression, and pain would be related to future use of services and that depression and psychosis would be most significantly related to use of psychiatric services as opposed to general medical services. Identification of comorbid symptoms that affect the use of health care services will be salient to targeting, preventing, or diffusing the escalation in patients' symptoms and subsequent need for services. Such a primary or secondary prevention strategy could improve the current approach to the treatment of depression, psychosis, aggression, and pain among patients with dementia.
Methods
The population of patients with dementia who were being seen at the Michael E. DeBakey Department of Veterans Affairs (VA) Medical Center in Houston, Texas, in 1999 was compiled by using the 1999 VA Outpatient Data Files stored at the Austin Automation Center. Patients with dementia were identified as those who were assigned an outpatient ICD-CM code for dementia (code 290.XX, 291.2, 292.82, 294.1, or 294.8). Patients who had died during 1999 and patients in long-term-care facilities were excluded. A representative sample was randomly selected from the list of 822 eligible patients, because the entire population of eligible patients could not be recruited because of time and financial constraints.
Thus 609 randomly selected patients (74 percent of the eligible population) were recruited to participate in the study. The families of the eligible patients received a postcard informing them that a research assistant from the medical center would be contacting them about participation in a dementia-related study. Potential participants were given a name, telephone number, and address they could use to inform the research team that they did not wish to participate or be contacted about participation. The names of those veterans, their caregivers, and their legal representatives (if different from the caregiver) who contacted the research assistant by the above-mentioned means were removed from the eligible list. The names of veterans whose postcard was returned because of inaccurate addresses in the system were also removed from the list. Caregivers were then contacted by telephone; the study was explained to them, and, if they were willing to participate, an interview was scheduled.
Over the seven-month recruitment period, we were able to contact 411 caregivers out of those initially recruited. After patients who were discovered to be ineligible for the study were excluded—for example, nursing home residents and those with no available caregiver—a total of 198 eligible patient-caregiver dyads were contacted. Of these, 52 refused to participate and 47 could not have interviews scheduled during the study period. Ninety-nine patient-caregiver dyads (50 percent) consented and completed assessments. All patients and caregivers were able to complete the 90-minute assessment. Approval for the study was obtained from the institutional review board of the Baylor College of Medicine.
Data collection consisted of a one-time interview with the veteran and the caregiver. A single trained interviewer conducted the interviews after receiving didactic and experiential training in interview and assessment administration from a psychologist with expertise in dementia. Informed consent was obtained from veterans who had the capacity to give consent; in the case of veterans who did not have this capacity, consent was obtained from the caregiver or legal representative, and assent was obtained from the veteran. As part of a larger assessment battery, the Dementia Rating Scale, the Cohen-Mansfield Agitation Inventory, the Pain Intensity Scale, the Hamilton Rating Scale for Depression, and the Neuropsychiatric Inventory were administered by a research assistant to the veteran and the caregiver.
The Mattis Dementia Rating Scale (DRS) is a standardized measure of general cognitive ability designed for use as a screen for cortical impairment, particularly of the degenerative type (18). The DRS has been shown to have adequate internal consistency, test-retest reliability, and convergent and predictive validity (19). We used a scoring formula developed by Monsch and colleagues (20) that yields 98 percent sensitivity and 92 percent specificity.
The Cohen-Mansfield Agitation Inventory (CMAI) is a valid, reliable scale that is commonly used to measure agitation among patients with dementia (21). This scale measures 29 agitation items by using Likert scales for frequency and disruptiveness. The CMAI scores are summed and result in a total score and three subscale scores: aggressive physical agitation, nonaggressive physical agitation, and verbal agitation. A total aggression subscale was devised by combining all the items on the physical aggression subscale and the two verbal aggression items contained in the verbal agitation subscale (22).
