Prevention and Management of Aggression Training and Violent Incidents on U.K. Acute Psychiatric Wards
For some time concern has been rising about patient violence on psychiatric wards. It has been estimated that nursing staff have a 10 percent risk of being subject to a physically violent attack during the course of one year ( 1 ). Although a majority of such attacks result in little or no physical injury, psychological responses can be significant, with reports of consequent anger, anxiety, symptoms of posttraumatic stress disorder, guilt, self-blame, and shame ( 2 ). There have been additional concerns about injuries to patients during the management of violent incidents, particularly concerns about manual restraint-related deaths ( 3 , 4 ).
These concerns have led to the development and implementation of courses for nursing staff on the Prevention and Management of Violence and Aggression (PMVA). These courses consist of theoretical material on factors influencing aggression and signs of imminent violence; discussions pertaining to when restraint can be legally used; teaching breakaway techniques; and teaching manual restraint techniques performed by a three-person team, utilizing pain-free holds based on leverage. In most cases the use of manual restraint involves taking the patient down to the floor in a controlled manner, where he or she is held until treatment is administered and the patient is calm. In the United Kingdom such courses originated within the prison system and were then imported into general psychiatry, with modifications, by way of forensic psychiatric hospitals ( 5 ). Such training is often referred to as "control and restraint" and appears to be the dominant form of training in the United Kingdom, although many other types and variations are also in use. More recently, such courses have become mandatory for U.K. psychiatric service providers ( 6 ).
Few published data exist on the frequency of use of manual restraint in the United Kingdom, with one study ( 7 ) suggesting a rate of eight times per year on an average ward in order to manage aggressive behavior. However, the three hospitals in which this study took place did not routinely collect information on the use of manual restraints, nor is it easy to distinguish manual restraint from lower-level coercion, which includes single arm holds, physical guiding of the patient to another area, and blocking the patient's pathway ( 8 ). In the United Kingdom, manual restraint is used throughout psychiatric services, seclusion is used in only 70 percent of acute wards nationally ( 9 ), and mechanical restraint is not used at all.
The evaluation of PMVA courses has not been rigorous. No randomized controlled trials of manual restraint techniques have been conducted ( 10 ). A number of studies have shown that staff feel safer and more confident in dealing with aggressive situations after training ( 11 , 12 , 13 ); however, this is not the same as demonstrating that violent incidents are subsequently prevented or better managed. There is surprisingly few peer-reviewed outcome data on the effects of training. Reductions in incident rates and injuries after the introduction of training courses have been reported by some ( 14 , 15 , 16 , 17 ). Others have reported no change in incident rates and an increase in injuries after the implementation of a course ( 18 ) or have reported no reduction in incidents for staff who were trained, compared with a control group of staff who did not take the training course ( 13 ). The most rigorous trial conducted so far found no convincing effect of training on aggression frequency ( 19 , 20 ). No previous study has used a longitudinal design to evaluate the outcome of PMVA training, although one provided graphs for one ward over a 31-month period showing decreases in aggression frequency once a threshold had been achieved of 60 percent of staff trained ( 17 ).
Data reported in this article were gathered as part of the Tompkins Acute Ward Study, a longitudinal research project investigating care on acute psychiatric wards by using qualitative and quantitative methods. The study aimed to illuminate links between rates of conflict and containment, staff characteristics, and multi-disciplinary relationships. The purpose of this study was to explore the relationship between the delivery of PMVA training to nursing staff and officially reported violent incident rates through retrospective analysis of official records.
Methods
Sample
Data were drawn from official reporting systems of one psychiatric service provider in London, United Kingdom. A total of 5,384 admissions on 14 acute psychiatric wards at three hospital sites were included in the sample. One was a female-only ward, a second served as an assessment ward, the remainder were mixed-gender wards serving specific localities. The period covered by our data was from April 2002 to November 2004, approximately two and a half years.
Data collection
Data on adverse incidents are routinely collected by using nursing reports, which are entered in a proprietary computer system. We were provided with the dates and wards of all incidents falling into the following categories: verbal abuse, property damage, physical assault, self-harm, and absconding. One hospital in our sample commenced using the proprietary incident recording system in September 2003, so for the five wards in this hospital, data are less comprehensive. Also, the assessment ward in another hospital closed in mid-2003. For the remaining eight wards, data covering the full study period were available.
