Perceived Coercion and Treatment Adherence in an Outpatient Commitment Program
Abstract
The authors investigated whether mental health inpatients' perceptions of coercion were associated with postdischarge treatment adherence. Patients eligible for New York's outpatient commitment program were interviewed and their perceptions of coercion measured during hospitalization and at one, five, and 11 months after discharge. Medication and clinical treatment adherence were measured at the three postdischarge interviews. Among the 117 participants who completed at least one follow-up interview, higher perceived coercion scores were correlated with greater self-reported adherence to clinical treatment at the one-month follow-up but not with participants' greater self-reported adherence at subsequent follow-ups or with providers' ratings of participants' adherence. Perceived coercion scores were positively correlated with participants' self-reported adherence to injected medications.
The role of coercion in the provision of mental health services is controversial (1,2). Although there are strongly held positions for and against coerced treatment, there is little empirical evidence about its effectiveness or its harmful effects (3).
Some studies have used patients' legal status as an "objective" measure of coercion. However, it has been shown that legal status fails to measure many forms of coercion as experienced by patients (4). Measures of perceived coercion, in contrast, obtain information about the subjective experiences of patients, specifically their perceptions of how much influence and control they have over their treatment decisions. Patients' perceptions of their own roles in decision making may have a greater influence than does their legal status on their reactions to hospitalization experiences.
Determinants of patients' perceptions of coercion have been studied, but few studies have investigated the relationships between perceived coercion and patient outcomes. Those that have done so have not shown consistent results. Two studies found few relationships between perceived coercion and outcomes. In a study of 825 patients, Rain and colleagues (5) found that perceived coercion at hospital admission did not affect subjects' adherence to outpatient treatment or to medication during the year following discharge. Similarly, Nicholson and colleagues (6) found that the duration of hospitalization, the perceived benefits of hospitalization, and functioning, as measured by the Global Assessment of Functioning (GAF) for patients who perceived high levels of coercion were similar to those for patients who perceived little or no coercion.
A study of 59 patients in Finland found that patients who felt coerced at hospital admission were less likely to take medications or use mental health services than were those who did not feel coerced (7). Patients who felt coerced were also less likely to show improvement in functioning or symptoms and more likely to feel negative about mental health staff and their own mental health outcomes. Although the small size of some of these differences and the small sample call these results into question, these data indicate the need for more research on the effects of perceived coercion.
In response to suggestions that high perceived coercion reduces future treatment adherence (8), this study investigated the relationships between perceived coercion—both at the time of hospital admission and after release into the community—and adherence to postdischarge treatment. Data examined are those from the study of the New York City Involuntary Outpatient Commitment Pilot Program (9), which includes a service provider interview that offers a more comprehensive assessment of treatment adherence than the self-report data used by most studies. These data also include measures of perceived coercion at each follow-up, an improvement on studies that focus only on perceptions of coercion at hospital admission.
Methods
The methods of the New York City Involuntary Outpatient Commitment Pilot Program, described in detail elsewhere (9), are summarized here. Between January 1996 and February 1998, patients at Bellevue Hospital in New York City who were eligible for the state's outpatient commitment pilot program were interviewed in the hospital and at one, five, and 11 months after discharge. Informed consent and institutional review board approval were obtained. Of the 172 patients interviewed, 55 percent were ultimately randomly assigned to outpatient commitment. Patients were asked about their perceptions of illness, treatment, and coercion and about social supports, quality of life, and recent life experiences. Functioning and symptoms were also assessed. Additional information about community-based treatment was collected at each of the three follow-ups.
During the follow-up period, each patient's case manager took part in an interview focusing on service use by patients in the study and on general program and service characteristics.
At the interview during hospitalization, patients were asked about coercion related to their current admission. At each follow-up, patients were asked about coercion related to their medication and to clinical treatment. Coercion was measured with the MacArthur Perceived Coercion Scale (10), administered to all patients enrolled in the study. The scale consists of five items: "I felt free to do what I wanted about [coming to the hospital/ taking medication/ getting treatment];" "I chose to [come into the hospital/ take medication/ get treatment];" "It was my idea to [come to the hospital/ take medication/ get treatment]; "I had a lot of control over whether I [went into the hospital/ took medication/ got treatment];" and "I had more influence than anyone else on whether I [came into the hospital/ took medication/ got treatment]." Each "true" was scored 0, and each "false" was scored 1. In the analyses, these scores were dichotomized into low coercion (0 to 2) and high coercion (3 to 5).
Adherence to postdischarge treatment was measured in several ways. First, respondents were asked what kind of treatment they received, how often they were supposed to attend treatment sessions, and how often they actually attended. A ratio of the number of sessions attended to the number of sessions prescribed was calculated, hereafter referred to as self-reported adherence. Patients who reported no prescribed treatments were excluded from analysis of this variable.