Pain was assessed with the Modified Philadelphia Geriatric Center Pain Intensity Scale (PGC-PIS), which has been shown to have adequate reliability and validity for use with patients with dementia (23). The scale consists of four items that assess the extent to which the patient is bothered by pain. For the purposes of this investigation, we used only one item pertaining to the patient's level of pain over the previous week, rated on a Likert scale of 1 to 6. Furthermore, the PGC-PIS was modified by pairing the questions with Roland and Morris' pain thermometer and response scale to improve the validity of the scale with severely impaired patients (24). Research has found that even persons with severe dementia can complete the pain thermometer presentation response scale (25).
The Hamilton Rating Scale for Depression (Ham-D) was used to assess depression (26). The Ham-D uses information from patients and their caregivers that results in a score ranging from 0 to 68 based on a 0-4 Likert scale of well-defined anchor points for 17 symptoms of depression. The Ham-D has been found to be valid for older adults with depression (27) and for patients with dementia and depression (28).
The Neuropsychiatric Inventory (NPI) delusions and hallucinations subdomains were used to assess psychosis (29). The NPI uses information from the primary caregiver of the patient with dementia to assess neuropsychiatric disturbances. The delusions subdomain consists of nine questions, and the hallucinations subdomain consists of seven questions. A 0-4 Likert response scale is used for both subdomains. The NPI has adequate content validity, and interrater reliability and test-retest reliability are also strong (29).
VA records were reviewed to assess use of health care services from the date of assessment to one year postassessment. Service use was collected from VA Inpatient and Outpatient File databases and included inpatient bed days (medical and psychiatric, excluding long-term-care days) and number of outpatient clinic visits (general medical visits and psychiatric visits). All the data for the study were collected during 2000 and 2001.
Internal consistency reliabilities for all measures except pain (because it was examined as only one item) were examined.All were above .77, which indicates generally good reliability.
The association between each of the treatable comorbid conditions—pain, aggression, depression, and psychosis—and subsequent use of health care services was examined with correlations and regression models. Separate regression models were constructed for each of three service use dependent variables (medical inpatient days per patient-year, medical outpatient visits per patient-year, and psychiatric outpatient visits per patient-year). Because of the rarity of psychiatric inpatient days of care, a model was not developed for this variable. Inpatient medical data represented a skewed distribution. Thus these data were collapsed into two categories (any bed days and no bed days), and a logistic model was developed. Linear regression models were developed for the outpatient utilization variables. Because it was hypothesized that all four variables would be associated with health service use, aggression, self-reported pain, depression, and psychosis were entered simultaneously rather than stepwise.
Results
The 99 patients who participated in the study were men. Their mean±SD age was 73.8±10.4 years, and they had a mean of 11.1±3.8 years of education. Seventy of the patients were married, 14 were divorced or separated, 12 were widowed, and three had never married. In terms of race, 43 patients were Caucasian, 40 were African American, and 15 were Hispanic. Compared with the 723 eligible patients who did not participate in the study, the study sample was on average slightly older (the average age of nonparticipants was 70.7 years) and had a higher proportion of African Americans and Hispanics.
The caregivers who participated in the study were related to the patients as follows: 68 were spouses, 16 were sons or daughters, eight were siblings, three were paid caregivers, two were friends, one was an in-law, and one was another relative. The caregivers were mostly women (N=95). Their mean±SD age was 63.5±13.5 years, and they had a mean of 11.8±3.9 years of education. Forty caregivers were Caucasian, 40 were African American, 17 were Hispanic, and two were of other racial backgrounds.
Table 1 presents the mean, standard deviation, and range for each type of health service use and the scores from the assessments of the severity of pain, aggression, depression, psychosis, and dementia. The DRS total scores indicate that the sample represented the entire spectrum of dementia severity: four patients (4 percent) were untestable because of severe dementia or agitation, 11 (11 percent) scored below 46 (indicating severe dementia), 39 (39 percent) scored from 47 to 102 (indicating moderate dementia), and 45 (46 percent) scored from 102 to 139 (indicating mild dementia) (30).