PMVA training has been given to all nursing staff in the study district for many years. A team of two trainers provided the courses over the study period. Courses consisted of either a five-day foundation course or a one-day annual update course. The five-day course covered the prediction, anticipation, and prevention of violence; reporting requirements; the role of personal, environmental, and organizational factors in violence reduction; responses to aggression, involving deescalation, communication skills, problem solving, and negotiation; and the principles and practice of breakaway and manual-restraint skills. Update courses covered manual-restraint skills only. The current PMVA trainers made available to us full training records for all wards for the full study period.
Permission to access and use these sources of data was provided by the National Health Service Trust managers and by the local research ethics committee. Hospital names have been changed to preserve anonymity.
Data analysis
Upon receipt, data were screened for outliers and obvious errors, which were checked against other sources of information and corrected or removed. All data were then imported into a database program and collated by using structured query language. The data were then exported as text files and imported into STATA version 8 for statistical analysis. The basic form of these data was incident and training counts by week by ward. Poisson regression was used, as this is particularly appropriate for the analysis of event counts over time.
Two different time frames were applied: four-week periods and weeks. Four-week periods smooth out daily and weekly variation caused by other factors and were used to assess relationships between variables over longer intervals of time. Weekly data were used to conduct a finer-grained analysis of short-term influences.
The number of occupied bed-days was used as the exposure variable, compensating in the analysis for week-to-week fluctuations in the numbers of patients present on the wards. The effect of incidents on training was assessed by regressing lags of incident rates on counts of attendance of the PMVA courses—for example, the number of physically aggressive incidents in one month was related to the following month's number of staff in training courses. A similar method was used to assess the effect of training on incidents—for example, the number of staff attending the PMVA courses in one month was related to the following month's number of verbally aggressive incidents. After initial analysis, each least significant variable was then removed sequentially, until only significant variables were in the model. Adjusted R 2 values were calculated for each model, and incident rate ratios (IRR) are provided as a guide to effect sizes.
Results
Incident rates and fluctuations over time
Data on both aggressive incidents and PMVA training were available for 1,404 ward-weeks. Mean weekly rates are shown in Table 1 . During the study period there were 226 incidents of verbal aggression, 88 incidents of property damage, and 370 incidents of physical aggression; 144 ward staff attended five-day PMVA courses, and 168 attended updates. These figures equate to roughly one incident of physical aggression per ward per four weeks and one staff per ward attending a PMVA course every five weeks.
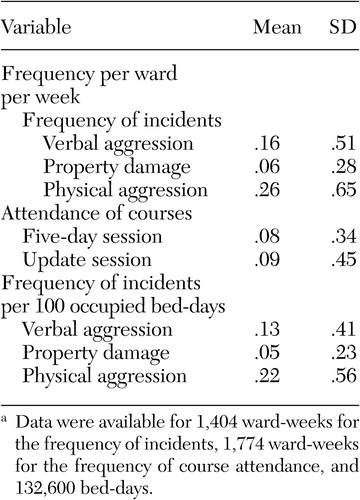 |
a Data were available for 1,404 ward-weeks for the frequency of incidents, 1,774 ward-weeks for the frequency of course attendance, and 132,600 bed-days.
Refuge Hospital joined the central incident recording system in 2003, and incidents peaked in summer 2004 then declined. A similar peak occurred at Haven Hospital during late 2002, thereafter evening out at a mean of one aggressive incident per week. The Shelter Hospital rate seems to have fluctuated more, with a higher mean of two incidents per week. Overall, there was no trend toward an increase or decrease in aggression over the study period.
Associations within four-week periods
The relationship between training and aggression was explored by examining the association of aggression to training in the months after the incident and the relationship between training and aggression in the months after the training course. This analysis was conducted for each type of violence and each type of PMVA course (five-day course or update), using lags of one, two, and three months.
