Patients' Concerns About and Perceptions of Electronic Psychiatric Records
Abstract
This study assessed concerns about and perceptions of electronic psychiatric records in a university psychiatric adult outpatient clinic. Forty-one patients who refused to have their psychiatric records transferred to the electronic record system were compared with 39 patients who agreed to an electronic record. Regardless of whether or not they refused to have their information transferred to an electronic record, a majority of patients reported numerous concerns about electronic records, such as concerns about unauthorized access to their records by parties within the university health care system. Patients' concerns may affect patient disclosure and other help-seeking behavior and therefore must be addressed by clinicians and health care systems.
Electronic medical records allow broader dissemination of medical information, which improves coordination of care between multiple providers and geographic locations and simplifies tracking of patient outcomes for the purposes of improving health care delivery. However, there is potential for risks such as confidentiality breaches and differential care by other medical providers based on psychiatric information.
The implementation of the Health Insurance Portability and Accountability Act (HIPAA) had a significant impact on patients' control of information in the electronic record (1,2). Although little systematic information about patients' opinions of electronic medical records has been gathered, there is reason to believe that people are concerned about the confidentiality of computer-based medical records (3,4), that these concerns may affect care seeking and disclosure (5), and that lack of complete information about computerized systems and information contained in these systems is common (6). Understanding patient characteristics and perspectives that influence comfort with electronic records will help inform administrative and system decisions, such as identification of areas that should be targeted for patient and staff education, and will heighten awareness of the ways that patient perceptions of confidentiality affect patient disclosure and other behaviors related to care.
In this paper we present data obtained from a sample of psychiatric outpatients who were surveyed about their concerns about electronic psychiatric records. Using a cross-sectional survey design, we compared a group of active patients who refused to have their records transferred to an electronic record with a control group of patients who agreed to electronic records.
Methods
As part of standard practice at the time of the study, all outpatients who were being seen in the University of Michigan Health System department of psychiatry received a letter from their provider detailing the procedures for the transfer of patient records to the electronic system. Overall, 5 percent of the patients (132 of 2,519 patients from May to December 1999) refused to have their information transferred to the electronic record. At the time of the study, 54 of these patients who refused the transfer remained in treatment and could be contacted about participation in the study.
All outpatients who were being seen in the department of psychiatry—that is, active patients at the time of this study—who refused to have their record transferred to the electronic system were eligible to participate in the study. Among these active patients, 41 (76 percent) agreed to complete the survey. These patients were contacted during a regular outpatient visit and were asked to complete a brief written survey. The control group of patients who agreed to an electronic record was randomly selected from patients of the clinicians who had patients in the group who refused to have an electronic record. A total of 39 of these patients completed the survey; two refused to participate in the study. The study participants were representative of the ethnic distribution and demographic mix of outpatients being seen in the department (73 percent female, 97 percent Caucasian). All study procedures were approved by the University of Michigan Medical School's institutional review board.
The patient survey included items inquiring about specific concerns about the electronic record system. The survey was constructed and modified by a team of five psychiatry faculty on the basis of anecdotal reports of patients' concerns. The final survey consisted of 22 items, for which the completion time was ten to 15 minutes. The survey assessed issues that may have influenced patients' decisions about whether to have their information transferred to the electronic psychiatric record. All patients were asked to rate, on a 5-point Likert scale, the extent to which each concern influenced their decision to agree or refuse to have their information transferred to the electronic record. The survey also assessed demographic information, specific concerns about confidentiality, and opinions about psychiatric information. Each of these items was rated dichotomously (yes or no).
Results
For all analyses, data from the group of patients who refused to have an electronic record were compared with those from the group who did not refuse (the control group). The two groups were similar in age, sex, partner status, and self-reported diagnosis. However, the patients who refused to have an electronic record were significantly more likely than the patients in the control group to have a four-year college degree or a more advanced degree.
Ratings of the extent to which a list of possible concerns influenced patients' decision to participate in the electronic record are summarized in Table 1. As can be seen in the table, a majority of patients, regardless of whether or not they refused to have an electronic record, endorsed specific concerns about the use of electronic records. For example, close to 90 percent of participants in both groups reported concerns about unauthorized access of their records by persons outside the hospital system. A minority in each group indicated concerns about receiving poorer care from their primary care physician as a result of the use of the electronic record.