Pearson's correlations for all study variables are shown in Table 2. Pain was associated with outpatient psychiatry visits, outpatient medical visits, aggression, and depression. Depression was also associated with outpatient psychiatry visits, outpatient medical visits, pain, and aggression. Psychosis was associated with only outpatient psychiatry visits and aggression. Notably, although aggression was significantly correlated with pain, depression, and psychosis, it was not related to any of the service use variables.
The potential associations of pain, aggression, depression, and psychosis with use of inpatient medical services were explored through a logistic regression model, shown in Table 3. Only self-reported pain was associated with having an inpatient medical admission. Patients who reported their overall level of pain in the previous week as "very bad" were almost seven times as likely to have an inpatient medical stay in the next year as those who reported no pain.
Next we explored the associations between pain, aggression, depression, and psychosis and use of outpatient general medical and psychiatric services. Both the outpatient general medical service use model (R2=.18, adjusted R2=.12, F=2.81, df=7, 91, p=.01) and the outpatient psychiatric service use model (R2=.32, adjusted R2=.27, F=6.04, df=7, 91, p<.001) were significant.
Patients who reported their overall level of pain in the previous week as "quite bad" (β=.26, p<.05) or "very bad" (β=.29, p<.01) used more outpatient general medical services in the next year than those who reported no pain. Aggression, depression, and psychosis were not significant predictors of use of outpatient general medical services.
Depression explained significant variance in use of outpatient psychiatric services (β=.4, p<.01). Patients who reported their overall level of pain in the previous week as "quite bad" (β=.31, p<.01) used more outpatient psychiatric services in the next year than those who reported no pain. Psychosis and aggression were not significant predictors.
Discussion and conclusions
Although sizable efforts have been directed toward the development of effective treatments for the cognitive impairments of persons with dementia, less attention has been paid to treating the comorbid psychosocial symptoms that occur among more than 60 percent of these patients. This investigation prospectively examined the association between these symptoms and use of health care services and found that pain was significantly related to all three types of service use examined, that depression was associated only with use of outpatient psychiatric services, and that aggression and psychosis were not associated with use of any of the services examined.
Thus the main findings of this study suggest that patients with dementia who are experiencing pain may use more inpatient and outpatient services than those without pain and that patients with depression may visit outpatient mental health clinics more frequently than those without depression, which implies that depression may be diagnosed and treated among persons with dementia to some extent.These findings suggest that targeting depression and pain for assessment and treatment among patients with dementia might reduce unnecessary use of health services while also helping patients. Although aggression and psychosis were not associated with use of health care services in this study, further examination of these comorbid conditions should not be abandoned, particularly in light of this study's small sample. Furthermore, aggression was significantly correlated with pain, depression, and psychosis, which is consistent with the existing literature (4). Future research could explore the possibility that aggression is a behavioral expression of an underlying factor such as pain or depression.
Alternatively, given that the patients' primary caregivers may have been the individuals responsible for arranging and obtaining services as well as the principal means of transportation for the patients, it is possible that the caregivers who were under the greatest amount of burden were more likely to seek help for the patient.From this perspective, the associations we observed between pain and service use as well as between depression and service use may be a proxy for the association between caregiver burden and service use.
As might be anticipated, future research is needed to fully evaluate the research questions addressed by this study. This study did yield results worthy of further exploration, although the conclusions that can be drawn from this study are constrained by the study's limitations. The sample might not be a completely representative one, because some patients with either undiagnosed dementia or with dementia that was not recorded were probably seen in 1999.If the patients who could not be contacted, could not have an interview scheduled, or declined to participate in the study were significantly different from the patients who did participate, particularly in terms of dementia or treatable comorbid symptoms, this could also have had a significant impact on the results. Furthermore, the generalizability of this study may be limited as a result of its all-veteran, all-male sample.