With respect to aggression leading to course attendance, property damage in the month before the course (IRR=1.38, p=.021) and physical violence during the month of the course (IRR=1.16, p=.03) were associated with greater attendance of the five-day PMVA course; physical violence three months before the course (IRR=.78, p=.012) was associated with less course attendance (adjusted R 2 =.029). This means that for every one incident of property damage in the month before the course, there was a 38 percent increase in course attendances; for every one incident of physical violence during the month of the course, the rate of course attendance increased by 16 percent, and for every incident of physical violence three months before the course, the attendance rate decreased by 22 percent.
With respect to aggression leading to attendance of the PMVA update course, verbal aggression at one (IRR=1.13, p=.049) and two (IRR= 1.20, p= .003) months before the update course was associated with greater attendance; property damage at one (IRR=.58, p=.009) and three (IRR=.60, p=.015) months before the course was associated with less attendance (adjusted R 2 =.036). These findings provide some limited support for the idea that aggression in the months before courses prompts greater attendance, but the pattern of results is inconsistent and therefore unconvincing.
Course attendance also had discernible effects upon incident rates in the months that followed. Greater physical aggression was associated with attendance of the update course in the month before the incident (IRR=1.17, p<.001, adjusted R 2 = .016). Greater verbal aggression was associated with attendance of the update course two months before the incident (IRR=1.13, p=.026). However, less verbal aggression was associated with attendance of the update course in the month before (IRR=.79, p= .019, adjusted R 2 =.013). There was no relationship between rates of property damage and previous course attendance. Again these results are inconsistent and provide little support for the idea that course attendance leads to substantive decreases in aggression rates over several months.
Associations within weeks
A similar analysis was therefore conducted at the level of ward-weeks, exploring the relationships between aggression and training courses by using lags of one, two, three, and four weeks. Greater attendance of the five-day course was associated with physical violence three weeks before the course (IRR=1.29, p=.019) and the week of the course (IRR=1.43, p<.001, adjusted R 2 =.018).
With respect to aggression leading to attendance of the update course, verbal aggression four weeks before the course (IRR=1.32, p=.031) and in the week of the course (IRR=1.33, p=.011) were associated with higher attendance of the course; physical violence three weeks before the course (IRR=.65, p=.023) was associated with lower attendance (adjusted R 2 =.014). Again, there were some indications of aggression prompting course attendance, but no consistent picture emerges. However, what does stand out clearly is that when regular staff leave the wards to attend the five-day course, there seems to be an increase in physical violence on the wards.
The impact of course attendance on aggression in the weeks after the course is clearer. Greater physical aggression was associated with attendance of the PMVA update course three weeks (IRR=1.17, p=.04) and four weeks (IRR=1.20, p=.019) before and with attendance of the five-day course (IRR=1.50, p<.001) in the same week (adjusted R 2 =.012). There was also a trend toward an association between greater physical aggression and attendance of the update course in the preceding week. For verbal aggression, greater frequency was associated with attendance of the five-day course (IRR=1.34, p=.042) and the update course (IRR=1.21, p=.038) in the same week (adjusted R 2 =.005). Rates of property damage had no relationship to attendance of the PMVA courses in the preceding weeks. These findings suggest that PMVA update courses might precipitate a short-term increase in physical violence.
Discussion
Our data covering a period of nearly three years provide no indication that violent incident rates are rising in any of the wards studied. Steeply rising trends were reported in a comparable London hospital during the 1980s ( 21 ). Comparisons are not easy to make because of differences in ward types, but it would appear that had those trends continued, our data should have shown rates of two violent incidents per ward per week. Instead, the rate of incidents in our study was .26 per ward per week. There is little hard evidence that violent incidents on psychiatric wards are increasing in the United Kingdom.
The finding of a positive correlation between training and aggressive incidents is an unwelcome result. We had hoped to identify reductions in aggression after course attendance. Theoretical discussions and previous work had suggested that greater technical mastery in the interpersonal management of aroused patients, coupled with a calm and confident demeanor on the part of staff, would together lead to more frequent resolution of tense situations without violence ( 22 ). Such training should have its greatest impact just after it has been completed, with its effect gradually attenuating thereafter. Instead, the results point in the other direction, with update courses apparently triggering small rises in physical violence. In addition, course attendance takes staff away from the ward, which stimulates more violence while they are away.
