Rehab Rounds: Cognitive-Behavioral Therapy and Clozapine for Clients With Treatment-Refractory Schizophrenia
Introduction by the column editors: The pervasive impairments in social, cognitive, affective, and daily functioning that are disabling for persons with schizophrenia require the integration of pharmacological and psychosocial interventions (1,2). In past Rehab Rounds columns, we have highlighted a variety of psychosocial interventions—social skills training, case management, and vocational rehabilitation—that have empirical validation and some level of acceptance among mental health providers in North America.
This month's Rehab Rounds focuses on cognitive-behavioral therapy, a psychotherapeutic intervention originally developed by Aaron Beck for depression and recently adapted for use with individuals with schizophrenia (3,4). Dr. Pinto and his colleagues from the treatment research unit of the Department of Mental Health of the Province of Naples in Pollena, Italy, present their rationale for using cognitive-behavioral therapy plus social skills training with this population and provide results of a randomized, controlled trial of cognitive-behavioral therapy for patients with treatment-refractory schizophrenia who were receiving clozapine.
Atypical antipsychotic medications have several advantages over conventional neuroleptic agents in the treatment of schizophrenia. The atypical antipsychotic medications induce fewer extrapyramidal side effects and are better able to ameliorate the cognitive deficits of individuals with schizophrenia (5). The salutary effects of atypical antipsychotics in these areas may allow individuals with schizophrenia to derive greater benefit from psychosocial interventions such as vocational rehabilitation, social skills training, and family psychoeducation, thereby extending the efficacy of the medications to the domains of social relationships, vocational functioning, and overall quality of life (6).
One psychosocial approach that may prove effective in the long-term management of schizophrenia is cognitive-behavioral therapy. Cognitive-behavioral therapy for schizophrenia addresses the dysfunctional information processing of individuals with this disorder.
For example, Perris (7) noted that clients' negative experiences and convictions about themselves often produce self-stigmatization and result in poor outcomes such as isolation and a lack of social competence. In his program, therapists encouraged clients to identify their negative self-views and world views, allowing more effective assumptions and behaviors to be gradually introduced. More recently, British researchers have used cognitive-behavioral therapy to help clients identify and manage psychotic symptoms (8). These techniques have been shown to help individuals with schizophrenia cope with residual delusions and hallucinations (9). However, none of these studies have attempted to combine cognitive-behavioral therapy with the newer, atypical antipsychotic agents.
In this report, we present findings from a study in which we randomly assigned clients with treatment-refractory schizophrenia who had recently started clozapine to receive either cognitive-behavioral therapy plus social skills training or individual supportive psychotherapy. Clients who were assigned to the experimental group received individual, one-hour sessions of cognitive-behavioral therapy weekly for six months.
Study design
Clients were selected for the study from among inpatients and outpatients who were consecutively referred to the program on atypcial antipsychotic drugs of the treatment research unit of the Department of Mental Health of the Province of Naples in Pollena, Italy. To be eligible for the study, clients had to have a DSM-IV diagnosis of schizophrenia, to show no evidence of current substance abuse or organic pathology, to have a treatment-refractory psychosis, and to provide informed consent. Evidence that the client had a treatment-refractory psychosis consisted of documentation of failure to respond to at least two previous neuroleptic drug trials, each at least six weeks in duration, at a dose of more than 600 mg per day of chlorpromazine equivalents.
The study took place between October 1996 and February 1998. Twenty clients were randomly assigned to the experimental condition to receive the cognitive-behavioral therapy plus social skills training, and 21 were assigned to supportive therapy. As Table 1 shows, the groups did not differ significantly on demographic or clinical history variables.
The initial cognitive-behavioral therapy session focused on facilitating engagement in treatment. Special efforts were made to foster the cooperation of clients who initially required hospitalization. For example, treatment was not begun until the client felt able to cope with the treatment program. The frequency and duration of the sessions were adapted flexibly to meet the individual needs of each client.
The early phase of treatment focused on building a therapeutic alliance within an empathic and cooperative atmosphere. After the clinical team obtained a detailed analysis of the client's problems, the stress-vulnerability paradigm was explained to the client. The aim of using this model was to change the clients' perspective of the illness from “symptoms to treat” to “problems to solve”.
Using individualized case formulations, clinicians implemented elements of cognitive-behavioral therapy or social skills training such as modeling, rehearsal, positive reinforcement, in vivo exercises, and homework assignments (10). Skills training methods were utilized to improve social behaviors including self-care, medication self-management, social conversation, interpersonal problem-solving, self-directed recreation, family communication, and management of personal resources.
Following the guidelines posed by Fowler and colleagues (11), specific interventions focused on improving clients' abilities to manage their current psychotic symptoms. The clients' own coping strategies were pointed out, and the behavioral and emotional consequences of psychotic symptoms were delineated. Maladaptive strategies for managing symptoms, such as social withdrawal, were discouraged, and more helpful ones, such as distraction and relaxation, were promoted.
Whenever possible, disputation of irrational beliefs related to delusions and hallucinations was tried. The therapist actively encouraged clients to talk about their understanding of psychotic symptoms. Clients were asked to demonstrate the justification of their beliefs, and then the therapist would propose an alternative explanation. The possible links between current symptoms and earlier real-life events were discovered. Reality testing was undertaken if feasible.