Other limitations of the study include potential sources of information bias. Because the diagnosis of dementia was based on what was written in the patient's chart (although the DRS was used to help confirm the diagnosis), it is possible that a few of the study participants did not have dementia; variation in the severity of dementia could have also confounded the results. There may have been variability in the validity of the caregiver reports, because the caregivers in this study probably had varying degrees of exposure to symptoms and behaviors, given their variable relationships to the patients. In addition, the four comorbid conditions were assessed at a single point in time. It is possible that this time point was not representative of the patient's typical state, thus leading to misclassification. Furthermore, these comorbid conditions are likely to fluctuate over time, and the underlying assumption that they have some degree of constancy over the course of a year may not be valid.
Potential confounding factors include type and severity of dementia, comorbid general medical conditions, treatment status (for aggression, depression, psychosis, and pain), and use of health care services outside the VA system. Given the small sample studied and the multiple-comparisons issues that arise when a large number of variables are included in a model, we were unable to address these factors. The small sample also limited the power of the study.
On the basis of the findings of this study, it seems possible that targeting pain for clinical intervention would reduce use of health care services by patients with dementia. Previous research has shown that pain is highly prevalent among patients with dementia, yet pain is not often systematically addressed and is frequently underdiagnosed and undertreated by health care teams (31). Although research has validated the assessment of pain among persons with mild to moderate impairment, limited support exists for accurately assessing pain among persons with severe cognitive impairment (31,32). With deficits in language leading to limited capacity for self-report, patients with dementia have been noted to manifest symptoms of pain through behaviors that overlap widely with those indicative of other conditions, such as aggression (33,34). These behaviors are likely to affect the well-being of both the patient and the caregiver as well as health service use.
Although pain among nonverbal patients with dementia is poorly understood, research in this area may shed significant light on issues of behavioral and psychiatric disturbances in this population. Subsequently, the cause or causes of these difficulties could be appropriately addressed by health care professionals, which would probably have an impact on these patients' quality of life and future use of health care services.
Pain, aggression, depression, and psychosis are all symptoms that may be treated with pharmacologic and nonpharmacologic interventions (35). The study reported in this article is one step in exploring the importance of pain, aggression, depression, and psychosis, but much more research needs to be done to fully understand the effects of these symptoms among patients with dementia. A future means of determining the importance of these symptoms may be to empirically examine the impact that a reduction in one or more of these symptoms would have on persons with dementia, and subsequently, on health services use, overall costs, functioning, and quality of life.
Acknowledgments
This research was supported by the Houston Center for Quality of Care and Utilization Studies, Health Services Research and Development Service, Office of Research and Development, Department of Veterans Affairs.
Dr. Kunik, Dr. Cully, Dr. Snow, Dr. Souchek, and Dr. Ashton are affiliated with the Houston Center for Quality of Care and Utilization Studies, Health Services Research and Development Service, Michael E. DeBakey Veterans Affairs Medical Center (152), 2002 Holcombe, Houston, Texas 77030 (e-mail, [email protected]). Dr. Kunik, Dr. Cully, and Dr. Snow are also with the department of psychiatry and behavioral sciences and the department of medicine of Baylor College of Medicine in Houston. Dr. Souchek and Dr. Ashton are also with the department of medicine of Baylor College of Medicine. Dr. Sullivan is affiliated with the University of Arkansas for Medical Sciences.
