Datapoints: Patients' Early Discontinuation of Antidepressant Prescriptions
The use of selective serotonin reuptake inhibitors (SSRIs) has increased in the past decade. This rapid growth in volume has led to widespread concern about the quality of antidepressant treatment in primary care (1). Previous studies indicated that rates of follow-up visits are worse for patients treated by primary care providers than for patients treated by psychiatrists, although follow-up was substandard in both types of settings (2,3).
Guidelines for the treatment of depression in primary care recommend a minimum of six to eight weeks of antidepressant treatment followed by six to nine months of continued treatment (4). We examined the prevalence of early discontinuation of SSRI treatment among patients seen by various medical specialties. Early discontinuation was defined as failure to refill a prescription for any antidepressant medication within 30 days of the end of the first SSRI prescription.
Data were obtained from Advance PCS. We examined medication discontinuation patterns among 26,888 adults who filled an SSRI prescription, had no record of taking any antidepressants in the previous year, and were eligible for AdvancePCS benefits for at least 180 days after they filled their first prescription for an SSRI.
Figure 1 shows that a majority of patients whose physician's speciality was known were given their first prescription by a primary care provider. Figure 2 shows that patients of psychiatrists were the least likely to discontinue the medication early, compared with patients of primary care providers and patients of other medical specialists (χ2=79.1, df=2, p<.001).
Rates of early discontinuation were above 30 percent in all three specialties, suggesting opportunities for performance improvement in each group.
Ms. Lewis is affiliated with the Vanderbilt University School of Medicine in Nashville. Dr. Marcus is with the University of Pennsylvania School of Social Work in Philadelphia. Dr. Olfson is with the College of Physicians and Surgeons at Columbia University in New York. Dr. Druss is with the Emory University School of Public Health in Atlanta. Dr. Pincus, who is coeditor of this column with Terri L. Tanielian, M.A., is with the department of psychiatry, University of Pittsburgh School of Medicine, 3811 O'Hara Street, Suite 230, Pittsburgh, Pennsylvania 15213 (e-mail, [email protected]) and the RAND-University of Pittsburgh Health Institute.
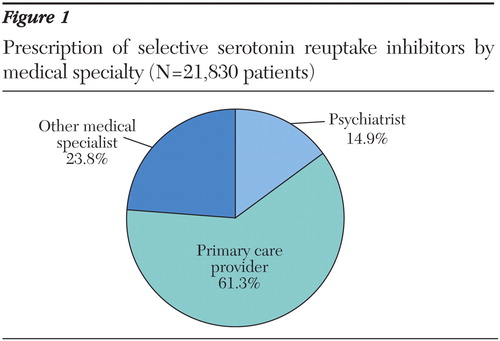
Figure 1. Prescription of selective serotonin reuptake inhibitors by medical specialty (N=21,830 patients)
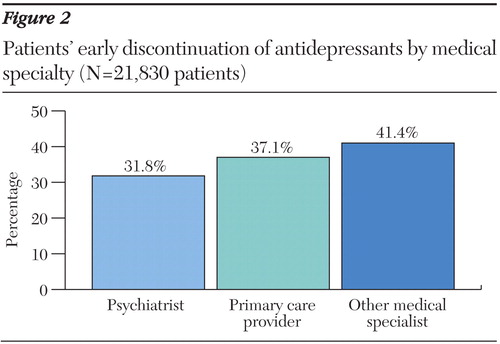
Figure 2. Patients' early discontinuation of antidepressants by medical specialty (N=21,830 patients)
1. Olfson M, Marcus SC, Druss BG, et al: National trends in the outpatient treatment of depression. JAMA 287:203–209, 2002Crossref, Medline, Google Scholar
2. Simon GE, Von Korff M, Rutter C, et al: Treatment process and outcomes for managed care patients receiving new antidepressant prescriptions from psychiatrists and primary care physicians. Archives of General Psychiatry 58:395–401, 2001Crossref, Medline, Google Scholar
3. Weilburg JB, O'Leary KM, Meigs JB, et al: Evaluation of the adequacy of outpatient antidepressant treatment. Psychiatric Services 54:1233–1239, 2003Link, Google Scholar
4. Depression in Primary Care, vol 2. Treatment of Major Depression. Clinical Practice Guideline, Number 5. Rockville, Md, US Department of Health and Human Services, Agency for Healthcare Research and Quality, 1993Google Scholar



