Utilization and Outcome in an Overnight Psychiatric Observation Program at a Veterans Affairs Medical Center
Abstract
OBJECTIVE: The effectiveness of an overnight psychiatric observation program was evaluated. The program was designed to avoid unnecessary hospitalization of patients experiencing acute psychiatric crises. METHODS: Of 110 patients admitted to the observation unit at a Veterans Affairs medical center over a six-month period in 1996, the charts of 92 patients were retrospectively reviewed. Characteristics of patients referred to the program were documented, inpatient hospitalization rates and suicide rates in the six-month periods before and after admission to the observation unit were examined, and variables related to the need for hospitalization immediately after observation were explored. RESULTS: Most of the 92 patients (98 percent) were referred from the medical center's emergency room. At the time of observation, 80 percent of the patients were unemployed, 55 percent expressed suicidal or homicidal ideation, 49 percent were intoxicated or at risk for alcohol withdrawal, and 41 percent were homeless. The most frequent psychiatric diagnosis was substance abuse or dependence (77 percent). The large majority of patients (88 percent) were referred the next day to other outpatient programs for follow-up and treatment, which avoided costly inpatient treatment. In the six months before admission to the observation program, the mean number of inpatient psychiatric bed days was 9.8, compared with 2.7 days in the six-month period after discharge from the observation program. No increase in suicide gestures or attempts was noted among the patients. No variables significantly predicted admission to inpatient care after the observation period. CONCLUSIONS: Overnight observation programs may provide a cost-effective alternative to traditional inpatient treatment for some individuals with psychiatric disorders.
The delivery of mental health services in this country has changed dramatically in the last decade. The change has been mostly driven by a need to control costs. Inpatient care is the costliest of all services and has repeatedly been shown to constitute the most significant portion of both psychiatric and total health care budgets (1).
In support of this cost-containment effort are numerous studies that have demonstrated that shorter inpatient stays have several advantages for patients, such as increasing patients' independence, maintaining them in their own environments, decreasing their symptoms, linking patients with community resources, and increasing patients' satisfaction with treatment (2,3). As a result, a primary focus of the new health care system has been to reduce the use of inpatient mental health services while increasing the use of outpatient services.
Two primary approaches have been examined in the attempt to reduce the utilization of inpatient mental health services. The most frequently studied are crisis hospitalization programs (3,4,5). These programs typically use a designated short length of stay to design a treatment plan that can be applied on an outpatient basis immediately on discharge. Several studies have suggested that most patients admitted to these programs showed improvement in the severity of their psychiatric symptoms, were able to be discharged in the designated time frame, expressed high satisfaction with the program (6), and had a low rehospitalization rate (2).
For example, Gillig and colleagues (7) reported that the 30-day readmission rate after a 24-hour inpatient program was 7.5 percent. However, other authors have reported high readmission rates. Schneider and Ross (6) reported that the 30-day readmission rate after a three-day inpatient program for severely mentally ill patients was 14.6 percent. Weisman and colleagues (5) reported a six-month readmission rate of 16 percent after a three-day hospitalization program. Two more studies have also shown that a decreased length of stay was associated with an increased readmission rate (8), particularly for patients with psychotic disorders (9).
Others have found no difference in readmission rates between patients treated in ultra-short hospitalization programs and those treated in traditional inpatient services (6). However, few studies have examined any other adverse or problematic outcomes after admission to the units. Jayaram and colleagues (2) emphasized the importance of measuring suicide as a negative outcome.
A second approach to reducing inpatient psychiatric services has been the use of very-short-stay observation periods of 24 hours or less. Unfortunately, little research has examined the use of observation periods. However, Gillig and associates (7) compared two psychiatric emergency services and found that the service with the 24-hour emergency evaluation unit had a significantly lower rate of hospital admissions (36 percent) than the one without the unit (52 percent). Clinicians in the program reported that 65 of the 134 patients admitted to the observation unit would have been admitted to the hospital if the unit had not been available.
In this paper we report descriptive and predictive data from an uncontrolled study of an overnight (23 hours or less) observation and stabilization program instituted in a large metropolitan Veterans Affairs hospital. The observation program was staffed by a clinical nurse specialist (three-quarter time), a psychiatry resident (half time), and an attending psychiatrist (one-quarter time). Because the observation beds were located on an inpatient psychiatric unit, existing nursing staff provided the nursing care needed.
The purpose of the study was to provide information on characteristics of patients referred to the program, examine inpatient hospitalization rates and suicide rates before and after observation, and explore variables related to the need for hospitalization immediately after observation.