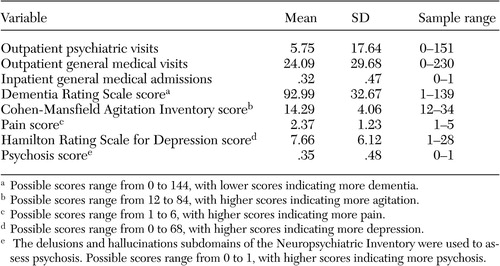 |
Table 1. Service use and symptoms of a sample of 99 veterans with dementia during a one-year period
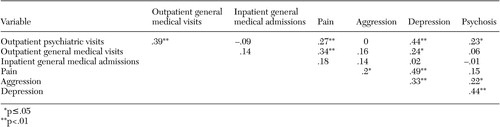 |
Table 2. Pearson's correlations of all variables in a study of comorbid conditions among veterans with dementia
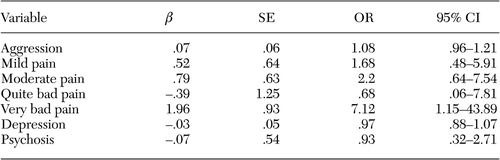 |
Table 3. Logistic regression model of use of inpatient medical services for a sample of 99 veterans with dementia
1. Richards KM, Shepherd MD, Crismon ML, et al: Medical services utilization and charge comparisons between elderly patients with and without Alzheimer's disease in a managed care organization. Clinical Therapeutics 22:775–791, 2000Crossref, Medline, Google Scholar
2. Gutterman EM, Markowitz JS, Lewis B, et al: Cost of Alzheimer's disease and related dementia in managed Medicare. Journal of the American Geriatrics Society 47:1065–1071, 1999Crossref, Medline, Google Scholar
3. Kunik ME, Snow AL, Molinari VA, et al: Health care utilization in dementia patients with psychiatric comorbidity. Gerontologist 43:86–91, 2003Crossref, Medline, Google Scholar
4. Kunik ME, Snow-Turek AL, Iqbal N, et al: Contribution of psychosis and depression to behavioral disturbances in geropsychiatric inpatients with dementia. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 54A:M157-M161, 1999Google Scholar
5. Lyketsos CG, Lopez O, Jones B, et al: Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA 288:1475–1483, 2002Crossref, Medline, Google Scholar
6. Rabins PV, Lyketsos CG, Steele C: Practical Dementia Care. New York, Oxford University Press, 1999Google Scholar
7. Kales HC, Blow FC, Copeland LA, et al: Health care utilization by older patients with coexisting dementia and depression. American Journal of Psychiatry 156:550–556, 1999Abstract, Google Scholar
8. Colenda CC, Hamer RM: Antecedents and interventions for aggressive behavior of patients at a geropsychiatric state hospital. Hospital and Community Psychiatry 42:287–292, 1991Abstract, Google Scholar
9. Steele C, Rovner B, Chase GA, et al: Psychiatric symptoms and nursing home placement of patients with Alzheimer's disease. American Journal of Psychiatry 147:1049–1051, 1990Link, Google Scholar
10. Miyamoto Y, Ito H, Otsuka T, et al: Caregiver burden in mobile and non-mobile demented patients: a comparative study. International Journal of Geriatric Psychiatry 17:765–773, 2002Crossref, Medline, Google Scholar
11. Gonzales-Salvador T, Lyketsos CG, Baker AS, et al: Quality of life of patients with dementia in long-term care. International Journal of Geriatric Psychiatry 15:181–189, 2000Crossref, Medline, Google Scholar
12. Lehmann LS, McCormick RA, Kizer KW: A survey of assaultive behavior in Veterans Health Administration facilities. Psychiatric Services 50:384–389, 1999Link, Google Scholar
13. Malone ML, Thompson L, Goodwin JS: Aggressive behaviors among the institutionalized elderly. Journal of the American Geriatrics Society 41:853–856, 1993Crossref, Medline, Google Scholar
14. Knopman DS, Berg JD, Thomas R, et al: Nursing home placement is related to dementia progression: experience from a clinical trial: Alzheimer's Disease Cooperative Study. Neurology 52:714–718, 1999Crossref, Medline, Google Scholar
15. Kopetz S, Steele CD, Brandt J, et al: Characteristics and outcomes of dementia residents in an assisted living facility. International Journal of Geriatric Psychiatry 15:586–593, 2000Crossref, Medline, Google Scholar
16. Patel V, Hope T: Aggressive behaviour in elderly people with dementia: a review. International Journal of Geriatric Psychiatry 8:457–472, 1993Crossref, Google Scholar
