The Cost of Schizophrenia Treatment in Taiwan
Abstract
The costs associated with mental illness in Taiwan have been the subject of discussion and concern in Taiwan's Bureau of National Health Insurance. The authors report the first estimates of these costs on the basis of national data for 52,432 patients treated in 1999. Total schizophrenia-related health care expenditure was estimated at $112.4 million, which constituted 1.2 percent of national health care expenditures that year. The cost per outpatient visit was $57, the cost per admission was $1,123, and the annual average direct cost of treating a person with schizophrenia was $2,144.
In recent years, the costs associated with mental illness have been the subject of much concern and discussion in Taiwan's Bureau of National Health Insurance (BNHI). Many debates have centered around the BNHI's regulations related to reimbursement restrictions for the prescribing of newer, more expensive antipsychotic drugs.
Taiwan's government-run national health insurance program, in which enrollment is mandatory, was implemented in 1995. By 1999, approximately 96 percent of Taiwan's population was covered by the program (1). The national health insurance program provides comprehensive coverage, including inpatient care, ambulatory care, laboratory tests, prescription drugs and certain nonprescription drugs, dental services, traditional Chinese medicine, day care for persons with mental illness, home care, and certain preventive services. A copayment is required for ambulatory care, inpatient care, and pharmaceuticals. However, services for catastrophic diseases, child delivery, and preventive health care as well as medical services offered in specific mountain areas or on offshore islands, for low-income households, and for veterans are exempt from the copayment. "Catastrophic diseases" include cancer, chronic mental illness, end-stage renal disease, and congenital illness.
In 1986 Taiwan established a regional psychiatric care network. Funds from this network subsidize both public and private hospitals in the establishment of psychiatric wards. By the end of 2000 a total of 213 psychiatric hospitals and clinics with 18,715 beds were in place, with the expectation that the goal of ten beds per 10,000 population would soon be reached.
As far as we know, no study has used national health insurance claims data to estimate the costs associated with treating schizophrenia in Taiwan. The emerging financial deficit of the national health insurance system has emphasized the importance of first obtaining cost estimates of proposed treatments in order to assist government health officials in resource allocation and decision making. Such cost estimates are especially critical in formulating reimbursement policies in regard to new medications.
Methods
Data on the use and costs of mental health services in 1999 were obtained from claims data from the BNHI. The fee-for-service payment system retains all the data relating to itemized medical orders and costs. Because schizophrenia is categorized as a catastrophic illness, data were available to include all patients with schizophrenia. However, in light of the huge amount of data collected nationwide, only samples of patients were included for other diseases.
The BNHI database contains each individual patient's scrambled identification number, age, sex, reimbursement scheme, admission date, discharge date, type of admission, and ICD-9-CM codes, including all itemized costs. Cost sharing is waived for all patients who have a catastrophic illness. The patients included in our study were defined as those with an ICD-9-CM diagnosis code of 295 and all its subgroups or with an outpatient A-code of 211. (The A-code is a simplified coding system for ambulatory care, used before the year 2000.)
Under this claims system, emergency and community rehabilitation health care expenditures are assigned to the outpatient section. Day care is covered in the hospitalization or inpatient section. Our first step was to estimate the total number of outpatient visits and admissions for patients with schizophrenia in one year. We then estimated the cost of total visits, total admissions, and total medications. The total cost for outpatients was then divided by the number of visits to determine the per-visit outpatient cost. The same procedure was followed for inpatients. The per-person cost for outpatients and inpatients as well as medication costs were calculated in the same way.
Results
A total of 52,432 patients (44.9 percent men, 54.7 percent women, and .4 percent whose sex was unknown) met the criteria for inclusion in the study. The mean±SD age of the participants was 39.7±12.6 years. Thirty-three percent of the patients were aged 30 to 39 years. Of the remaining patients, 26 percent were aged 40 to 49; 19 percent were aged 20 to 29; and 2 percent were aged 19 or younger. Only 8 percent of the participants were older than 60 years.
In 1999 the total national health care expenditure was U.S.$9.28 billion (1 U.S.$=31.40 New Taiwan dollars in 1999); 68 percent ($6.30 billion) was spent on outpatient care, and 32 percent ($2.98 billion) went toward inpatient care. The total amount spent on patients with schizophrenia was $112.4 million, or 1.2 percent of the total national health care expenditure. Of this $112.4 million, $84.5 million was accounted for by hospitalization and $27.9 million was accounted for by outpatient care.
In terms of service use, 46,226 patients had 487,227 outpatient visits and 16,312 patients had 75,277 admissions to hospitals in 1999. On average, each outpatient visit cost $57 and each inpatient admission cost $1,123. A total of 52,432 patients with a diagnosis of schizophrenia used the free national insurance medical service. The average total direct cost of treatment for schizophrenia per person per year was $2,144. This figure can be broken down as $604 per patient per year for outpatient care and $5,182 per patient per year for inpatient care.
