Characteristics of Patients Presenting for Emergency Psychiatric Assessment at an English Hospital
Abstract
OBJECTIVE: The needs and characteristics of patients who are referred for psychiatric emergency services vary by the source of referral. Such differences have wider implications for the functioning of the mental health care system as a whole. This study compared three groups of patients in a two-month cohort of 189 patients who were referred for emergency psychiatric assessment at a hospital in England: those who were referred by general practitioners (family physicians), those who were receiving specialist services from community mental health teams, and those who arrived at the hospital from the broader community. METHODS: The three groups were compared on demographic characteristics, clinical and service use variables, risk to self or others, factors that contributed to the emergency presentation, and ratings on standardized scales of functioning. RESULTS: The patients who were receiving specialist services from community mental health teams had high rates of psychosis, often relapsed, and had a history of contact with a psychiatrist. These patients were the most likely to be admitted to the hospital after emergency assessment. The patients who had been referred by general practitioners tended to have fewer indicators of social problems and were more likely to be experiencing a new episode of mental illness. Their referral to the emergency department was most likely to be deemed inappropriate by emergency department clinicians. The patients who came from the broader community were more likely to be male and to exhibit self-harming behavior, substance misuse, and behavioral difficulties. CONCLUSIONS: The rate of emergency referral is one indicator of the functioning of the service system as a whole. Improvements to the system should include better access to community mental health team services and a greater capacity of the primary care system to manage mental health crises. Services need to be developed that are acceptable to male patients who are experiencing social and behavioral problems.
Over the past decade mental health services in England have developed according to national priorities and imperatives, which have sought to address the burgeoning problems of delivering mental health care in settings other than psychiatric hospitals. Community mental health teams deliver services by using a care program approach, which is built broadly on case management principles and targets resources toward people who have serious mental illnesses and complex social problems, particularly those who may pose a risk of harm to themselves or others. One of the consequences of systematic targeting is that key groups of people who have mental health needs but who do not fall within the designated priority groups may either be excluded from specialist services or receive relatively little specialist input.
One approach to exploring the functioning of complex mental health care systems is to study the point at which patient need or demand "breaks through" the designated systems of care and emergencies occur. In England, this point is usually when a patient presents or is referred for same-day psychiatric assessment. The nature and volume of such emergency demand provide some important indicators of how other components of the system of care delivery are functioning.
This study examined a cohort of patients who successively presented at the psychiatric emergency service in the district mental health service of Stockport, a district on the outer margins of the greater Manchester area in the northwest of England. Covering a population of some 300,000, Stockport has a wide range of population subgroups, including suburban areas, more impoverished urban areas, and semirural areas with more stable populations. Overall, it is close to the mean on the Jarman index of deprivation (1).
As is the case throughout England, Stockport has an extensive primary health care system; nearly everybody has a local general practitioner (family physician) who can make referrals for specialist care. Recent mental health policy has attempted to improve the confidence in and effectiveness of primary mental health care for people who are "less ill." In this context, emergency services are designed to be used for sudden and serious mental health problems. People who present for emergency services can be classified into three broad groups: those who are referred by general practitioners; those who go directly to a hospital accident and emergency clinic (emergency department), where they will be referred to an on-call psychiatrist without engaging the established service structure; and those who come via either route but who are already receiving specialist services from a community mental health team.
This study compared the characteristics of these three groups of patients. We hypothesized that the three groups would differ according to the parts of the mental health system from which they originated. First, we expected that patients who came directly from the broader community would have lower rates of serious mental illness and possibly be reacting to life crises or social adversity. Second, we expected that patients who had been referred by their general practitioner would experience new episodes of serious mental illness or pose substantial risks of self-harm or harm to others. Finally, we expected that the patients who had been in contact with community mental health teams would have an ongoing serious mental illness, possibly relapsing because of noncompliance with medication regimens. In this article we describe service referral for the three groups after emergency assessment and report the results of an 18-month follow-up of the cohort.