Methods
The sample consisted of patients consecutively admitted to the observation program during the six-month period from February through July 1996. To be admitted to the program, a patient had to exhibit psychiatric symptoms, such as acute anxiety, mood instability, acute extrapyramidal symptoms, suicidal or homicidal ideation, and intoxication from alcohol or drugs or acute withdrawal symptoms; to be in crisis; and to need further evaluation or stabilization. In every case a less restrictive treatment option was judged to be inadequate. Patients who were medically unstable or judged to be inappropriate for outpatient care within 24 hours, such as those who were acutely psychotic, were excluded.
After the patient was admitted to an observation bed, he or she was interviewed by the resident physician who obtained a history, completed a physical exam, and ordered the appropriate laboratory tests and admission orders. The patient was then seen the next morning by the entire team, and a plan for care was discussed with the patient.
Information about each patient's stay on the observation unit was recorded during the admission. All other information used as outcome data, including use of hospital resources and significant clinical events, was obtained from a retrospective chart audit of two time periods—the six months before and the six months after the patient's admission to the observation program.
Results
During the six-month study, 110 patients were referred to the observation program, an average of 18.3 patients per month. Before the existence of the observation program these patients would typically have been admitted to inpatient units. The patients' use of inpatient resources in the preceding six months was substantial, with more than half having been admitted to psychiatric or medical units. During the same six months, an average of 97.2 patients per month were also admitted to inpatient psychiatric units.
Most of the patients admitted to the observation program (108 patients, or 98 percent) were referred from the VA medical center's emergency room. Because some records were transferred to other hospitals, satellite clinics, and administrative offices in the VA healthcare system, complete hospital records were available for review for 92 of the 110 patients (84 percent).
The mean±SD age of the sample, which was composed of 90 men and two women, was 43.9±8.2 years, with a range from 24 to 69 years. At the time of observation, 38 patients (41 percent) were homeless, 45 (49 percent) were intoxicated or at risk of alcohol withdrawal, 51 (55 percent) expressed suicidal ideation, and 74 (80 percent) were unemployed. The most frequent psychiatric diagnosis was substance abuse or dependence (71 patients, or 77 percent). Table 1 summarizes the characteristics of the 92 patients at the time of admission to the observation program.
Of the 18 veterans whose charts were unavailable, 14 were men and four were women, with an average age of 44 years. The most frequent psychiatric diagnosis in this group was also substance abuse or dependence (12 patients, or 67 percent). No significant differences were found between the 18 patients and the 92 patients in age or frequency of substance use diagnoses.
Of the 92 patients whose charts were available, 35 (38 percent) had been admitted at least once to an inpatient psychiatric unit in the past six months, and eight (9 percent) had been admitted at least once to a medical-surgical or rehabilitation inpatient unit in the same time period. Another seven patients (8 percent) were admitted to both psychiatric and medical-surgical or rehabilitation inpatient units during the six months before admission to the observation program. No significant association was found between the two types of admissions.
On average, before admission to the observation unit, patients in this sample each received 9.8 days of psychiatric inpatient care and .9 days of medical-surgical or rehabilitation inpatient care. For 11 of the 92 patients (12 percent), the disposition at the end of the observation period was admission to one of the medical center's two inpatient psychiatric units; the remaining 81 patients (88 percent) were discharged to an outpatient setting. More specifically, 32 percent of the discharged patients were referred to our VA mental health clinic, 23 percent to our VA alcohol and drug abuse treatment program, 16 percent to long-term community substance abuse treatment programs, 15 percent to homeless shelters, 4 percent to an outlying VA clinic, and 3 percent to our medical clinics. The remaining patients were referred to other settings or refused referral.
The number of inpatient days in the previous six months did not differentiate between patients admitted to inpatient care and those discharged to outpatient care, for either psychiatric admissions or admissions to medical-surgical or rehabilitation units.
Concerns about an increase in suicide rates in the period after discharge from the observation unit were alleviated. Examination of the patients' records revealed a very low frequency of suicide attempts in the months before and after admission to the observation unit, precluding any statistical analysis. Only one patient attempted suicide in the postdischarge period; three patients attempted suicide in the period before admission.
To determine predictors of admission to inpatient care immediately after the observation period, we conducted a logistic regression analysis, using a forward stepwise entry procedure. In this procedure variables enter the logistic regression equation in order of size of contribution. The Wald statistic, set at a probability value of .05, was used as a criterion to determine whether a variable would enter the analysis. The following variables were examined as predictors: number of days of inpatient psychiatric care in the previous six months, history of past suicide attempts, the time of day in which the patient presented to the emergency room, a diagnosis of substance abuse or dependence, the presence of suicidal ideation at the time of admission to the observation unit, and intoxication symptoms when presenting to the emergency room. No variable was a significant predictor of disposition to inpatient or outpatient care after the observation period.