17. Beeri MS, Werner P, Davidson M, et al: The cost of behavioral and psychological symptoms of dementia (BPSD) in community dwelling Alzheimer's disease patients. International Journal of Geriatric Psychiatry 17:403–408, 2002Crossref, Medline, Google Scholar
18. Mattis S: Dementia Rating Scale: Professional Manual. Odessa, Fla, Psychological Assessment Resources, 1988Google Scholar
19. Smith GE, Ivnki RJ, Malec JF, et al: Psychometric properties of the Mattis Dementia Rating Scale. Assessment 1:123–132, 1994Crossref, Medline, Google Scholar
20. Monsch AU, Bondi MW, Salmon DP, et al: Clinical validity of the Mattis Dementia Rating Scale in detecting dementia of the Alzheimer type: a double cross-validation and application to a community-dwelling sample. Archives of Neurology 52:899–904, 1995Crossref, Medline, Google Scholar
21. Cohen-Mansfield J, Billing N: Agitated behaviors in the elderly: a conceptual review. Journal of the American Geriatrics Society 34:711–721, 1986Crossref, Medline, Google Scholar
22. Shahar K, Snow AL, Souchek J, et al: Cut point definition of agitation. Clinical Gerontologist 27:15–23, 2004Crossref, Google Scholar
23. Parmelee PA, Smith B, Katz IR: Pain complaints and cognitive status among elderly institution residents. Journal of the American Geriatrics Society 41:517–522, 1993Crossref, Medline, Google Scholar
24. Roland M, Morris R: A study of the natural history of low-back pain: II. development of guidelines for trials of treatment in primary care. Spine 8:145–150, 1983Crossref, Medline, Google Scholar
25. Weiner D, Peterson BL, Logue P, et al: Predictors of pain self-report in nursing home residents. Aging Clinical and Experimental Research 10:411–420, 1998Crossref, Google Scholar
26. Hamilton M: Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology 6:278–296, 1967Crossref, Medline, Google Scholar
27. Mottram P, Wilson K, Copeland J: Validation of the Hamilton Depression Rating Scale and Montgommery and Asberg Rating Scales in terms of AGECAT depression cases. International Journal of Geriatric Psychiatry 15:1113–1119, 2000Crossref, Medline, Google Scholar
28. Mulsant BH, Sweet R, Rifai AH, et al: The use of the Hamilton Rating Scale for Depression in elderly patients with cognitive impairment and physical illness. American Journal of Geriatric Psychiatry 2:220–228, 1994Crossref, Medline, Google Scholar
29. Cummings JL, Mega M, Gray K, et al: The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology 44:2308–2314, 1994Crossref, Medline, Google Scholar
30. Shay KA, Duke LW, Conboy T, et al: The clinical validity of the Mattis Dementia Rating Scale in staging Alzheimer's dementia. Journal of Geriatric Psychiatry and Neurology 4:18–25, 1991Crossref, Medline, Google Scholar
31. Huffman JC, Kunik ME: Assessment and understanding of pain in patients with dementia. Gerontologist 40:574–581, 2000Crossref, Medline, Google Scholar
32. Cohen-Mansfield J, Lipson S: Pain in cognitively impaired nursing home residents: how well are physicians diagnosing it? Journal of the American Geriatrics Society 50:1039–1044, 2002Google Scholar
33. Feldt KS, Warne MA, Ryden MB: Examining pain in aggressive cognitively impaired older adults. Journal of Gerontological Nursing 24:14–22, 1998Crossref, Medline, Google Scholar
34. Marzinski LR: The tragedy of dementia: clinically assessing pain in the confused, nonverbal elderly. Journal of Gerontological Nursing 17:25–28, 1991Crossref, Medline, Google Scholar
35. Kunik ME, Yudofsky SC, Silver JM, et al: Pharmacologic approach to management of agitation associated with dementia. Journal of Clinical Psychiatry 55(suppl):13–17, 1994Google Scholar