Methods
The study was approved by the local research ethics committee and was conducted according to the committee's requirements. Patient consent was not required. The study sample was a two-month continuous cohort of all persons who presented to or were referred for emergency psychiatric assessment in May and June of 1998. Patients were included if the referral information indicated that a same-day assessment took place, as opposed to an appointment for assessment at a later time, and referrals from all sources were included.
One schedule was developed specifically for the study and was derived from the "MARC-2" schedule that is used to collect information about individuals on the caseloads of community mental health teams (2) and has been extensively piloted. Information was recorded about the characteristics of each patient, features of the crisis situation that led to the referral to a psychiatrist, provisional diagnosis and risk factors, problems in a range of life domains, and action taken. Diagnoses were assigned according to the judgment of the assessing physician and in accordance with ICD classification categories. Risk and harm to self or others were also rated according to clinical judgment. Repeat use of the emergency service was identified from records.
Two further standardized instruments were used to assess mental health and functioning: the Health of the Nation Outcome Scales (HoNOS) (3) and the Global Assessment of Functioning (GAF) scale (4,5). Both sets of scales have been found to have acceptable reliability and validity (6,7). Although the HoNOS were developed for use with populations with severe mental disorders, the content of the scales was judged to be appropriate for use in a group that was likely to have a broader range of mental health and social problems. Total HoNOS scores as well as scores on four subscales—behavioral problems, impairment, symptoms, and social problems—were used in the analysis.
A total of 206 emergency assessments took place in the two months, and full data were collected for 189 of these (a response rate of 92 percent). If the two months of the study were typical, these numbers suggest that the psychiatric on-call system in Stockport is responding to approximately 1,200 referrals per calendar year.
All data were entered into SPSS and analyzed by using chi square and t tests as appropriate to levels of measurement and distribution of data. Discriminant-function analysis was used to identify variables that were most closely associated with the grouping variable "originating health care system."
Results
Of the 189 patients assessed, 48 were referred by general practitioners, 102 came directly to emergency services from the broader community, and 39 were in current contact with community mental health teams.
The sample included 103 men (54.5 percent) and 86 women (45.5 percent). The mean±SD age of the patients was 36.6±15.2 years (median=33.1, range=10.3 to 87.5). Only five patients were older than 75 years, and all except one were older than 16 years. A total of 182 patients (96 percent) were described as white British, which reflects the ethnic structure of the area. The overall characteristics associated with presentations to the emergency service have been described elsewhere (8).
Basic demographic and clinical characteristics of the three groups are summarized in Table 1. Predictably, the patients who were receiving services from a community mental health team had characteristics reflecting more severe illness: a significantly greater prevalence of psychotic illness, hospital admission in the previous two years, and contact with a psychiatrist. Patients who came directly from the broader community were more likely to be men and to have less severe psychosis than those in the other two groups. The patients who were referred by general practitioners had lower rates of use of accident and emergency clinics and lower rates of hospital admission.
Emergencies are not just a function of medical factors but can also be a manifestation of the referral habits and perceptions of patients, caregivers, and professionals. The referral and assessment characteristics of the study cohort are summarized in Table 2. In all three groups, a majority of referrals occurred during "routine" hours when other services could have provided an urgent response. The apparent seriousness of the emergency is reflected in the assessed risks of the three populations. The patients who came directly from the broader community were significantly more likely to be assessed as posing a moderate or severe risk of self-harm and were more likely to be seen during the daytime for an initial assessment of risk after an overdose. More patients were at risk of self-harm than of harm to others, and rates did not differ significantly between the three groups.
The patients who were referred by general practitioners were significantly less likely to be seen as being referred appropriately—that is, it was believed that more patients could have been managed within primary care settings. In terms of the outcomes of referral, significantly more of the patients who were referred from community mental health teams were admitted to the hospital; of those who were not admitted, most were referred back to the community mental health team. A number of patients who had been referred by general practitioners or who came directly from the broader community were also referred to the local community mental health team, where their needs would have been assessed but continuing service would depend on whether they met the team's criteria. A significantly greater proportion of the patients from the broader community were referred to their general practitioners.
