Mental Health Care for Latinos: Inequalities in Use of Specialty Mental Health Services Among Latinos, African Americans, and Non-Latino Whites
Abstract
OBJECTIVE: The authors investigated whether there are disparities in the rates of specialty mental health care for Latinos and African Americans compared with non-Latino whites in the United States. METHODS: Data were analyzed from the 1990-1992 National Comorbidity Survey, which surveyed a probability sample of 8,098 English-speaking respondents aged 15 to 54 years. Respondents self-identified their race or ethnicity, yielding a sample of 695 Latinos, 987 African Americans, and 6,026 non-Latino whites. Data on demographic characteristics, insurance status, psychiatric morbidity, whether the respondent lived in an urban or a rural area, geographic location, income, and use of mental health services were determined for each ethnic or racial group. Logistic regression analyses were used to examine the associations between ethnic or racial group and use of specialty services, with relevant covariates adjusted for. RESULTS: Significant differences between ethnic groups were found in demographic characteristics, geographic location, zone of residence, insurance status, income, wealth, and use of mental health services. The results indicated that poor Latinos (family income of less than $15,000) have lower access to specialty care than poor non-Latino whites. African Americans who were not classified as poor were less likely to receive specialty care than their white counterparts, even after adjustment for demographic characteristics, insurance status, and psychiatric morbidity. CONCLUSIONS: To understand ethnic or racial disparities in specialty care, the effects of ethnicity or race should be analyzed in combination with variables related to poverty status and environmental context. Further research needs to address the complex construct of social position in order to bridge the gap in unmet need in specialty care.
Demand for proper health care has spawned a greater awareness of the role of ethnicity or race in the provision of appropriate mental health services for minority populations (1). Until recently, research on the provision of mental health services did not consider race or ethnicity as a major factor (2). However, when investigators examined the use of and expenditures for mental health services by Medicaid beneficiaries in New York, they found marked differences between ethnic groups (3). These data, as well as the findings of other investigators (4), have raised concerns about potential disparities in mental health care among racial and ethnic minorities.
Not all differences in rates of service use constitute disparities. Adjustment for "legitimate" sources of difference—such as need—is necessary for identifying inequities (5). Further adjustment for the many factors that affect use, such as socioeconomic status, is necessary for identifying the inequity due to race or ethnicity (6). The U.S. Surgeon General (7) recently called attention to the limited understanding of cultural factors that may contribute to an inadequate allocation of and access to resources for appropriate treatment. The study reported here used data from the National Comorbidity Survey (NCS) (8)—a nationwide survey designed to provide information on the prevalence of DSM-III-R disorders and the use of mental health services—to investigate whether there are inequalities in the rates of specialty care for Latinos and African Americans compared with non-Latino whites.
Some studies have indicated that Latinos experience great difficulties in obtaining adequate access to mental health services (9,10,11) and are underrepresented in mental health care settings (12,13,14,15,16,17). Other studies have shown comparable levels of use of mental health services between Latinos and non-Latinos (18,19). Possible methodologic explanations for these divergent results are differences in the measures used to assess psychiatric disorders and service use (20), response bias due to instrumentation (21,22), differences in geographic locations, and differences in measures of access to mental health services. The differences have also been attributed to the selection of covariates or to uncontrolled factors such as level of psychiatric morbidity (23), insurance coverage (24), and socioeconomic status.
We explored multiple factors that may contribute to ethnic or racial disparities in the use of mental health services. What role does ethnicity or race play compared with other components of social position, such as income and wealth or the environmental context, in explaining differential rates of specialty care use? Substantial evidence indicates that social position plays a major role in psychiatric disorders (25) and service use (26,27). Similarly, the environmental context is crucial in the variations in health and access to health care (28). These factors can help clarify links to ethnic or racial differences in service use, illustrated in Table 1. Therefore, we first compared estimated rates of use of specialty care services by ethnic and racial groups, adjusting for psychiatric disorder, insurance status, and socioeconomic status. Second, we evaluated the association between ethnic and racial group and differential rates of specialty care, stratifying by poverty status and by geographic location.