During treatment sessions, special effort was devoted to enhancing clients' abilities to identify and monitor their stress levels, based on the recognition that stressors may either exacerbate psychotic phenomena or provoke inappropriate behaviors. Furthermore, signs and symptoms that might precede psychotic relapse were examined. Therapists sought to improve clients' direct or indirect control over the sources of stress using coping methods such as appropriate avoidance, seeking help, and medication compliance.
Clients who were assigned to the comparison group received individual supportive therapy provided by a well-trained psychiatrist or psychologist. Supportive therapy sessions were provided for the same duration and frequency as the sessions of cognitive-behavioral therapy plus social skills training and included basic psychoeducation about the nature and the treatment of schizophrenia, active listening, empathy and reassurance, reinforcement of clients' health-promoting initiatives, help in managing crisis situations, and advocacy for clients' needs and preferences.
Monthly support meetings for family members were available for the families of clients in both groups. These meetings addressed the symptoms of schizophrenia, the effects of treatment with clozapine, and the progress of the client.
Demographic and clinical history information was assessed at baseline. All clients were assessed using the Brief Psychiatric Rating Scale (BPRS) (12), the Scale for the Assessment of Positive Symptoms (SAPS) (13), and the Scale for the Assessment of Negative Symptoms (SANS) (14) at baseline and after the intervention. Records were also kept on each client's dosage of clozapine, attendance at therapy sessions, and use of inpatient services.
Results
Outcome measures were analyzed using data from all clients who provided information at both baseline and post-intervention—19 clients in the experimental group and 18 clients in the comparison group. None of the clients relapsed or required rehospitalization during the course of the study. One subject in the cognitive-behavioral group did not complete the study; the client developed leukopenia, and clozapine was discontinued. In the supportive therapy group, two subjects withdrew because of refusal to participate further, and a third developed seizures and his clozapine was stopped.
As Table 2 shows, the two study groups did not differ in symptomatology at baseline. Both groups showed statistically significant improvement on the BPRS, SAPS, and SANS from baseline to postintervention. However, comparisons between the groups showed that at postintervention, clients who had received cognitive-behavioral therapy plus social skills training had lower BPRS and SAPS scores than the clients who received supportive therapy. No significant differences between treatment groups were found on SANS scores during either evaluation period.
Adherence to the therapeutic regimen was high in both groups, ranging between 75 and 85 percent, but the clients in the experimental group attended more sessions than the clients in the comparison group. At the end of the study, there was no significant difference between the groups in daily clozapine dose.
Case vignette
Mr. L, a 28-year-old high school graduate who had been an avid body builder and a successfully employed electrician, was diagnosed as having paranoid schizophrenia at age 20. Despite continuous treatment with conventional neuroleptic medications, he was hospitalized repeatedly and suffered from persistent psychotic symptoms, including visual and auditory hallucinations and mystical delusions. He was also depressed and had low self-esteem. He had not worked or socialized for several years, and he was completely dependent on his relatives for all his self-care needs.
Mr. L was started on clozapine and randomly assigned to the experimental condition of the study. In the first phase of therapy, Mr. L was helped to express his needs and to formulate a list of problems that required assistance from the treatment team. At this point, the team did not try to challenge the core of his delusional beliefs, thus avoiding any rifts in the collaborative process. However, as the therapy progressed, Mr. L and the therapist agreed to work on coping strategies such as using headphones to listen to music, watching TV or listening to the radio, engaging in dialogue with friends and family, and reading the newspaper.
The next step in therapy was helping Mr. L identify relationships between the emergence of psychotic symptoms and stressful life events. For instance, he noted that arguments with his father often led to an increase in his paranoid ideation as well as to his withdrawing from other people. He learned problem-solving and assertiveness skills and practiced them at home. He was instructed to experiment with a number of different strategies until he developed a useful coping repertoire.
In the next phase of treatment, the vulnerability-stress model of mental illness was presented. The model was used to help Mr. L understand his condition and to provide a rationale for why he should take antipsychotic medication. With this foundation, Mr. L was enrolled in an illness self-management course aimed at helping him develop strategies for recognizing the warning signs of relapse and learning techniques for avoiding relapses. Additional skills learned as part of this course were grooming and self-care, use of public transportation, and basic conversational techniques.
More advanced cognitive-behavioral therapy techniques were the focus of the next few sessions. For example, the therapist used Socratic questioning to engage Mr. L in talking about his psychotic ideas. The aim was to help him identify rational explanations for the occurrence of his psychotic experiences. This process entailed eliciting Mr. L's views of the reasons for the development and maintenance of his beliefs. In an atmosphere of trust, the collaborative therapeutic relationship that had been fostered over time allowed Mr. L to consider alternative interpretations of specific events, such as the possibility that his relatives were not really turning into monsters but were simply behaving in ways that he could not understand.
Next, the therapist targeted Mr. L's dysfunctional assumptions about himself, including his feelings of worthlessness and uselessness and his belief that he was unlovable. Through a process of guided discovery, Mr. L slowly realized the implications of his dysfunctional assumptions and was gradually able to develop a more realistic and salutary viewpoint.