In the six-month postobservation period, 20 of the 92 patients were admitted to an inpatient psychiatric unit, and six patients were admitted to an inpatient medical-surgical or rehabilitation unit. Three patients were admitted to both types of unit. No significant association was found between the two types of admissions. A significantly larger proportion of the patients were admitted to a psychiatric unit before the observation period than after (42 versus 23 patients; χ2=16.88, df=1, p<.001). A similar analysis revealed no change over the two time periods in the proportion of the sample admitted to medical-surgical or rehabilitation units.
The mean±SD number of days in inpatient psychiatric treatment decreased significantly, from 9.8±16.2 days in the preobservation period to 2.7±7.9 days in the postobservation period (t=4.59, df=91, p<.001). No significant change was found in the mean number of days of inpatient treatment in medical-surgical or rehabilitation units (.9±2.8 days in the preobservation period and .7±3.9 in the postobservation period). Patients who were admitted to inpatient care after the observation period did not differ from patients discharged to outpatient care in the mean number of days in inpatient psychiatric treatment or treatment in medical-surgical or rehabilitation units.
A final analysis attempted to determine if other variables could predict the number of readmissions in the six months after the observation period. The variables included number of inpatient psychiatric days in the past six months, past history of a suicide attempt, intoxication when presenting to the emergency room, suicidal ideation during the observation period, inpatient or outpatient status at the end of the observation period, and service-connected status—that is, whether the patient was receiving a pension for illness or injury sustained during a tour of duty in the military. For this analysis we used multiple linear regression, employing a stepwise method of entry of predictor variables.
The number of days of inpatient psychiatric care in the previous six months entered the regression equation on the first step (F=19.40, df=1,90, p<.001, R=.42) and explained 17.7 percent of variance in the number of days in inpatient psychiatric care in the postobservation period. No other variable entered the equation at step two, indicating that the other predictors did not significantly increase the predicted variance in the number of days in inpatient psychiatric care in the postobservation period.
Discussion and conclusions
The results of this study are relatively straightforward. The response to our establishment of an observation program was notable, resulting in an average of almost 20 patient referrals per month, which represented the equivalent of 19 percent of monthly inpatient psychiatric admissions. The majority of the patients admitted for observation had acute psychiatric and socioeconomic problems. Most were referred from the emergency room, and most were intoxicated, unemployed, and homeless, with suicidal ideation.
The patients' use of inpatient resources in the preceding six months was substantial, with more than half having been admitted to psychiatric or medical units. The immediate impact of the program was apparent—only 12 percent of the patients were admitted to inpatient care after observation. This low rate was achieved with the help of a few factors. The clinical nurse specialist assigned to this program is very active in reviewing patients' records for any available collateral information and available social or family resources. She also actively explores referral options as early as possible after the patient is admitted for observation. Patients with substance use disorders can be evaluated within 24 hours by the alcohol and drug abuse treatment program staff, who will make appropriate treatment recommendations. The Health Care for Homeless Veterans program is available in our medical center, and its staff members' knowledge of community resources has also been very helpful.
Finally, our staff begin to plan for follow-up care while they consider whether the patient should be admitted to the overnight observation program. The purpose of admission to the program is discussed with the patient, who is informed of the anticipated length of stay. Although we found no variables that predicted whether a patient would be admitted to inpatient care after the 23-hour observation period, patients who were admitted the next day to an inpatient bed were those who continued to have active suicidal ideation, those whose psychotic or depressive symptoms interfered with their ability to care for themselves, and those with continued active alcohol withdrawal symptoms, who were at risk for seizures or delirium tremens.
The long-term impact of the program was examined by comparing the number of inpatient treatment days in the six-month periods before and after discharge from the observation program. A significant reduction in psychiatric inpatient days after discharge was noted, without an increase in adverse outcomes such as suicide gestures or attempts. Furthermore, the number of inpatient days after discharge was found to be predicted in part by the number of inpatient days in the period before program admission.
Reasons for the decrease in inpatient services were not systematically explored as part of the study design. However, participating staff members hypothesized that the short duration of the observation period facilitated rapid decision making and referrals to outpatient programs, such as residential substance abuse treatment and partial hospitalization programs, and capitalized on the fact that a high level of distress often motivates patients to accept treatment programs that are immediately available.
This study was not immune to the shortcomings of an uncontrolled research design. In the absence of a control group, we cannot rule out the possibility that a similar sample of patients admitted to an inpatient unit would not have had a similar, or greater, reduction in inpatient days in the six months after discharge. In fact, during the year of the study, the average length of an inpatient stay dropped to 12.1 days from 15.3 days the previous year.