Methods
Study population and data
We used data from the 1990-1992 NCS (29), based on a probability sample of 8,098 English-speaking respondents in the United States aged 15 to 54 years. The study methods have been described previously (30,31,32). Although the NCS was not designed to provide an understanding of racial and ethnic disparities in the use of mental health services, it does provide comparative data for African Americans, Latinos, and non-Latino whites, all based on the same methods and research design.
Ethnic and racial identification
Respondents were asked to self-identify whether they were of Spanish or Latino descent and, if so, to indicate their nationality—Mexican, Mexican American, Chicano, Puerto Rican, Cuban, or other Spanish. Persons who identified themselves as being of Latino descent, independent of how they reported their race, were categorized as Latino (N=695). Overall, there were 432 Mexican Americans, 67 Puerto Ricans, 30 Cubans, and 166 other Latinos. Nonetheless, the small size of the Latino sample prevented us from conducting subgroup analyses. Respondents who did not identify themselves as being of Spanish or Latino descent were asked to identify themselves as white, black, American Indian, Asian, or other. Respondents who classified themselves as non-Latino white (N=6,026) or African American (N=987) were also included in the analysis.
Use of outpatient mental health services
Any use of outpatient mental health services in the previous year was defined as speaking to a professional about symptoms or disorders in the 12-month period before the interview (32). Treatment for a mental health problem by a physician other than a psychiatrist or treatment in a hospital emergency department or a doctor's private office was defined as general medical care. Specialty mental health care was defined as treatment by a psychiatrist, a psychologist, or a psychotherapist or treatment by any professional in a specialty mental health setting. Mental health care provided in a social service agency or department was coded as human service- sector care.
Social position, geographic location, and zone of residence
No consensus exists about how social position is best operationalized, but—however defined—this variable shows a robust relationship to psychiatric illness and service use (26,33,34). Social position was based on the respondent's estimate of household income from all sources before income tax deductions and wealth. Income was coded in four categories: $0 to $14,999, $15,000 to $34,999, $35,000 to $69,999, and $70,000 or more. Wealth was defined as the total funds of the respondent and his or her spouse or partner in checking and saving accounts, stocks, bonds, real estate, and house value net of any mortgage. Wealth was coded in three categories: less than $10,000, $10,000 to $99,000, and $100,000 or more. Poverty status was determined by dividing the family income data into poor (less than $15,000) and nonpoor ($15,000 or more). This categorization is based on Census Bureau income thresholds for 1990-1992. The poverty threshold for a four-person household was $13,400 to $14,400 (35); therefore, a threshold of less than $15,000 was used to designate poverty in our sample. Geographic location was coded as Northeast, South, West, and Midwest. Zone of residence was coded as urban or rural.
Demographic characteristics, insurance status, and psychiatric morbidity
Several demographic variables that have previously been found to be correlated with use of mental health services (36,37) were included as controls: sex, age, marital status, education, and insurance status. Sex was a dichotomous variable, with female as the reference category. Age was included as either a categorical variable (15 to 24 years, 25 to 34 years, 35 to 44 years, and 45 years or older) or as a continuous variable. Marital status was categorized as disrupted marriage (for example, separated, divorced, or widowed), never married, or married. Education was included as a continuous variable of the number of years of education or as a categorical variable (less than high school, high school, 13 to 15 years, and 16 years or more). Insurance was represented by two dichotomous variables: private insurance other than Medicaid and Medicaid, with no insurance as the reference category.
Previous research has established a strong association between the presence and severity of psychiatric morbidity and the use of mental health services (17). Therefore, we examined how differences in psychiatric morbidity might influence ethnic and racial differences in service use. Psychiatric morbidity was constructed as a four-category variable: two or more diagnoses in the previous year, one diagnosis in the previous year, any lifetime diagnosis, and no lifetime diagnosis. Diagnoses of mental disorders were determined by the Composite International Diagnostic Interview (CIDI) (38) using DSM-III-R criteria. The CIDI generates diagnoses of mood disorders, anxiety disorders, and substance use disorders with good reliability and validity (39). Disability was measured by asking respondents to report the number of days in the previous 30 days that they either cut down on or were unable to perform usual activities because of mental illness. Disability was recorded for respondents who reported one or more such days.