Medication was found to be an important element of health care expenditures for schizophrenia. The cost of medication for schizophrenia represented 25.7 percent ($28.9 million) of the total direct schizophrenia health care costs ($112.4 million). Seventy-one percent of outpatient costs were for medication ($41 per visit), which was much higher than the corresponding figure in developed countries. In contrast, medication costs accounted for only 10.5 percent of total inpatient costs ($118 per admission). On average, the annual medication cost for one patient with schizophrenia was $550. The average for each outpatient and inpatient (not every patient was admitted) was $432 and $546, respectively.
Discussion
Schizophrenia is a costly disease. According to the 1991 Taiwan Psychiatric Epidemiological Project Study and data from the Epidemiologic Catchment Area survey, the prevalence of schizophrenia in Taiwan's population is approximately .24 to .3 percent. Our study showed that health care expenditures for schizophrenia account for around 1.2 percent of Taiwan's total health care expenses. This proportion compares with 2.5 percent in the United States (2), 1.6 percent in the United Kingdom (3), 2 percent in the Netherlands (4), and 2 percent in France (2). Inpatient costs represented 75.2 percent of total schizophrenia expenditures, compared with 32 percent of total national health expenditures for inpatient costs.
Our study found that drug expenditures account for a greater proportion of the total direct cost of treatment of schizophrenia in Taiwan compared with other developed countries. The total percentage of direct costs of schizophrenia incurred by drug therapy was 25.7 percent ($28.9 million) in Taiwan, compared with 4.3 percent in Canada (5), 2.3 percent in the United States (6), 5.4 percent in Belgium (7), and 4 percent in the United Kingdom (8). Although our data are more recent than those from these other countries, the cost of the newer, more expensive antipsychotic drugs still cannot explain this substantial difference. A possible explanation is the effects of low physician fees and hospital room costs in Taiwan.
Reimbursement for schizophrenia treatment has increasingly been the subject of debate in Taiwan. The BNHI set criteria restricting psychiatrists from prescribing the expensive new-generation antipsychotics to all patients, despite evidence that these agents are cost-effective, especially for lifelong treatment. We suspect that if the BNHI removes this drug therapy restriction, the high cost of admission and perhaps even total schizophrenia-related expenditures will be reduced.
The fact that we used the catastrophic illness database as our data source was associated with certain limitations. Although cost sharing for patients categorized as having a catastrophic illness is waived, some patients have not applied for catastrophic illness status because of the cultural stigma associated with schizophrenia. Thus the numbers of patients with schizophrenia and the national cost of the treatment of schizophrenia would have been higher in our study if this stigma did not exist.
Conclusions
This cost-of-illness study illustrated how resources are utilized for the treatment of disease and is the first attempt at using the national health insurance claims data to estimate the costs associated with treating schizophrenia in Taiwan. Our treatment cost estimates are at the lower end of the scale in estimating the true cost of this disease. We expect that future studies will investigate the benefits of treatment to both patients and caregivers.
Acknowledgments
This study was funded by grant NSC 89-2314-B-010-060 from the Taiwan National Science Council. The authors thank Hong-Shiow Yeh, M.D., and Chen-Jee Hong, M.D., from the department of psychiatry at the Taipei Veterans' General Hospital in Taipei, Taiwan, for their assistance during the data collection period.
The authors are affiliated with the Institute of Hospital and Health Care Administration at National Yang-Ming University, 155 Li-Nong Street, Section 2, Taipei, Taiwan 112 R.O.C. (e-mail, [email protected]).
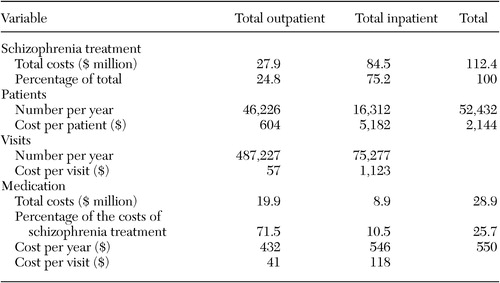 |
Table 1. Expenditures related to treating schizophrenia in Taiwan
1. Bureau of National Health Insurance: National Health Insurance Annual Statistical Report, 1999. Taipei, Taiwan, June 2000Google Scholar
2. Rupp A, Keith SJ: The costs of schizophrenia: assessing the burden. Psychiatric Clinics of North America 16:413–423, 1993Crossref, Medline, Google Scholar
3. Davies LM, Drummond MF: Economics and schizophrenia: the real cost. British Journal of Psychiatry 165(suppl 25):18–21, 1994Google Scholar
4. Evers SMAA, Ament JHA: Costs of schizophrenia in the Netherlands. Schizophrenia Bulletin 21:141–153, 1995Crossref, Medline, Google Scholar
5. Goeree R, O'Brien BJ, Goering P, et al: The economic burden of schizophrenia in Canada. Canadian Journal of Psychiatry 44:464–472, 1999Crossref, Medline, Google Scholar
6. Rice DP: The economic impact of schizophrenia. Journal of Clinical Psychiatry 60(suppl 1):4–6, 1999Medline, Google Scholar
7. De Hert MD, Thys E, Boydens J, et al: Health care expenditure on schizophrenia patients in Belgium. Schizophrenia Bulletin 24:519–527, 1998Crossref, Medline, Google Scholar
8. Knapp M: Costs of schizophrenia. British Journal of Psychiatry 171:509–518, 1997Crossref, Medline, Google Scholar