However, even assuming that a control sample with similar patient characteristics would have short inpatient stays of only three or four days, the overall impact of the program is difficult to discount because the program reduced subsequent inpatient days to an average length of stay of 2.7 days, which is lower than a brief inpatient stay. Thus an inpatient control group would have to eliminate subsequent inpatient days entirely for a similar overall economic effect to be realized. When this study was done, the average cost for a day of inpatient psychiatric care was $320. Therefore, even small reductions in the number of inpatient admissions translated into substantial cost savings.
Aside from limitations to generalization of the findings inherent in uncontrolled studies, we also note that findings from a VA population may not be generalizable to civilian patients. The clinical and economic benefit of observation programs such as ours would be clearer in future studies that include a control group. In such studies, patients who meet admission criteria to the observation program would be randomly assigned to either inpatient care or the observation program; they would be followed for six months to more carefully explore outcome data and predictors of inpatient status after the observation period.
Dr. Francis is assistant chief of mental health services, Ms. Carter is coordinator of the psychiatric observation program, Dr. Schinka is director of the neuropsychology clinic, and Dr. Ordorica is associate chief of staff of mental health services at James A. Haley Veterans Affairs Health Care System in Tampa, Florida, where Dr. Marchand was formerly a staff psychiatrist. Dr. Francis is also assistant professor, Dr. Schinka is associate professor, Dr. Feldman is resident, and Dr. Ordorica is associate professor in the department of psychiatry at the University of South Florida, where Dr. Hart was formerly chief resident. Dr. Marchand is now attending psychiatrist in the youth unit of Utah State Hospital in Provo. Dr. Hart is now staff psychiatrist at Mental Health Care, Inc., in Tampa. Send correspondence to Dr. Francis at the James A. Haley Veterans Affairs Health Care System, Mental Health and Behavioral Sciences Service (116A), 13000 Bruce B. Downs Boulevard, Tampa, Florida 33612 (e-mail, [email protected]). Portions of the data from this study were presented at the Institute on Psychiatric Services held October 24–28, 1997, in Washington, D.C.
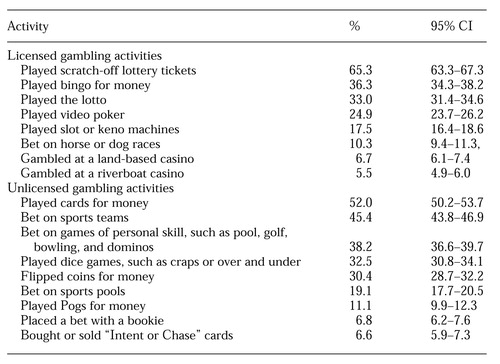 |
Table 1. Characteristics of 92 patients with acute psychiatric crises admitted for an overnight observation peried in a VA medical center
1. Addington DE, Jones B, Bloom D, et al: Reduction of hospital days in chronic schizophrenic patients treated with risperidone: a retrospective study. Clinical Therapeutics 15:917-926, 1993Medline, Google Scholar
2. Jayaram G, Tien AY, Sullivan P, et al: Elements of a successful short-stay inpatient psychiatric service. Psychiatric Services 47:407-412, 1996Link, Google Scholar
3. Breslow RE, Klinger BI, Erickson BJ: Crisis hospitalization on a psychiatric emergency service. General Hospital Psychiatry 15:307-315, 1993Crossref, Medline, Google Scholar
4. Rhine MW, Mayerson P: Crisis hospitalization within a psychiatric emergency service. American Journal of Psychiatry 127:122-130, 1971Link, Google Scholar
5. Weisman G, Feirstein A, Thomas C: Three day hospitalization: a model for intervention. Archives of General Psychiatry 21:620-629, 1969Crossref, Medline, Google Scholar
6. Schneider SE, Ross IM: Ultra-short hospitalization for severely mentally ill patients. Psychiatric Services 47:137-138, 1996Link, Google Scholar
7. Gillig PM, Hillard JR, Bell J, et al: The psychiatric emergency service holding area: effect on utilization of inpatient resources. American Journal of Psychiatry 146:369-372, 1989Link, Google Scholar
8. Appleby L, Luchins D, Desai P, et al: Length of inpatient stay and recidivism among patients with schizophrenia. Psychiatric Services 47:985-990, 1996Link, Google Scholar
9. Thomas M, Rosenberg S, Giese A, et al: Shortening length of stay without increasing recidivism on a university-affiliated inpatient unit. Psychiatric Services 47:996-998, 1996Link, Google Scholar