Analyses
Comparisons of the distributions of demographic characteristics, insurance status, psychiatric morbidity, zone of residence, geographic location, income, and use of mental health services across ethnic groups were made by using chi square tests. Differences in service use were apparent only in the use of specialty services; therefore, all subsequent analyses used specialty care as the dependent variable. Logistic regression analyses examined the positive correlations between ethnic or racial group and use of specialty care with adjustment for demographic and insurance variables.
A second set of analyses was conducted to assess the relationship between ethnic or racial group and use of specialty care after adjustment for social position, geographic location, and zone of residence. To better understand the association between ethnicity and the use of specialty care, a third logistic regression was computed that added to the model two additional covariates: psychiatric illness and disability. We also conducted separate logistic regressions stratifying the sample by poverty status and by geographic location. The standard errors of the estimates and the logistic regression coefficients were calculated by using SUDAAN (40) to adjust for clustering and nonresponse in the sample design.
Results
Differences by ethnic or racial group
As shown in Table 2, significant differences were observed between the three ethnic or racial groups. Compared with non-Latino whites, Latinos were younger and less educated and were more likely to have never been married, to have no insurance, and to live in the South or the West. The proportion of Latinos reporting an annual household income of less than $15,000 was 28.4 percent, similar to that for African Americans. The three groups showed marked differences in aggregate measures of psychiatric morbidity. Latinos were more likely to have two or more previous-year psychiatric disorders than non-Latino whites and African Americans. The rate of disability was significantly lower among African Americans than in the other two groups. Significant differences were noted in the proportional distributions of use of any specialty care.
Rates of specialty care after adjustment for psychiatric morbidity
When we restricted the analysis to respondents who reported the presence of any of the assessed psychiatric disorders in the previous year, no significant differences between groups were observed in the rates of overall use of any mental health, general health, or human services. However, a significantly higher proportion of non-Latino whites reported receiving specialty care (11.8 percent) than did African Americans (7.2 percent) or Latinos (5.9 percent) (data not shown).
In Table 3, the findings of regression 1 show the relationship between ethnic or racial group and past-year use of specialty mental health services, with adjustment only for demographic variables and insurance status. The findings of the second regression show the association between ethnicity or race and past-year use of any specialty service, with adjustment for demographic variables, insurance status, income, wealth, zone of residence, and geographic location. In the third regression, psychiatric illness and disability were included as additional covariates in estimating the relationship between ethnicity and the use of specialty services.
Under regression 1, African Americans had significantly lower odds than non-Latino whites of receiving specialty use. When income, geographic location, and zone of residence were included in the regression, both African Americans and Latinos had significantly lower odds of use of specialty services than non-Latino whites. When psychiatric illness and disability were included in the regression, differences between African Americans and non-Latino whites were still significant, but differences between Latinos and non-Latino whites were not significant.
Role of income, geographic location, and zone of residence
Table 4 lists separate estimates of the associations between ethnicity or race and use of specialty services, stratified by poverty status and adjusted for demographic characteristics, insurance status, psychiatric illness, and disability. The odds ratios (ORs) of use of any specialty care by poor respondents were significantly lower for Latinos than for non-Latino whites but not for poor African Americans.
The results in Table 4 show a significant difference in the probability of any specialty care for poor respondents in the South compared with poor respondents in the Midwest. African Americans who were not poor had lower odds of receiving specialty care than whites who were not poor, and there were significant differences in receipt of specialty care between rural respondents who were not poor and their urban counterparts.
We proceeded to explore the association between ethnicity or race and use of specialty services in separate logistic regressions stratified by geographic region. The data shown in Table 5 demonstrate that African Americans living in the South or the West, compared with non-Latino whites living in those same regions, had a significantly lower probability of any use of specialty services. In this stratification, the Latino samples were too small—as evidenced by the large range for the ORs—to enable us to find anything but large significant differences for this group. A larger sample would have been required for testing of differences in the relation of specialty mental health services and Latino ethnicity.
Discussion
The lower level of access to specialty mental health care among poor Latinos compared with poor non-Latino whites is consistent with the results of other published studies (4,33,41). At least five factors could explain differences in use of specialty services between poor Latinos and poor non-Latino whites: language fluency, cultural differences such as self-reliance, access to Medicaid specialty services in Latino neighborhoods, differences in recognition of mental health problems, and lower quality of mental health care. Even though the NCS was limited to English-speaking respondents, many poor Latinos may not be fluent enough in English to feel comfortable discussing their mental health problems or participating in psychotherapy.