These results are based on officially reported data and should be accepted with caution. Official data are subject to a number of different influences (for example, the concerns of managers and the constant changes in policy in the U.K. health service). Official statistics on violence are notorious for being lower than real rates, because of underreporting ( 23 ). It is therefore possible that the relationships that we have found are a product of chance or that course attendance stimulated an increase in reporting. Alternatively, course attendance may have stimulated an increase in reporting. However, if this were the case, rates of verbal abuse and property damage should also have increased after staff attended the update course, and similar (possibly even larger) increases should have occurred after the five-day course. Neither of these relationships was evident in our data.
Another potential explanation is that local circumstances have produced anomalous results. Although PMVA courses in general elsewhere may produce the drop in incident rates that we had anticipated, either the local content or teaching delivery may have led to the opposite effect. However, we have no evidence or reason to believe this. The course content is fairly standard, and the local trainers who deliver it are qualified, experienced, and competent. Alternatively, the effect may have been produced by the combination of the course with local service characteristics. The acute wards in this study suffer from staff shortages. Although data are not available for the whole period of the study, for most of 2004 the mean vacancy rate for nursing staff positions was 24 percent. This may explain the increase in incidents when staff were away at the PMVA training courses, on the grounds that any strain on this fragile staffing situation had negative consequences. In our study we found that among nursing staff, approximately 10 percent of all leave taken was for attendance of PMVA courses. Vacancy rates may also have contributed in some way to the rise in incidents after the update courses. However, we are unable to explain why this might happen and why the effect is specific only to the update course but not the five-day course.
The most favorable view that can be taken in light of the failure to find a drop in incident rates after training is that the culture of violence prevention in the locality is in a steady state. Further training keeps violence at a low level, rather than lowering it from a high level. The discrepancy between our findings and those of some previous studies could thus be due to the occurrence of a maximal impact on violent incident rates only when training is first introduced. Violent incidents in the study district may have been reduced some years before when training was first introduced and stayed low as the training continued. This interpretation would be supported by data showing sustained decreases in incident rates once a 60 percent threshold in trained staff had been achieved ( 17 ).
Alternatively, the early impact of training on aggression rates may be a "Hawthorne effect," caused by novelty, which could wear off in the longer term. The most negative interpretation is that training in the management of aggression makes staff more confident and more likely to confront patients, elicit a violent response, and use the manual restraint techniques that they have been taught ( 24 ). It may be that such a response occurs only with more superficial training, thus the rise in violence after the update course rather than the five-day course. It is perhaps noteworthy that in the study district, update courses concentrate solely on violence management skills and do not refresh participants' knowledge of violence prevention and deescalation.
Conclusions
Analyses of this longitudinal data set of official reports showed a positive association between PMVA training and violent incident rates. Findings provide weak evidence that aggressive incident rates prompt course attendance, no evidence that course attendance (either the five-day course or the update course) reduced violence in the short or long term, and some evidence that the update course triggered short-term (four weeks) rises in rates of physical aggression. In addition, the data show that course attendance led to a significant rise in physical and verbal aggression on the ward while staff were away.
The evidence regarding the efficacy of PMVA training in reducing rates of aggression is finely balanced. Although some reported studies are positive, in most cases the methodologies used have not been highly rigorous, with nearly all being uncontrolled natural experiments. Assessing this evidence is complicated by variation in training course content, delivery, and duration. Our results raise questions about the necessity for annual updates, but further research is clearly required before any changes in policy are considered.
Even if such courses do not prevent aggression, they may still have value for the skills that they teach in safe manual restraint techniques. However, there remains a paucity of evidence on outcome in terms of staff and patient injuries, as well as prevention of violence and aggression. We clearly need to know more about the effect of differing course content and identify what types of teaching and management lead, and do not lead, to the successful prevention of violent and aggressive incidents.
Acknowledgments
Funding from the Tompkins Foundation and the Department of Health supported this research. The views expressed in this publication are those of the authors and not necessarily those of the funding bodies.