Factors assessed by psychiatrists as making some contribution or a major contribution to the crisis that led to the patient's presentation at the emergency department are listed in Table 3. The patients who were referred by a general practitioner were significantly more likely to be experiencing the onset of a new episode of mental illness and to be compliant with medication regimens. The patients who had been in contact with a community mental health team were more likely to be experiencing relapse of psychosis and had a significantly higher rate of noncompliance. The patients from the broader community were significantly more likely to have experienced a major life event and to have a substance use problem. Levels of coping difficulties and chronic social difficulties were high in all three groups, which is perhaps not surprising for patients seen in an emergency service.
Differences between the three groups were also observed in standardized ratings of functioning. Table 4 provides patient data on total HoNOS scores and the four subscales; GAF scores are also compared.
The patients who were referred by a general practitioner had significantly lower levels of difficulty overall, particularly in the area of social problems. The patients who had been in contact with a community mental health team had higher levels of difficulty in relation to social problems as well as significantly lower GAF scores, indicative of poorer overall functioning. Those who came to the emergency department directly from the broader community had the highest overall HoNOS scores, which was accounted for by significantly higher scores on the behavior subscale. This subscale combines scores on three individual items: overactive, aggressive, or disruptive behavior; self-harm; and problem drinking or drug taking.
Discriminant function analysis was used to examine the extent to which patient characteristics discriminated between the various routes through mental health services to emergency assessment. The variables entered into the analysis were all those shown in Tables 1 through 4, except for owner-occupied housing and diagnosis of psychosis, which were excluded because of missing data. Outcome of assessment was included only as an indicator of whether hospital admission occurred.
Three variables emerged from the model as predicting the category of originating health care system: number of psychiatric admissions in the previous two years, relapse of severe mental illness having some or a major contribution to the crisis, and the HoNOS behavioral problems subscale score. These variables correctly classified 63.5 percent of cases.
Discussion and conclusions
The results of this study confirmed the hypothesis that the cohort of patients would have different characteristics depending on whether they had been referred by a general practitioner, had been in contact with a community mental health team, or had come to the emergency department independently from the wider community. The characteristics of the three groups of patients provoke further thought about what future services might need to be provided. There are also implications for the overall coordination of the health care systems and the pathways and filters by which the systems are linked (9).
The volume of referrals to emergency services is high enough to warrant investigation, although there is a dearth of comparable data. Schnyder and colleagues (10) recorded 3,611 consecutive emergencies in three years for a catchment are in Switzerland with a population of 400,000, which is not dissimilar to Stockport's projected emergency incidence of 1,200 per annum.
The patients in this study who were referred for assessment by general practitioners presented with intermediate levels of morbidity and fewer social problems. It seems that patients whose illness is in remission or who develop new episodes of illness come to the emergency department via this route. Perhaps because this group has better social support, some of them are presenting for attention early because of family concerns. However, it is not clear why referrals by general practitioners should be emergencies: most patients in our study came to the emergency department during working hours, and risks are not prominent, other than self-harm and health deterioration, which were features of all three groups.
Hillard (11) defines a psychiatric emergency in terms of "any behavior that cannot be dealt with as rapidly as needed by the ordinary mental health … system." This begs two questions: whether there are comprehensive care systems in place, and whether such systems could respond rapidly. Concern has been expressed about emergency departments' dealing with conditions that are amenable to management by a general practitioner (12,13). However, in the United Kingdom, community mental health teams deliberately and exclusively target serious chronic mental illness; it is expected that the remainder of the population will be dealt with by primary care (14).
Moreover, many of the concepts behind the development of community mental health teams derive from Australia and the United States, which do not have the comprehensive primary care structures of the United Kingdom. The rate of referral of patients to emergency mental health services by general practitioners in Stockport may reflect an absence of a satisfactory interface with local community mental health teams, leaving no other viable pathway for helping patients with burgeoning mental illness.
The group of patients in this study who had been in contact with a community mental health team reflects well the targeting of the local community mental health teams: This group had high levels of identified mental illness and other markers of morbidity. There was a clear pattern of relapse, in some cases leading to hospitalization.