Previous studies have shown that psychiatric patients with limited English proficiency underutilized specialist outpatient services and that those who did receive such services were less likely to participate in psychotherapy than fluent English speakers (42). We speculate that limited English proficiency among poor Latinos in our study may have contributed to their lower use of specialty services compared with poor African Americans or whites with no linguistic barriers. If a patient with limited English proficiency cannot gain access to a bilingual provider, he or she may not seek specialty care.
A second factor may be self-reliance among poor Latinos. Self-reliance in dealing with mental health problems, a coping mechanism more commonly observed among Latinos than whites (43), reduces the use of mental health services (44). A third factor might be the access to Medicaid specialty services in Latino neighborhoods compared with neighborhoods where poor non-Latino whites live. Research has found that the more behavioral health specialists there are in a community, the more likely individuals are to use these services (45).
In one study, lack of recognition of mental health problems might also account for differences in use of specialty care. Differences in the use of mental health services between persons in Canada and persons in the United States (mostly non-Latino whites) were not significant after perceived need for mental health care was controlled for (46). This finding suggests that ethnic or racial differences in perceived need for care might explain lower rates of care.
Another explanation for the lower rates of specialty care among poor Latinos than among poor whites might be previous experience with lower-quality mental health care. In a recent study, only 24 percent of Hispanic persons with anxiety and depression received appropriate care (47), which suggests that Latinos may perceive that they have less to gain from the mental health care system.
Our findings that African Americans who were not categorized as poor were less likely to use specialty services than their white counterparts, even after adjustment for demographic variables, insurance status, and psychiatric morbidity, is supported by the results of other research (48). African Americans appear to have fewer financial resources than whites in any income bracket and may experience the modest cost sharing associated with private insurance as more of a burden than whites (49). Crude control for insurance might not eliminate the differences in the insurance benefits between African Americans and whites categorized as not being poor.
Another possible explanation for the differences we observed is greater mistrust among patients; African Americans have experienced racism and mistreatment by the health care system (50), which may discourage them from seeking specialty care. In a nationwide study, 35 percent of African Americans stated that racism was a major problem in health care, compared with only 16 percent of whites (51).
In addition, regional variations in the receipt of specialty care by ethnic and racial minorities suggest policy or system factors as topics for research. Whether these regional differences are functions of geographic location rather than different levels of availability of particular minority providers in different communities cannot be determined from the NCS data. Thus it is impossible to clarify whether eligibility policies in the South make it less likely for African Americans than for non-Latino white to obtain care or whether the difference is due to the availability of minority providers or health care system factors—for example, referrals and reimbursement procedures. Distribution of specialty facilities that serve African Americans in the South compared with those that serve non-Latino whites may account for differences in access to specialty care.
Our results are consistent with McKinlay's framework (52), which supposes that the combined effect of poverty and minority status places a person at a higher risk of reduced access to mental health services. Our findings suggest that the effect of minority status on use of specialty care services may vary depending on poverty status and geographic location. The importance of stratification underlines how the effects of ethnicity or race, poverty, and geographic region need to be analyzed in combination. In terms of specialty care use, being African American has less of an impact among poor persons than among those who are not poor, whereas the opposite is true for Latinos. Thus the effects of ethnicity and race should not be examined alone but in terms of how they interact with poverty and region.
The fact that the magnitude of the association between ethnicity and the use of specialty services did not substantially change after adjustment for psychiatric morbidity and other covariates suggests that ethnicity and race may be a component of a more complex construct of social position. Subjective social class, perceived placement in the community, and relative deprivation may all be important variables—not measured in the NCS study—that, in addition to race, income, and wealth, define a person's social position. Furthermore, income can be confounded by other dimensions of health that were not measured in this study (53). More detailed information about environmental context is also required for modeling the effects of the neighborhood—for example, the neighborhood's environment and cohesion. Such information portrays commonly held views about life that may affect psychiatric illness and pathways to treatment.
