A Public Health Perspective on Violent Offenses Among Persons With Mental Illness
Abstract
OBJECTIVE: This study reanalyzed existing data to assess the extent to which persons with mental illness might contribute to criminal violence in the community. METHODS: Data were examined from a representative sample of 1,151 remanded offenders who underwent a full structured diagnostic interview that was used to provide one-month prevalence rates of mental illnesses as defined by the Structured Clincal Interview for DSM-III-R. Diagnoses of interest were mood, psychotic, anxiety, psychoactive substance use, adjustment, and miscellaneous axis I disorders and axis II personality disorders. Criminological data describing the number of offenses against persons and property and the number of victimless crimes were abstracted from police arrest reports and warrants. A violent crime was defined as any crime against a person. RESULTS: The one-month prevalence of major mental and substance use disorders of newly admitted inmates was 61 percent. About 3 percent of violent offenses could be attributed to individuals who had a principal diagnosis of any non-substance use-related disorder. An additional 7 percent of violent offenses could be attributed to individuals who had a primary diagnosis of a substance use disorder. CONCLUSIONS: The results of the study support the hypothesis that people with mental and substance use disorders are not major contributors to police-identified criminal violence. Public perceptions of mentally ill persons as criminally dangerous appear to be greatly exaggerated.
Reducing stigmatization of persons with mental illness is a major goal of organizations that work to improve treatment, research, and tolerance for this population. Acts of criminal violence by mentally ill persons are often highly publicized and have a powerful impact on public fears, which can undermine efforts to achieve this goal.
An ongoing question about persons with mental illness is whether they are more likely than the general population to commit violent acts (1). Results of studies conducted before 1980 consistently showed that persons with a serious mental illness such as schizophrenia were no more likely—and often were less likely—to commit a violent or criminal act than persons who did not have a mental illness (2,3). However, more recent studies have reported higher than average rates of violence among persons with mental illnesses or substance use disorders (4,5,6,7,8,9,10).
Despite the change in the statistical trend, it is unlikely that a large portion of community violence is attributable to persons with mental illness (1), although few studies have directly addressed this important public health issue. The vast majority of persons with mental illness do not commit acts of violence (11). When people in this population do act violently, their most likely target is a close family member rather than a stranger (12). Even within families, the prevalence of violence is low. Estroff and colleagues (13) found that only 2 percent of individuals in close family networks of persons with serious mental illness were targets of violence, and most of them were mothers who were involved in a reciprocally threatening and hostile relationship with a child who was diagnosed as having schizophrenia and a co-occurring substance abuse problem, who was not receiving treatment, and who was financially dependent.
Using data from the Epidemiologic Catchment Area study, Wessely (14) estimated that only 3 percent of all violent incidents that occurred in the community could be attributed to persons with mental illness.
Although many acts of violence never come to the attention of law enforcement officials, violent acts that are identified as having been committed by a mentally ill person are those most often sensationalized in the media, further fueling public fear and intolerance (15).
The study reported here used a public health approach to determine the proportion of violent, remanded crimes in the community that could be attributed to persons with a defined Structured Clinical Interview for DSM-III-R (SCID) mental disorder, specifically a mood, psychotic, anxiety, adjustment, psychoactive substance use, or miscellaneous other axis I disorder or an axis II personality disorder. We were particularly interested in violent crimes attributable to individuals with an axis I disorder. Axis II disorders were of less interest because of the complexities associated with accurately identifying antisocial personality disorders in incarcerated populations.
Methods
The data analyzed in this study were originally collected and analyzed in 1992 to estimate the prevalence of DSM-III-R mental disorders in a pretrial population (16). The methods and other findings are described in more detail in the original and subsequent studies (17,18).
The original study was conducted at the only detention center serving a geographic catchment area of 1.5 million residents in the southern portion of a province in western Canada. A majority of inmates entered this facility as prearraignment cases; a minority were sentenced prisoners who were in transit, on courtesy holds, or serving intermittent sentences (on weekends, for example). As there were no diversion programs operating in the area at the time, the police had virtually no opportunity to redirect criminally violent offenders to alternative mental health dispositions. The study received ethical review and approval from the University of Calgary bioethics committee and from the Department of Justice in Alberta.