Significantly more of the patients who refused to have an electronic record reported concerns about unauthorized access to their records by parties within the university health care system (t=10.2, df=76, p=.002), concerns about the security of the electronic record system (t=8.3, df=76, p=.005), concerns about the stigma of having a psychiatric illness (t=8.5, df=76, p=.005), and concerns about the possible impact of the electronic psychiatric record on their jobs (t=5, df=76, p=.03).
Patients who refused to have an electronic record reported significantly more often that they would transfer their care elsewhere if electronic psychiatric records became mandatory (31 patients, or 76 percent, compared with six patients, or 16 percent). Patients who agreed to an electronic record were significantly more likely to report a belief that the use of electronic psychiatric records is likely to lead to better coordination of care.
Discussion and conclusions
The advantages of switching to an electronic psychiatric record system are potentially very great. However, it remains to be seen whether and how this transformation will affect patients' behavior and the doctor-patient relationship. A majority of the patients we surveyed, regardless of whether or not they agreed to have an electronic record, reported numerous specific concerns about the use of electronic records. The primary concerns were concerns about unauthorized access to records, inappropriate use of information contained in the record, stigmatization, and the security of the electronic record system.
Patients who had advanced academic degrees were more likely to refuse to have an electronic psychiatric record, possibly reflecting more awareness of the vulnerability of such systems. Otherwise, no demographic differences were found between the patients who refused to have an electronic record and those who did not. Both groups of patients reported fears of both unauthorized access within the health system and a possible adverse impact on their job. Both groups were very likely to report doubts about the security of the electronic record system and to report that they might transfer out of the health care system if electronic records were mandatory.
The reported concerns and feelings about the sensitivity of the information indicate that even apparently cooperative patients may feel constrained in their use of psychiatric services or in the amount of information they share with their doctor. The patients' willingness to consider transferring out of the health care system suggests that many patients will either not seek care for a sensitive problem or will seek care outside of the system, potentially undoing the potential benefits of coordination of care. Both these hypotheses need to be systematically examined in future studies.
The findings of this study suggest that providers and health systems that implement electronic records should focus on educating patients and staff about issues pertaining to electronic medical records. Clinics and institutions that move to an electronic record system should attend to patient concerns by creating an open atmosphere in which concerns can be expressed and addressed.
Limitations of the study include reliance on self-report and lack of data on the impact of electronic records on health care behaviors. In addition, we had no information about the 24 percent of patients who refused to participate in our study. Despite these limitations, the study clearly points to widely held perceptions and concerns that may well shape patient health care behavior in the inevitable move to electronic records.
The authors are affiliated with the department of psychiatry of the University of Michigan, 400 East Eisenhower Parkway, Suite 2A, Ann Arbor, Michigan 48108 (e-mail, [email protected]).
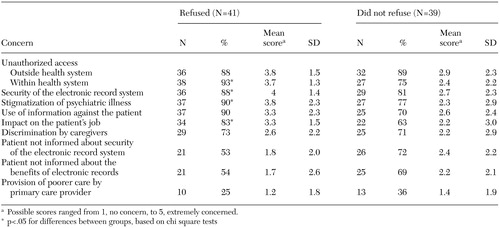 |
Table 1. Specific concerns reported by patients who refused to have an electronic record and a control group of patients who did not refuse and scores indicating the extent of concern
1. Appelbaum PS: A "health information infrastructure" and the threat to confidentiality of health records. Psychiatric Services 49:27–30, 1998Link, Google Scholar
2. Appelbaum PS: Threats to the confidentiality of medical records: no place to hide. JAMA 283:795–797, 2000Crossref, Medline, Google Scholar
3. Ornstein S, Bearden A: Patient perspectives on computer-based medical records. Journal of Family Practice 38:606–610, 1994Medline, Google Scholar
4. Pennbridge J, Moya R, Rodrigues L: Questionnaire survey of California consumers' use and rating of sources of health care information including the internet. Western Journal of Medicine 171:302–305, 1999Medline, Google Scholar
5. Cheng TL, Savageau JA, Sattler AL, et al: Confidentiality in health care: a survey of knowledge, perceptions, and attitudes among high school students. JAMA 269:1404–1407, 1993Crossref, Medline, Google Scholar
6. Kinzie JD, Holmes JL, Arent J: Patients' release of medical records: involuntary, uninformed consent? Hospital and Community Psychiatry 36:843–847, 1985Google Scholar