This study had several limitations. The NCS study was conducted in the pre-managed care era, so there are no data on how the results of our study might vary under newer health care organization and financing structures. In addition, the cross-sectional design of the study makes it difficult to establish the causal pathways of differential rates of use of specialty services among different ethnic and racial minorities. Selective migration to geographic regions where specialty services are not easily accessible could explain some of the observed ethnic or racial differences. The exclusion of other social and lifestyle factors that were not available in the data set could also change the strength of the correlations with some of the independent variables. Furthermore, some of the observed results may have been due to measurement error in ethnic and racial data (54).
Operationalization of the constructs of race or ethnicity in the NCS follows a crude approach. The survey merely asks respondents to indicate their race or ethnicity by choosing from one of several response options, which might be arbitrary depending on the types and number of categories provided (55). The conceptual validity of these constructs has been challenged (56).
Another limitation of the NCS is that all interviews were conducted in English. Latino, Spanish-speaking, monolingual respondents were effectively excluded from the survey. This bias might have served to underestimate the effects of ethnicity or race on use of specialty services, if we assume that these ethnic minorities are less likely to seek care as a result of increased barriers, such as language barriers, lack of knowledge about how to navigate the service sectors, and undocumented immigration status.
Conclusions
The results of this study underline the urgent need for action to augment access to specialty care for poor Latinos and African Americans who are not categorized as poor. Public policy changes, such as increasing consumers' cost sharing for services or monitoring the availability of bilingual specialty providers by regions, should be carefully reviewed. It is necessary to ensure the availability and effectiveness of psychiatric services tailored to meet the needs of Latino and African-American communities. Furthermore, given the social and regional differences in specialty care, research may need to refocus on how to best target these inequalities at the community and system level, beyond the mere study of individual factors leading to increased access to care.
Dr. Alegría is affiliated with Cambridge Health Alliance, Center for Multicultural Mental Health Research, 120 Beacon Street, Fourth Floor, Somerville, Massachusetts 02143 (e-mail, [email protected]). Dr. Canino is with the Behavioral Sciences Research Institute of the University of Puerto Rico in San Juan. Dr. Ríos, Dr. Vera, and Mr. Calderón are with the Center for Evaluation and Sociomedical Research of the University of Puerto Rico. Mr. Rusch is with the department of psychology of the University of Illinois in Champaign. Dr. Ortega is with the division of health policy and administration of the department of epidemiology and public health at Yale University in New Haven, Connecticut. This paper is part of a special section on disparities in mental health care for Latinos.
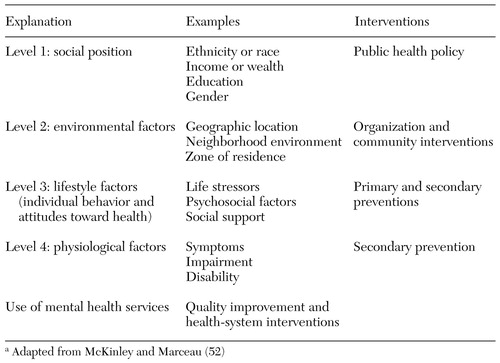 |
Table 1. Levels of explanation and corresponding types of interventions for psychiatric illnessa
a Adapted from McKinley and Marceau (52)
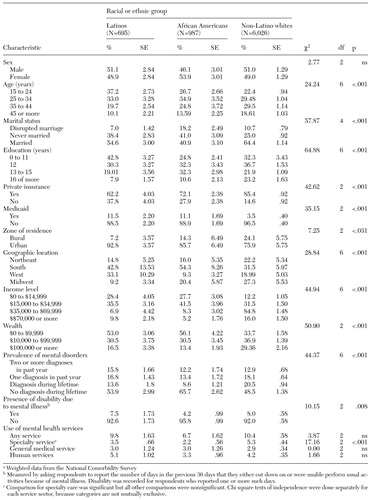 |
Table 2. Demographic and socioeconomic characteristics, psychiatric morbidity, and service use among Latinos, African Americans, and non-Latino whitesa
a Weighted data from the National Comorbidity Survey
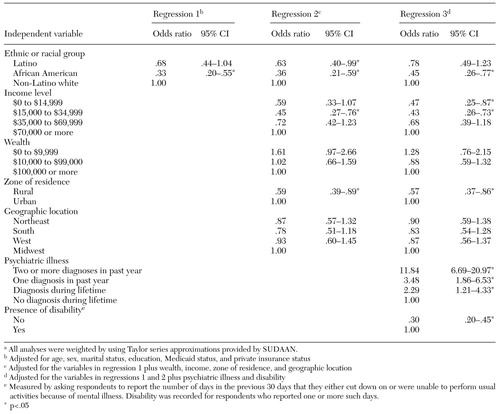 |
Table 3. Adjusted associations between use of any specialty mental health service and ethnic or racial groupa
a All analyses were weighted by using Taylor series approximations provided by SUDAAN.