Participants
Inmates were selected by random sampling from daily admission logs between July and December 1992. All selected inmates were approached for an interview within 24 hours of their admission to the facility, before any bail hearings, forensic transfers, or other releases. A total of 4,770 inmates were admitted during the study months. Of these, 1,151 were asked to participate in the study; 326 refused, yielding a response rate of 78 percent and a sampling fraction of about 25 percent. This response rate was considered to be acceptable, given that the inmates were not remunerated for their participation. Thirty-three inmates were ineligible for interviewing because of language or logistical barriers—for example, inaccessibility because of court appearances, consultations with officers of the court, or meetings with counsel.
No demographic differences were noted among the inmates who agreed to participate and those who refused. There were no significant differences between the sample group and the population of offenders admitted during the study period in terms of age, gender, ethnicity, education, category of crime, and month of admission. Because the sample was representative of all remanded offenders in a geographically defined area, it served as an appropriate basis for drawing population-based inferences.
Data collection
After a structured clinical interview, each participant received a single primary diagnosis from one of four forensic psychiatrists. The SCID Non-patient edition, modules B and C of the SCID Patient edition (19), and the Psychopathic Checklist (20) were used to structure the interview session and assist in the diagnostic formulation of all major DSM-III-R disorders. A substudy confirmed interrater reliability for SCID diagnoses, with partial kappa coefficients ranging from .80 to 1 for broad disorder categories. Interrater agreement was monitored throughout the study with an evaluation after every 200 interviews.
Crime data detailing criminal code offenses were obtained from official police arrest reports and warrants of remand. All crimes against persons were considered violent offenses. Nonviolent offenses were defined as crimes against property and victimless offenses.
Results were based on the one-month prevalence of SCID-defined principal diagnoses. A principal diagnosis was defined as the only condition present or, when more than one condition was present, the most important condition or the condition resulting in the most difficulty or functional impairment. Primary diagnoses were assigned by use of conventional DSM-III-R hierarchical and exclusion rules. Consequently, they are not directly comparable to those in studies that use nonhierarchical assignment rules—prevalence rates for certain mental disorders are higher when nonhierarchical rules are used—and specific combinations of comorbidities cannot be assessed.
The prevalence of antisocial personality disorder in incarcerated populations is typically high when DSM-III-R-based criteria are used because of their emphasis on law-breaking and arrest-prone behaviors. To avoid inflating the prevalence of axis II disorders, interviewers asked participants who received a diagnosis of antisocial personality disorder by means of the SCID also to complete the Psychopathic Checklist. Only participants who exceeded the checklist's recommended threshold were considered to have antisocial personality disorder and counted as meeting the criteria for an axis II diagnosis.
The use of primary diagnoses and the restrictive criteria for antisocial personality disorder will yield lower axis II prevalence figures than those reported in other studies. Given that our interest was in axis I disorders, this effect did not pose a significant interpretation problem.
Results
Sample characteristics
Table 1 presents detailed characteristics of the study participants. A total of 1,045 of the 1,151 participants were men (91 percent). Male and female participants did not differ significantly in age distributions. The mean±SD age was 28±8.8 years. Although both men and women had low educational levels, a significantly larger proportion of women had not attended high school (χ2=9.33, df=3, p=.025). Also, a significantly larger proportion of women were of aboriginal origin (χ2=22.87, df=2, p<.001).
The 1,151 participants had accrued a total of 4,991 charges for the current incarceration: 537 crimes against persons (10.8 percent), 1,622 crimes against property (32.5 percent), and 2,832 victimless offenses (56.7 percent). The distribution of charges was similar for men and women. A significantly larger proportion of men were charged with a violent offense (27 percent versus 18 percent; χ2=4.23, df=1, p=.04).
Despite the use of restrictive diagnostic criteria, psychiatric morbidity among the participants was relatively high. A total of 703 participants (61.1 percent) received a principal diagnosis involving either an axis I mental disorder or an axis II personality disorder. Distributions of diagnoses did not differ significantly between men and women. Two of every three diagnoses were psychoactive substance use disorders (mostly alcohol related), making these the most prevalent of any disorder type. Psychotic disorders (mostly schizophrenia) were the least prevalent.
As expected, the prevalence of axis II disorders was low. Less than a third of the participants met the criteria for a personality disorder. The proportions of men and women who received a diagnosis of any axis II personality disorder were similar. A total of 187 participants (16 percent)—167 men (16 percent) and 20 women (19 percent)—were diagnosed as having both an axis I and an axis II disorder. Finally, one in five inmates reported having made one or more suicide attempts. Women were significantly more likely to report a history of suicide attempts (χ2=9.97, df=3, p=.02).
Prevalence of violence
Because offenders could have been charged with multiple offenses, a comparison of the proportion of violent offenders in each diagnostic category with the proportion of violent offenses is presented in Table 2.