Despite emergency presentation, the most prominent concern in regard to the group of patients who had been in contact with a community mental health team was deterioration in health rather than imminent risk to self or others. Also, these patients presented during routine hours. Taking Hillard's (11) perspective on emergencies, services were in place, but establishing a rapid effective response was apparently difficult. In the case of Stockport, the primary feature of the emergency department is its ability to provide the opinion of a medical specialist. Thus the provision of medical input to community mental health teams and the development of extended hours and assertive outreach capability should be priorities.
The largest group of patients who were seen in the emergency department were patients who came directly from the wider community without having been referred through an intervening health care system. This group was predominantly male and was characterized by high levels of self-harm, substance misuse, and behavioral difficulties but low levels of psychotic illness. The existence of a substantial patient population with few social skills and supports and a tendency to present to emergency services has been reported and discussed by several authors (15,16). However, it is important to note that the emergency department plays a larger role in the North American health care system than in the UK system, in which a large proportion of the population is covered by primary care and accident and emergency clinics serve as default sources of help.
In the face of life challenges, some individuals, rather than using routine services, attend accident and emergency clinics. Others end up in emergency departments after an overdose of medications or other drugs. These behavior patterns represent a shift in the way communities relate to health care systems. The role of emergency services in mental health care and other health domains is a much-discussed topic (13,17). The assumption that patients with psychiatric disorders are referred to specialist services by general practitioners (9) has become less tenable, and there are implications for expanding awareness of mental health care issues to a broader front. Interestingly, in this study the patients who were self-referred were more likely than others to be referred to the primary care system by emergency service clinicians, which suggests that specialists viewed primary care as the most appropriate source of help, whereas the patients themselves bypassed this service.
Despite its limitations, this study has suggested three distinct populations with different service needs that go beyond routine services. By studying the breakdown of routine health care systems, it has been possible to raise questions about those systems, which may in turn inform future service development.
Acknowledgment
This study was funded by the Stockport Social Services Department.
Dr. Spurrell is consultant psychiatrist at Stepping Hill Hospital in Stockport, United Kingdom. Ms. Hatfield is director and Ms. Perry is research associate in the Mental Health Social Work Research Unit at the University of Manchester. Send correspondence to Ms. Hatfield at the Mental Health Social Work Research Unit, Department of Psychiatry, 12th Floor, Mathematics Building, University of Manchester, Oxford Road, Manchester M13 9PL, United Kingdom (e-mail, [email protected]).
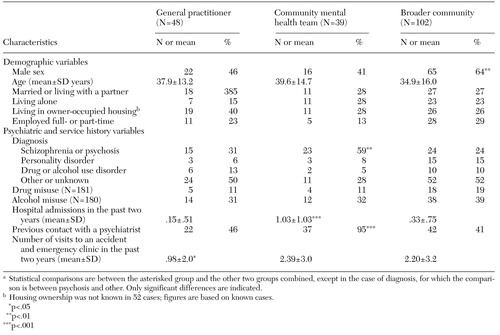 |
Table 1. Characteristics of 189 users of emergency services, by originating health care systema
a Statistical comparisons are between the asterisked group and the other two groups combined, except in the case of diagnosis, for which the comparison is between psychosis and other. Only significant differences are indicated.
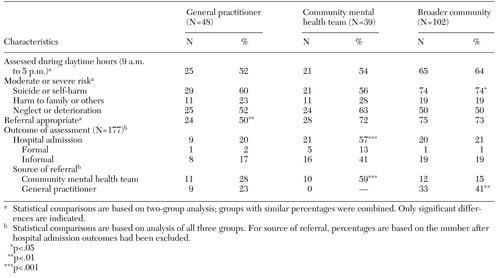 |
Table 2. Referral and assessment characteristics of 189 users of emergency services, by originating health care system
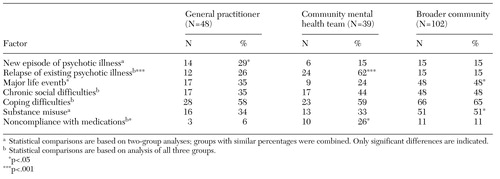 |
Table 3. Factors assessed by a psychiatrist as making some or a major contribution to the crisis that led to emergency presentation among 189 patients, by originating health care system
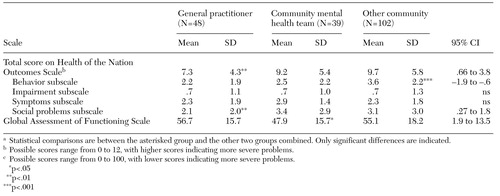 |
Table 4. Scores on measures of functioning and impairment among 189 patients who presented for emergency services, by originating health systema
a Statistical comparisons are between the asterisked group and the other two groups combined. Only significant differences are indicated.