1. Healthcare Commission: Healthcare Commission NHS National Staff Survey 2004: Summary of Key Findings. London, Commission for Healthcare Audit and Inspection, 2005Google Scholar
2. Needham I, Abderbalden C, Halfens R, et al: Non-somatic effects of patient aggression on nurses: a systematic review. Journal of Advanced Nursing 49:283-296, 2005Google Scholar
3. Paterson B, Bradley P, Stark C, et al: Deaths associated with restraint use in health and social care in the UK. The results of a preliminary survey. Journal of Psychiatric and Mental Health Nursing 10:3-15, 2003Google Scholar
4. Blofeld J, Sallah D, Sashidharan SP, et al: Independent inquiry into the death of David Bennett. Cambridge, Norfolk, Suffolk and Cambridgeshire Strategic Health Authority, 2003Google Scholar
5. Wright S: Physical restraint in the management of violence and aggression in in-patient settings: a review of issues. Journal of Mental Health 8:459-472, 1999Google Scholar
6. Mental Health Policy Implementation Guide: Developing Positive Practice to Support the Safe and Therapeutic Management of Aggression and Violence in Mental Health In-patient Settings. Leeds, National Institute for Mental Health in England, Department of Health, 2004Google Scholar
7. Duff L, Gray R, Brostor F: The use of control and restraint techniques in acute psychiatric units. Psychiatric Care 3:230-234, 1996Google Scholar
8. Ryan CJ, Bowers L: Coercive maneuvers in a psychiatric intensive care unit. Journal of Psychiatric and Mental Health Nursing 12:695-702, 2005Google Scholar
9. Garcia I, Kennett C, Quraishi M, et al: Acute Care 2004: A National Survey of Adult Psychiatric Wards in England. London, Sainsbury Centre for Mental Health, 2005Google Scholar
10. Sailas E, Fenton M: Seclusion and restraint for people with serious mental illnesses. Cochrane Database of Systematic Reviews, 1st Quarter, 2005Google Scholar
11. Beech B, Leather P: Evaluating a management of aggression unit for student nurses. Journal of Advanced Nursing 44:603-612, 2004Google Scholar
12. Collins J: Nurses' attitudes towards aggressive behaviour, following attendance at "The Prevention and Management of Aggressive Behaviour Programme." Journal of Advanced Nursing 20:117-131, 1994Google Scholar
13. Van Rixtel A, Nijman H, Jansen G: Aggression and psychiatry. Does training have any effect? [in Dutch] Verpleegkunde 12:111-119, 1997Google Scholar
14. Gertz B: Training for prevention of assaultive behavior in a psychiatric setting. Hospital and Community Psychiatry 31:628-630, 1980Google Scholar
15. St Thomas Psychiatric Hospital: A program for the prevention and management of disturbed behavior. Hospital and Community Psychiatry 27:724-727, 1976Google Scholar
16. Carmel MD, Hunter M: Compliance with training in managing assaultive behavior and injuries from inpatient violence. Hospital and Community Psychiatry 41:558-560: 1990Google Scholar
17. Mortimer A: Reducing violence on a secure ward. Psychiatric Bulletin 19:605-608, 1995Google Scholar
18. Parkes J: Control and restraint training: a study of its effectiveness in a medium secure psychiatric unit. Journal of Forensic Psychiatry 7:525-534, 1996Google Scholar
19. Needham I, Abderhalden C, Meer R, et al: The effectiveness of two interventions in the management of patient violence in acute mental inpatient settings: report on a pilot study. Journal of Psychiatric and Mental Health Nursing 11:595-601, 2004Google Scholar
20. Needham I: A Nursing Intervention to Handle Patient Aggression: The Effectiveness of a Training Course in the Management of Aggression. Maastricht, the Netherlands, Maastricht University, 2004Google Scholar
21. Noble P, Rodger S: Violence by psychiatric in-patients. British Journal of Psychiatry 155:384-390, 1989Google Scholar
22. Bowers L: Dangerous and Severe Personality Disorder: Response and Role of the Psychiatric Team. London, Routledge, 2002Google Scholar
23. Lion JR, Snyder W, Merrill GL: Under-reporting of assaults on staff in a state hospital. Hospital and Community Psychiatry 32:497-498, 1981Google Scholar
24. Morrison EF: The tradition of toughness: a study of nonprofessional nursing care in psychiatric settings. Journal of Nursing Scholarship 22:32-38, 1990Google Scholar