Charges were grouped into three broad categories: charges against persons (all physical attacks or physical threats, including assault, sexual assault, and murder), property crimes (all theft or destruction of property), and miscellaneous victimless crimes (for example, motor traffic violations, drug offenses, disturbing the peace, and trespassing). The number of offenses allegedly committed by offenders with mental disorders was generally proportionate to their number in the inmate population. The largest discrepancy was only 3 percent, for offenders with non-substance-use disorders. For example, 5 percent of the participants had mood disorders (Table 1), and participants with mood disorders accounted for 6 percent of the violent offenders and 5 percent of the violent charges (Table 2).
Participants with substance use disorders accounted for almost half of all violent offenses (49 percent), whereas participants with psychotic disorders accounted for less than 1 percent. One of every six violent offenses was committed by a person with a non-substance-use disorder, whereas one of every two was committed by a person with a primary substance use disorder.
The data summarized in Table 3 were used to examine whether offenders with mental disorders were charged with more serious offenses than those without mental illness. Offense categories were ranked according to their seriousness, from victimless offenses to violent offenses. Chi square analysis was used to compare differences in the proportions of these types of offense in each diagnostic group with those of offenders who had no diagnosis.
An inverse trend between the frequency of an offense and its severity was noted. Of the 4,991 offenses, 537 (11 percent) were classified as violent. Crimes of violence had the lowest frequencies, typically constituting about 10 percent of all the offenses in each diagnostic group. Victimless crimes accounted for 57 percent of all offenses and had the highest frequencies in each diagnostic group (range= 50 percent to 72 percent). As Table 3 shows, when compared with offenders with no diagnosis, only two diagnostic groups showed a significant trend: a significantly greater proportion of violent offenses were committed by offenders with a principal diagnosis of adjustment disorder and a significantly smaller proportion of violent offenses were committed by offenders with a psychotic disorder.
Violent offenses attributable to persons with mental disorders
Table 4 presents calculations of the incidence rates of violent offenses per 1,000 offenders for those with no disorder and for violent offenders with a mental disorder in three broad categories: non-substance-use disorders, substance use disorders, and all axis I disorders combined. Numerators for the calculations were the number of violent offenses attributable to offenders in each diagnostic category, and denominators were the total number of individuals in that group.
Table 4 also presents the attributable fraction exposed—that is, the percentage by which the incidence rate for each diagnostic category would have to drop in order to match the rate among offenders without a disorder. For public health planners, this calculation represents the reduction that would occur if the exposure in question—in this case, mental illness—could be entirely eliminated or prevented (21). Finally, by expressing the theoretically preventable offenses as a proportion of all violent offenses in our sample, the extent to which persons with mental illness may contribute to violent remanded crime was estimated.
The incidence of violent offenses was higher among offenders in all diagnostic groups than among offenders with no disorder. To be comparable to the rate among offenders with no disorder, the incidence of violent offenses among persons with any mental disorder would have to drop by 16 percent, or 55 offenses. A reduction of this magnitude would yield a reduction of only 10 percent of the 537 violent offenses in this sample. Stated another way, one in ten violent crimes in our sample could be attributed to persons with a mental or substance use disorder. The bulk of these offenses—about 7 percent—were attributable to offenders with a primary substance use disorder and only about 3 percent to offenders with a primary non-substance-use mental disorder.
Discussion
Results from this study show a relatively high one-month prevalence (61 percent) of any principal axis I disorder—about 46 percent for substance use disorders and 15 percent for non-substance-use disorders. High prevalences of mental illness and substance use disorders among remanded populations have been consistently reported in Canada (22,23,24), the United States (25,26,27,28), and the United Kingdom (29,30), with higher prevalences reported in studies that do not use DSM-III-R hierarchical exclusion rules and those that estimate the lifetime prevalences of the disorders.
The high rate of mental disorders among pretrial offenders relative to community samples (31,32,33) is generally considered to be a result of poorly executed deinstitutionalization and community care policies (34). Proponents of the "criminalization hypothesis" argue that inadequate housing, lack of assertive community-based mental health treatment programs, and inaccessibility of long-stay inpatient beds have resulted in the incarceration of large numbers of persons with mental illness, often for minor offenses.
However, with only two exceptions, the offenders with mental disorders in our sample were not more likely to be charged with a minor offense. Indeed, as a group, their charge profile was similar to that of offenders without mental illness. With respect to the exceptions, offenders with adjustment disorders were more likely to be charged with a violent offense, and those with a psychotic disorder were less likely. Therefore, our results support the criminalization hypothesis only for offenders with a psychotic disorder—a minority of offenders in our sample.