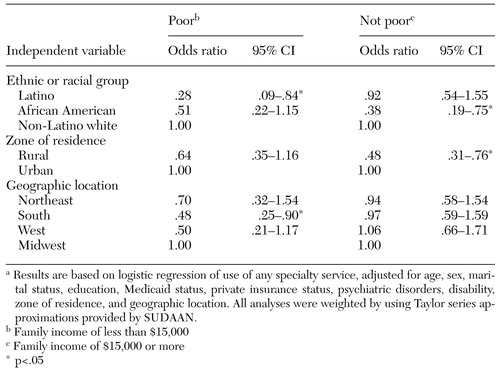 |
Table 4. Adjusted associations between use of any specialty mental health service and ethnic or racial group, zone of residence, and geographic location, by poverty level
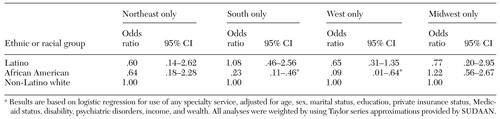 |
Table 5. Adjusted associations between use of any specialty mental health service and ethnic or racial group and income, stratified by geographic locationa
a Results are based on logistic regression for use of any specialty service, adjusted for age, sex, marital status, education, private insurance status, Medicaid status, disability, psychiatric disorders, income, and wealth. All analyses were weighted by using Taylor series approximations provided by SUDAAN.
1. Bernal G, Bonilla J, Belido C: Ecological validity and cultural sensitivity for outcome research: issues for the cultural adaptation and development of psychosocial treatments with Hispanics. Journal of Abnormal Child Psychology 23:67-82, 1995Crossref, Medline, Google Scholar
2. Lawson WB: Racial and ethnic factors in psychiatric research. Hospital and Community Psychiatry 37:61-65, 1986Abstract, Google Scholar
3. Temkin-Greener H, Clark KT: Ethnicity, gender, and utilization of mental health services in a Medicaid population. Social Science Medicine 26:989-996, 1988Crossref, Medline, Google Scholar
4. Padgett DK, Patrick CP, Burns BJ, et al: Ethnicity and the use of outpatient mental health services in a national insured population. American Journal of Public Health 84:222-226, 1994Crossref, Medline, Google Scholar
5. Wagstaff A, van Doorslaer E: Income inequality and health: what does the literature tell us? Annul Review of Public Health 21:543-567, 2000Google Scholar
6. Willams DR, Rucker TD: Understanding and addressing racial disparities in health care. Health Care Financing Review 21(4):75-90, 2000Google Scholar
7. Mental Health: A Report of the Surgeon General. Washington, DC, Department of Health and Human Services, 1999Google Scholar
8. Kessler RC, Zhao S, Katz SJ, et al: Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. American Journal of Psychiatry 156:115-123, 1999Link, Google Scholar
9. Woodward AM, Dwinell AD, Arons BS: Barriers to mental health care for Hispanic Americans: a literature review and discussion. Journal of Mental Health Administration 19:224-236, 1992Crossref, Medline, Google Scholar
10. Ruiz P: Access to health care for uninsured Hispanics: policy recommendations. Hospital and Community Psychiatry 44:958-962, 1993Abstract, Google Scholar
11. Ginzburg E: Access to health care for Hispanics. JAMA 265:238-241, 1991Crossref, Medline, Google Scholar
12. Vega WA, Kolody B, Aguilar-Gaxiola S, et al: Gaps in service utilization by Mexican-Americans with mental health problems. American Journal of Psychiatry 156:928-934, 1999Link, Google Scholar
13. Gallo JJ, Marino S, Ford D, et al: Filters on the pathway to mental health care: II. sociodemographic factors. Psychological Medicine 25:1149-1160, 1995Crossref, Medline, Google Scholar
14. Sue S, Fujino DC, Hu I, et al: Community mental health services for ethnic minority groups: a test of the cultural responsiveness hypothesis. Journal of Consulting and Clinical Psychology 59:533-540, 1991Crossref, Medline, Google Scholar
15. Scheffler RM, Miller AB: Demand analysis of mental health service use among ethnic subpopulations. Inquiry 26:202-215, 1989Medline, Google Scholar
16. Wells KB, Golding JM, Hough RL, et al: Acculturation and the probability of use of health services by Mexican Americans. Health Services Research 24:237-257, 1989Medline, Google Scholar
17. Hough RL, Landsverk JA, Karno M, et al: Utilization of health and mental health services by Los Angeles Mexican Americans and non-Hispanic whites. Archives of General Psychiatry 44:702-709, 1987Crossref, Medline, Google Scholar