Second, respondents were asked, "How much of the time did you take the injections/shots as scheduled?" and "How much of the time did you take the oral medication as prescribed?" The response categories were "never or almost never" ( 0 to 25 percent of the time), "sometimes" (26 percent to 49 percent), "usually" (50 percent to 74 percent), and "always or almost always" (75 percent to 100 percent). These variables are referred to as "adherence to injected medication" and "adherence to oral medication."
Third, treatment providers were asked how compliant clients were with a number of prescribed services: supervision of living arrangements, case management, day programs, individual and group therapy, and alcohol and drug treatment. The response categories were the same as those for adherence to medication. Individual and group therapy received the lowest adherence rating recorded among all the services.
Results
Initial interviews and one-month follow-up interviews were conducted with 117 patients. Those with high perceived coercion scores at hospitalization were more likely to be female, to have more years of education, and to be white. No significant differences were found between the two groups in number of previous hospitalizations, marital status, age, GAF scores, and employment status.
Significant bivariate correlations were found between perceived coercion and some of the adherence measures at the one-month follow-up, as shown in Table 1. A positive correlation was found between perceived coercion (regarding hospitalization, first follow-up medication, and first follow-up treatment) and adherence to injected medication. Otherwise, none of the perceived coercion scores measured at the follow-ups were significantly related to adherence.
The significant correlations found at the first follow-up were not significant at the second or third follow-up. No significant relationships were found between perceived coercion and providers' ratings of the patients' treatment adherence.
Discussion and conclusions
In this study, perceived coercion at hospitalization was associated with increased self-reported treatment adherence at the first follow-up but not at subsequent follow-ups. We observed no relationship between patients' perceived coercion and adherence as reported by service providers. These ambiguous findings prevent us from concluding that there is a positive relationship between perceived coercion and treatment adherence. However, no evidence was found that higher levels of perceived coercion lead to subsequent nonadherence to mental health treatment, as has been suggested. Taken together, these findings were consistent with the MacArthur study's findings (5) that perceived coercion is incidental to treatment adherence.
Acknowledgments
The authors thank John Monahan, Ph.D., and Valerie Williams, M.A., M.S., for their assistance.
Ms. Rain, Dr. Steadman, and Ms. Robbins are affiliated with Policy Research Associates, Inc., in Delmar, New York. Send correspondence to Ms. Robbins at Policy Research Associates, Inc., 345 Delaware Avenue, Delmar, New York 12054 (e-mail, [email protected]).
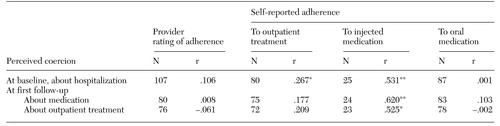 |
Table 1. Correlations between perceived coercion and adherence at first follow-up as rated by providers and reported by mental health inpatients
1. Dennis DL, Monahan J: Coercion and Aggressive Community Treatment: A New Frontier in Mental Health Law. New York, Plenum, 1996Google Scholar
2. Group for the Advancement of Psychiatry: Forced Into Treatment: The Role of Coercion in Clinical Practice. Washington, DC, American Psychiatric Press, 1994Google Scholar
3. Blanch A, Parrish J: Reports of Three Roundtable Discussions on Involuntary Interventions. Psychiatric Rehabilitation and Community Support Monograph 1. Rockville, Md, National Institute of Mental Health, Division of Applied and Services Research, 1990Google Scholar
4. Monahan J, Hoge S, Lidz C, et al: Coercion and commitment: understanding involuntary mental hospital admission. International Journal of Law and Psychiatry 18:249-263, 1995Crossref, Medline, Google Scholar
5. Rain SD, Williams VF, Robbins PC, et al: Perceived coercion at hospital admission and adherence to mental health treatment after discharge. Psychiatric Services 54:103-105, 2003Link, Google Scholar
6. Nicholson RA, Ekenstam C, Norwood S: Coercion and the outcome of psychiatric hospitalization. International Journal of Law and Psychiatry 19:201-217, 1996Crossref, Medline, Google Scholar
7. Kaltiala-Heino R, Laippala P, Salokangas RKR: Impact of coercion on treatment outcome. International Journal of Law and Psychiatry 20:311-322, 1997Crossref, Medline, Google Scholar
8. Parrish J: Involuntary use of interventions: pros and cons. Innovations and Research 2:15-22, 1993Google Scholar
9. Steadman HJ, Gounis K, Dennis D: Assessing the New York City involuntary outpatient commitment pilot program. Psychiatric Services 52:330-336, 2001Link, Google Scholar
10. Gardner W, Hoge S, Bennett N, et al: Two scales for measuring patients' perceptions of coercion during mental hospital admission. Behavioral Sciences and the Law 11:307-321, 1993Crossref, Medline, Google Scholar