The notion that mentally ill individuals are dangerous and pose a significant risk of violence to the public reinforces social stigma and discrimination and reduces opportunities for successful community integration and improved quality of life (3). The results of our study support previous speculations that the public's fear greatly exceeds the actual risk (1). Using a public health approach (21), we calculated the proportion of violent offenses that could be attributed to persons with mental illness. Less than 3 percent of violent crimes could be attributed to persons with a principal diagnosis reflecting a non-substance-use disorder—that is, a mood, psychotic, anxiety, adjustment, or miscellaneous other axis I disorder or an axis II personality disorder—and an additional 7 percent could be attributed to those with a principal psychoactive substance use disorder.
Because our sample was representative of all offenders arrested and detained by police for violent crimes in a geographically defined area, these findings support the hypothesis that the public risk of criminal violence by a person with a mental disorder or a substance use disorder is low. From the perspective of public health interventions, only one in ten violent crimes in our sample could have been prevented if these disorders did not exist.
With respect to generalizability to other locales, the generally low base rates of criminal violence in Canada will inflate the overall estimate, because the denominator for the calculation—the total number of violent crimes—was small. In societies with a high baseline rate of criminal violence, the denominator will be much larger and the proportion of violent offenses attributable to persons with mental illness much smaller (35).
Furthermore, different arrest and detention policies, particularly with respect to diversion to treatment, could significantly alter results. Our study took place in an area where law enforcement officers seldom used their discretion to divert violent offenders to mental health alternatives. No formal diversionary programs existed, and access to assessment and treatment through forensic psychiatric programs was good. Transfers out of the justice system to mental health alternatives were still possible but did not usually occur within 24 hours after detention. Because we interviewed newly admitted offenders within the first 24 hours of detention, results will more closely estimate the true relationship between mental illness and crime at the community level (36). Studies of inmates conducted later in their pretrial detention or after they have been sentenced may yield lower crime rates among offenders with mental illness (29).
This study could not examine the specific, fear-inducing qualities of violent crime committed by mentally ill individuals, and no data were obtained on the relationship of the victim to the perpetrator. Future research should examine the extent to which persons with mental illness commit seemingly random violent acts that are distinguishable by their bizarre or fear-inducing qualities. The extent to which public perceptions may be influenced by these qualitative characteristics should also be investigated. A typology of violence would be a useful first step—one, as Marzuk (37) has suggested, capable of distinguishing between the young man who robs a convenience store and the elderly woman who strikes out at imaginary demons with her cane.
Conclusions
The belief that mentally ill persons are dangerous is the cornerstone of public apprehension and fear about this population. In turn, community intolerance has influenced the placement of transitional housing, the availability of community treatment options, and employment opportunities (1,2). Recent research showing higher rates of violence among subgroups of mentally ill persons may support this view and inadvertently reinforce social stigma and discrimination (15). By adopting a public health perspective, studies such as ours can show that people with mental and substance use disorders are not major contributors to community violence, and by so doing, perhaps help diminish public fear and intolerance.
Acknowledgments
This study received financial support from the Department of the Solicitor General (now the Department of Justice) in Alberta, Canada, and the research and development committee of Calgary General Hospital.
Dr. Stuart is associate professor in the department of community health and epidemiology and the department of psychiatry and Dr. Arboleda-Flórez is professor and head of the department of psychiatry at Queen's University, Abramsky Hall, Kingston, Ontario K7L 3N6, Canada (e-mail, [email protected]). A version of this paper was presented at the annual meeting of the American Psychiatric Association held May 13-18, 2000, in Chicago.