18. Portes A, Kyle D, Eaton WW: Mental illness and help-seeking behavior among Mariel Cuban and Haitian refugees in South Florida. Journal of Health and Social Behavior 33:283-298, 1992Crossref, Medline, Google Scholar
19. Alegría M, Robles R, Freeman DH, et al: Patterns of mental health utilization among island Puerto Rican poor. American Journal of Public Health 81:875-879, 1991Crossref, Medline, Google Scholar
20. Alegría M, Kessler R, Bijl R, et al: Comparing data on mental health service use between countries, in Unmet Need for Treatment. Edited by Andrews G, Henderson S. Cambridge, Cambridge University Press, 2000Google Scholar
21. Mezzich JE, Kleinman A, Fabrega H, et al: Cultural proposals and supporting papers for DSM-IV. Submitted to the DSM-IV task force by the Steering Committee, NIMH-sponsored group on culture and diagnosis, 1993Google Scholar
22. Guarnaccia PJ: Ataques de nervios in Puerto Rico: culture-bound syndrome or population illness? Medical Anthropology 15:1-14, 1992Google Scholar
23. Flaskerud JH, Hu L: Racial/ethnic identity and amount and type of psychiatric treatment. American Journal of Psychiatry 149:379-384, 1992Link, Google Scholar
24. Solis JM, Marks G, Garcia, M, et al: Acculturation, access to care, and use of preventive services by Hispanics: findings from HHANES 1982-84. American Journal of Public Health 80(suppl):11-19, 1990Medline, Google Scholar
25. Holzer CE, Shea BM, Swanson JW, et al: The increased risk for specific psychiatric disorders among persons of low socioeconomic status. American Journal of Social Psychiatry 20:259-271, 1986Google Scholar
26. Alegría M, Bijl R, Lin E, et al: Income differences in persons seeking outpatient treatment for mental disorders: a comparison of the US with Ontario and the Netherlands. Archives of General Psychiatry 57:383-391, 2000Crossref, Medline, Google Scholar
27. Snowden LR: Psychiatric inpatient care and ethnic minority populations, in Cross Cultural Psychiatry. Edited by Herrera JM, LawsonWB, Sramek JJ. Chichester, England, Wiley, 1999Google Scholar
28. MacIntyre S, MacIver S, Sooman A: Area, class, and health: should we be focusing on places or people? Journal of Social Policy 22:213-234, 1993Google Scholar
29. Kessler RC, McGonagle KA, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry 51:8-19, 1994Crossref, Medline, Google Scholar
30. Kessler RC, McGonagle KA, Nelson CB, et al: Sex and depression in the National Comorbidity Survey: II: cohort effects. Journal of Affective Disorders 30:15-26, 1994Crossref, Medline, Google Scholar
31. Blazer DG, Kessler RC, McGonagle KA, et al: The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. American Journal of Psychiatry 151:979-986, 1994Link, Google Scholar
32. Katz SJ, Kessler RC, Frank RG, et al: The use of outpatient mental health services in the United States and Ontario: the impact of mental morbidity and perceived need for care. American Journal of Public Health 87:1136-1143, 1997Crossref, Medline, Google Scholar
33. Williams DR, Collins C: US socioeconomic and racial differences in health: patterns and explanations. Annual Review of Sociology 21:349-387, 1995Crossref, Google Scholar
34. Marmot M: Multi-level approaches to understanding social determinants, in Social Epidemiology. Edited by Berkman L, Kawachi I. Oxford, England, Oxford University Press, 1999Google Scholar
35. United States Census Bureau: Historical Poverty Tables. Available at http://www.census.govhhes/poverty/histpov/hstpov1.htmlGoogle Scholar
36. Leaf PJ, Bruce ML, Tischler GL: Factors affecting the utilization of specialty and general medical mental health services. Medical Care 20:9, 1988Crossref, Google Scholar
