Datapoints: Trends in Psychiatric Practice, 1988-1998: I. Demographic Characteristics of Practicing Psychiatrists
The past decade has seen important changes in the practice of psychiatry. This first of three reports examines changes in the demographic characteristics of practicing psychiatrists that are evident from the results of two large national surveys.
The 1988-1989 Professional Activities Survey (PAS) (1) included 19,498 responses to a mailed survey targeting an unduplicated list of all American Psychiatric Association (APA) members (68 percent response) and all self-identified psychiatrists from the American Medical Association master file who were not APA members (29 percent response). The 1998 National Survey of Psychiatric Practice (NSPP) (2) included 871 responses to a mailed survey that targeted a stratified random sample of the APA membership (71 percent response). Both samples were limited to psychiatrists in active practice.
Figure 1 highlights the changing landscape of psychiatric practitioners. Between 1988 and 1998, the mean age of the psychiatric workforce increased—from 49.6 years to 50.9 years. The number of young psychiatrists in the field decreased significantly. In addition, more women and non-Caucasians were practicing psychiatry in 1998.
These findings are consistent with those of a 1996 survey (3) and provide evidence that these trends are continuing. The psychiatric profession has apparently failed to attract a younger cohort to replace retiring practitioners. A growing proportion of women, who tend to work fewer hours, are entering the workforce. Presumably the larger proportion of minority psychiatrists is partly associated with an increase in the number of U.S. residency slots that are filled by international medical graduates. This trend may have an impact on workforce capacity because international graduate psychiatrists are more likely to work in the public sector (4).
The demographic characteristics of U.S. psychiatrists are changing. Although the reasons are not obvious, the changes have important implications for medical education, residency training, and workforce planning.
Dr. Marcus is affiliated with the University of Pennsylvania School of Social Work, 3719 Locust Walk, Philadelphia, Pennsylvania 19104 (e-mail [email protected]). Ms. Suarez and Ms. Tanielian are with Rand in Arlington, Virginia. Dr. Pincus, who is coeditor of this column with Ms. Tanielian, is affiliated with Rand and the department of psychiatry at the University of Pittsburgh School of Medicine.
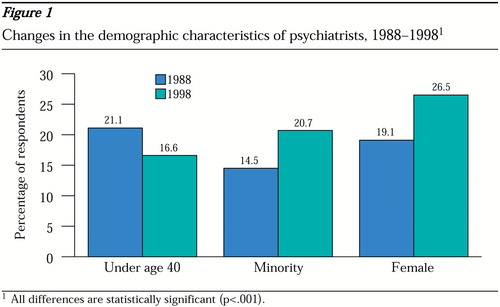
Figure 1. Changes in the demographic characteristics of psychiatrists, 1988-199811
All differences are statistically significant (p<001).
1. Dorwart RA, Chartock LR, Dial T, et al: A national study of psychiatrists' professional activities. American Journal of Psychiatry 149:1499-1505, 1992Link, Google Scholar
2. National Survey of Psychiatric Practice. Washington, DC, American Psychiatric Association, Office of Research, 1998Google Scholar
3. Zarin DA, Pincus HA, Peterson BD, et al: Characterizing psychiatry with findings from the 1996 National Survey of Psychiatric Practice. American Journal of Psychiatry 155:397-404, 1998Link, Google Scholar
4. Blanco C, Carvalho C, Olfson M, et al: Practice patterns of international and US medical graduate psychiatrists. American Journal of Psychiatry 156:445-450, 1999Abstract, Google Scholar