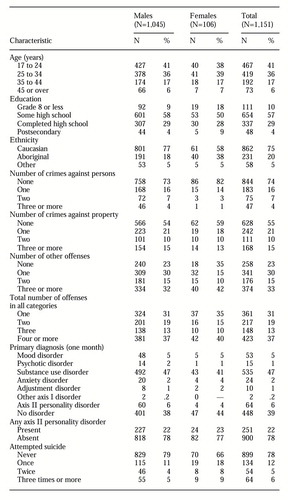 |
Table 1. Characteristics of participants in a study of violent behavior among offenders with mental illness
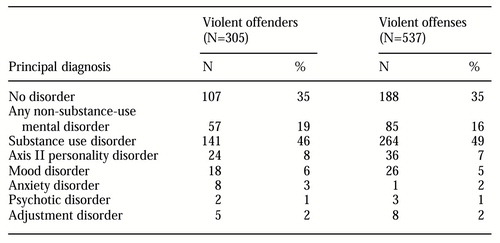 |
Table 2. Percentage of violent offenders and violent charges among inmates with no disorders and those with psychiatric and substance use disorders
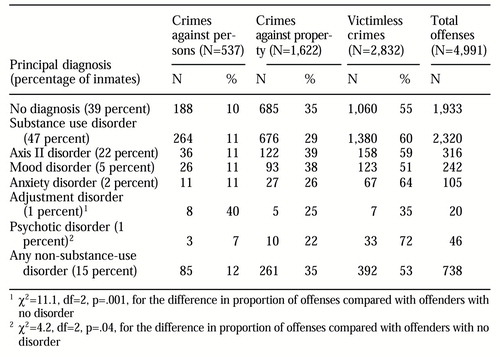 |
Table 3. Number and types of charges among inmates with no disorders and those with psychiatric and substance use disorders
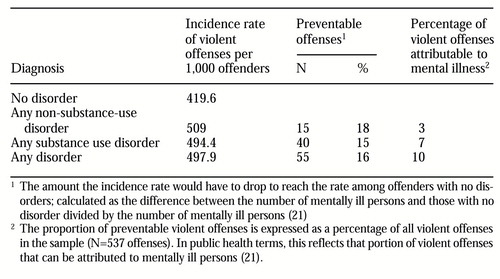 |
Table 4. Violent offenses, preventable offenses, and offenses attributable to mental illness among inmates with no disorders and those with psychiatric and substance use disorders
1. Pescosolido BA, Monahan J, Link BG, et al: The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. American Journal of Public Health 89:1339-1345, 1999Crossref, Medline, Google Scholar
2. Link BG, Stueve A: Evidence bearing on mental illness as a possible cause of violent behavior. Epidemiologic Reviews 17:172-181, 1995Crossref, Medline, Google Scholar
3. Hwang SD, Segal SP: Criminality of the mentally ill in sheltered care: are they more dangerous? International Journal of Law and Psychiatry 19:93-105, 1996Google Scholar
4. Mullen PE: A reassessment of the link between mental disorder and violent behaviour, and its implications for clinical practice. Australian and New Zealand Journal of Psychiatry 31:3-11, 1997Crossref, Medline, Google Scholar
5. Bland R, Orn H: Family violence and psychiatric disorder. Canadian Journal of Psychiatry 31:129-137, 1986Crossref, Medline, Google Scholar
6. Swanson JW, Holzer CE, Ganju VK, et al: Violence and psychiatric disorder in the community: evidence from the Epidemiologic Catchment Area surveys. Hospital and Community Psychiatry 41:761-770, 1990Abstract, Google Scholar
7. Eronen M, Hakola P, Tiihonen J: Mental disorders and homicidal behavior in Finland. Archives of General Psychiatry 53:497-501, 1996Crossref, Medline, Google Scholar
8. Hodgins S, Mendick SA, Brenan PA, et al: Mental disorder and crime: evidence from a Danish birth cohort. Archives of General Psychiatry 53:489-495, 1996Crossref, Medline, Google Scholar
9. Stueve A, Link BG: Violence and psychiatric disorders: results from an epidemiological study of young adults in Israel. Psychiatric Quarterly 66:327-342, 1997Crossref, Google Scholar
10. Swanson JW, Estroff S, Swartz M, et al: Violence and severe mental disorder in clinical and community populations: the effects of psychotic symptoms, comorbidity, and lack of treatment. Psychiatry 60:1-22, 1997Crossref, Medline, Google Scholar
11. Lamberg L: Mental illness and violent acts: protecting the patient and the public. JAMA 280:407-408, 1988Crossref, Google Scholar
12. Tardiff K, Marzuk PM, Leon AC, et al: A prospective study of violence by psychiatric patients after hospital discharge. Psychiatric Services 48:678-681, 1997Link, Google Scholar
13. Estroff SE, Swanson JW, Lachicotte WS, et al: Risk reconsidered: targets of violence in the social networks of people with serious psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology 33:S95-S101, 1988Google Scholar
14. Wessely S: Violence and psychosis, in Violence: Basic and Clinical Science. Edited by Thompson C, Cowen P. Oxford, England, Butterworth-Heinemann, 1993Google Scholar
15. Angermeyer MC, Cooper B, Link BG: Mental disorder and violence: results of epidemiological studies in the era of de-institutionalization. Social Psychiatry and Psychiatric Epidemiology 33:S1-S6, 1998Google Scholar
16. Arboleda-Flórez JE: An epidemiological study of mental illness in a remanded population and the relationship between mental condition and criminality. Ph.D. dissertation. University of Calgary, Department of Community Health Sciences, Alberta, Canada, 1994Google Scholar