37. Lin E, Parikh SV: Sociodemographic, clinical, and attitudinal characteristics of the untreated depressed in Ontario. Journal of Affective Disorders 53:153-162, 1999Crossref, Medline, Google Scholar
38. Composite International Diagnostic Interview (CIDI). Version 1.0. Geneva, World Health Organization, 1990Google Scholar
39. Wittchen HU: Reliability and validity studies of the WHO Composite International Diagnostic Interview (CIDI): a critical review. Psychiatry Research 28:57-84, 1994Crossref, Google Scholar
40. Shah BV, Barnwall BC, Bieler GS: SUDAAN User's Manual, release 7.5. Research Triangle Park, NC, Research Triangle Institute, 1997Google Scholar
41. Pappas G, Quees S, Hadden W, et al: The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. New England Journal of Medicine 329:103-109, 1993Crossref, Medline, Google Scholar
42. Stuart GW, Minas IH, Klimidis S, et al: English language ability and mental health service utilization: a census. Australian and New Zealand Journal of Psychiatry 30:270-277, 1996Crossref, Medline, Google Scholar
43. Chapman PL, Mullis RL: Racial differences in adolescent coping and self-esteem. Journal of Genetic Psychology 161:152-160, 2000Crossref, Medline, Google Scholar
44. Ortega AN, Alegría MA: Self-reliance, mental health need, and the use of mental healthcare among island Puerto Ricans. Mental Health Services Research 4:131-140, 2002Crossref, Medline, Google Scholar
45. Horgan CM: The demand for ambulatory mental health services from specialty providers. Health Services Research 21:291-319, 1986Medline, Google Scholar
46. Katz SJ, Kessler RC, Frank RG, et al: The use of outpatient mental health services in the United States and Ontario: the impact of mental morbidity and perceived need for care. American Journal of Public Health 87:1136-1143, 1997Crossref, Medline, Google Scholar
47. Young AS, Clap R, Sherbourne CD, et al: The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry 58:55-61, 2001Crossref, Medline, Google Scholar
48. Snowden LR, Thomas K: Medicaid and African American outpatient mental health treatment. Mental Health Services Research 2:115-120, 2000Crossref, Medline, Google Scholar
49. Krieger N: Counting accountability: implications of the new approaches to classifying race/ethnicity in the 2000 Census. American Journal of Public Health 90:1687-1689, 2000Crossref, Medline, Google Scholar
50. Diala C, Muntaner C, Walrath C, et el: Racial differences in attitudes toward professional mental health care and in the use of services. American Journal of Orthopsychiatry 70:455-464, 2000Crossref, Medline, Google Scholar
51. Lillie-Blanton M, Brodie M, Rowland D, et al: Race, ethnicity, and the health care system: public perceptions and experiences. Medical Care and Research Review 57 (suppl 1):218-235, 2000Medline, Google Scholar
52. McKinlay JB, Marceau LD: A tale of 3 tails. American Journal of Public Health 89:295-298, 1999Crossref, Medline, Google Scholar
53. Lantz PM, House JS, Lepkowski JM, et al: Socioeconomic factors, health behaviors, and mortality. JAMA 279:1703-1708, 1998Crossref, Medline, Google Scholar
54. Williams DR: African-American health: the role of the social environment. Journal of Urban Health: Bulletin of the New York Academy of Medicine 75:300-321, 1998Medline, Google Scholar
55. Good BJ: Culture, diagnosis, and comorbidity. Culture Medicine and Psychiatry 16:427-446, 1992-93Medline, Google Scholar
56. Beutler LE, Brown MT, Crothers L, et al: The dilemma of factitious demographic distinctions in psychological research. Journal of Consulting and Clinical Psychology 64:892-902, 1996Crossref, Medline, Google Scholar