1. Huxley P, Reilly S, Mohamad H, et al: Severe mental illness: comparing CPNs' and social workers' inputs. Mental Health Nursing 18(3):14-17, 1998Google Scholar
2. Jarman B: Identification of under-privileged areas. British Medical Journal 286:1705-1709, 1983Crossref, Medline, Google Scholar
3. Wing JK, Beevor AS, Curtis RH, et al: Health of the Nation Outcome Scales: research and development. British Journal of Psychiatry 172:11-18, 1998Crossref, Medline, Google Scholar
4. Phelan M, Wykes T, Goldman H: Global function scales. Social Psychiatry and Psychiatric Epidemiology 29:205-211, 1994Crossref, Medline, Google Scholar
5. Jones SH, Thornicroft G, Coffey M, et al: A brief mental health outcome scale: reliability and validity of the Global Assessment of Functioning (GAF). British Journal of Psychiatry 166:654-659, 1995Crossref, Medline, Google Scholar
6. Bebbington P, Brugha T, Hill T, et al: Validation of the Health of the Nation Outcome Scales. British Journal of Psychiatry 174:389-394, 1999Crossref, Medline, Google Scholar
7. Orrell M, Yard P, Handysides J, et al: Validity and reliability of the Health of the Nation Outcome Scales in psychiatric patients in the community. British Journal of Psychiatry 174:409-412, 1999Crossref, Medline, Google Scholar
8. Hatfield B, Spurrell M, Perry A: Emergency referrals to an acute psychiatric service: demographic, clinical, and social characteristics and comparisons with those receiving continuing services. Journal of Mental Health 9:305-317, 2000Crossref, Google Scholar
9. Goldberg D, Huxley P: Mental Illness in the Community: The Pathway to Psychiatric Care. London, Tavistock, 1980Google Scholar
10. Schynder U, Klaghofer R, Beddeberg C: Characteristics of psychiatric emergencies and the choice of intervention strategies. Acta Psychiatrica Scandinavica 99:179-187, 1999Crossref, Medline, Google Scholar
11. Hillard JR: The past and future of psychiatric emergency services in the US. Hospital and Community Psychiatry 45:541-543, 1994Abstract, Google Scholar
12. Hobday PJ: Patients attending casualty from one group practice. Practitioner 232:552-555, 1988Medline, Google Scholar
13. Dale J: Primary care: the old bugbear of accident and emergency services. British Journal of General Practice 42:90-91, 1992Medline, Google Scholar
14. Health of the Nation: Key Area Handbook Mental Illness, 2nd ed. London, UK Department of Health, 1994Google Scholar
15. Katschnig H, Koniecza T: Innovative approaches to the delivery of emergency services in Europe, in Mental Health Care Delivery: Innovations, Impediments, and Innovation. Edited by Marks IM, Scott RA. Cambridge, United Kingdom, Cambridge University Press, 1990Google Scholar
16. Johnson S, Baderman H: Psychiatric emergencies in the casualty department, in Emergency Mental Health Services in the Community. Edited by Phelan M, Strathdee G, Thornicroft G. Cambridge, United Kingdom, Cambridge University Press, 1995Google Scholar
17. Calling all gatekeepers: this is an emergency [editorial]. Lancet 343:305-306, 1994Crossref, Medline, Google Scholar