17. Arboleda-Flórez JE, Love EJ, Fick G, et al: An epidemiological study of mental illness in a remanded population. International Medical Journal 2:113-126, 1995Google Scholar
18. Holley HL, Arboleda-Flórez J, Love EJ: Lifetime prevalence of prior suicide attempts in a remanded population and relationship to current mental illness. International Journal of Offender Therapy and Comparative Criminology 39:191-209, 1995Crossref, Google Scholar
19. Spitzer RL, Williams JBW, Gibbon M, et al: Structured clinical interview for DSM-III-R. Washington, DC, American Psychiatric Press, 1990Google Scholar
20. Hare R: A research scale for the assessment of psychopathy in criminal populations. Personality and Individual Differences 1:111-119, 1980Crossref, Google Scholar
21. Last JM: A Dictionary of Epidemiology, 3rd ed. Toronto, Oxford University Press, 1995Google Scholar
22. Allodi F, Kedward HB, Robertson M: Insane but guilty: psychiatric patients in jail. Canada's Mental Health 25:3-7, 1977Medline, Google Scholar
23. Bland RC, Newman SC, Dyck RJ, et al: Prevalence of psychiatric disorders and suicide attempts in a prison population. Canadian Journal of Psychiatry 35:407-413, 1990.Crossref, Medline, Google Scholar
24. Hodgins S, Coté G: Prevalence of mental disorders among penitentiary inmates in Quebec. Canada's Mental Health 38:1-4, 1990Google Scholar
25. Swank GE, Winer D: Occurrence of psychiatric disorder in a county jail population. American Journal of Psychiatry 133:1331-1333, 1976Link, Google Scholar
26. Whitmer GE: From hospitals to jails: the fate of California's deinstitutionalized mentally ill. American Journal of Orthopsychiatry 50:65-75, 1980Crossref, Medline, Google Scholar
27. Abram KM: The effect of co-occurring disorders on criminal careers: interaction of antisocial personality, alcoholism, and drug disorders. International Journal of Law and Psychiatry 12:133-148, 1989Crossref, Medline, Google Scholar
28. Teplin LA: The prevalence of severe mental disorder among male urban jail detainees: comparison with the Epidemiologic Catchment Area program. American Journal of Public Health 80:663-669, 1990Crossref, Medline, Google Scholar
29. Taylor PJ, Gunn J: Violence and psychosis: I. risk of violence among psychotic men. British Medical Journal 288:1945-1949, 1984Crossref, Medline, Google Scholar
30. Watt F, Tomison A, Torpy D: The prevalence of psychiatric disorder in a male remand population: a pilot study. Journal of Forensic Psychiatry 4:75-83, 1993Crossref, Google Scholar
31. Regier DA, Boyd JH, Burke JD, et al: One-month prevalence of mental disorders in the United States based on five Epidemiologic Catchment Area sites. Archives of General Psychiatry 45:977-986, 1988Crossref, Medline, Google Scholar
32. Bland RC, Orn H, Newman SC: Lifetime prevalence of psychiatric disorders in Edmonton. Acta Psychiatrica Scandanavica 77(suppl 338):24-42, 1988Google Scholar
33. Robins LN, Helzer JE, Weissman MM, et al: Lifetime prevalence of specific psychiatric disorders in three sites. Archives of General Psychiatry 41:949-958, 1984Crossref, Medline, Google Scholar
34. Modestin J: Criminal and violent behavior in schizophrenic patients: an overview. Psychiatry and Clinical Neurosciences 52:547-554, 1998Crossref, Medline, Google Scholar
35. Wessely S: The Camberwell study of crime and schizophrenia. Social Psychiatry and Psychiatric Epidemiology 33:S24-S28, 1998Google Scholar
36. Monahan J, Steadman H: Crime and mental illness: an epidemiological approach, in Crime and Justice, vol 4. Edited by Morris N, Tonry M. Chicago, University of Chicago Press, 1983Google Scholar
37. Marzuk PM: Violence, crime, and mental illness: how strong a link? Archives of General Psychiatry 53:481-486, 1996Google Scholar