By the end of the study, Mr. L had developed an increased ability to manage his psychotic symptoms. His symptoms gradually decreased while his quality of life improved. After six months of therapy, he was able to use public transportation independently. Soon after he moved to a nearby city and got a license to teach body-building skills, which allowed him to work as a teacher in a fitness center. His newly found social contacts there helped him to develop friendships with men and women. He also developed much better grooming skills and the ability to keep his apartment clean.
Afterword by the column editors: Although replication and generalization studies are needed, the benefits accrued from integrating clozapine with cognitive-behavioral therapy plus social skills training for the client with treatment-refractory schizophrenia are intriguing because of the difficulty in engaging these clients in therapy. The improved cognitive functioning and symptom stabilization that result from clozapine could enhance the effectiveness of cognitive-behavioral therapy and social skills training in ameliorating the irrational beliefs that distort clients' view of the world and impede social competence. These latter goals are notable prerequisites both for mobilizing clients to form stronger collaborations with their treatment team and for helping them achieve successful adaptation in their community.
It is perhaps expected that the symptom improvement over time due to clozapine was much greater than the effects of the cognitive-behavioral therapy plus social skills training. Treatments in schizophrenia tend to be domain specific, with medications having a greater impact on symptoms than psychosocial treatments, and psychosocial treatments having a greater effect on psychosocial functioning. We eagerly await a follow-up report from Dr. Pinto and his colleagues about the changes in psychosocial functioning brought about by cognitive-behavioral therapy plus social skills training. Even though psychosocial interventions are used with some of the most disabled and highly symptomatic patients with schizophrenia, the interventions have shown benefits beyond those that could be accounted for by medication (15,16).
The authors are affiliated with the treatment research unit of the Department of Mental Health of the Province of Naples in Pollena, Italy. Address correspondence to Dr. Pinto at Piazza Ettore Vitale 28, 80126 Naples, Italy. Alex Kopelowicz, M.D., and Robert Paul Liberman, M.D., are editors of this column.
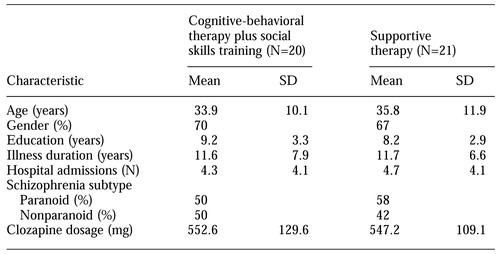 |
Table 1.
Demographic and clinical characteristics of clients with treatment-refractory schizophrenia started on clozapine who were randomly assigned to receive individual cognitive-behavioral therapy plus social skills training or individual supportive therapy
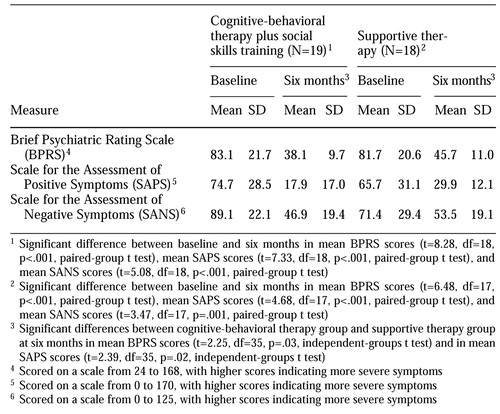 |
Table 2.
Baseline and six-month follow-up measures of symptoms for clients randomly assigned to receive individual cognitive-behavioral therapy plus social skills training or individual supportive therapy
1. Kopelowicz A, Liberman RP: The biobehavioral treatment and rehabilitation of schizophrenia. Harvard Review of Psychiatry 3:55-64, 1995Crossref, Medline, Google Scholar
2. Moebius RE, Jones BB, Liberman RP: Improving pharmacotherapy in a state hospital. Psychiatric Services 50:335-338, 1999Link, Google Scholar
3. Wykes T, Tarrier N, Lewis S: Outcome and Innovation in Psychological Treatment of Schizophrenia. Chichester, England, Wiley, 1998Google Scholar
4. Birchwood M, Tarrier N: Psychological Management of Schizophrenia. Chichester, England, Wiley, 1994Google Scholar
5. Green MF, Marshall B, Wirshing W, et al: Does risperidone improve verbal working memory in treatment-resistant schizophrenia? American Journal of Psychiatry 154:799-804, 1997Google Scholar
6. Green MF: What are the functional consequences of neurocognitive deficits in schizophrenia? American Journal of Psychiatry 153:321-330, 1996Google Scholar
7. Perris C: Cognitive Therapy With Schizophrenic Patients. New York, Guilford, 1989Google Scholar
8. Kingdon DG, Turkington D: Cognitive-Behavioral Therapy of Schizophrenia. New York, Guilford, 1994Google Scholar
9. Kuipers E, Garety P, Fowler D: London-East Anglia randomized, controlled trial of cognitive-behavioural therapy for psychosis: I. effects of the treatment phase. British Journal of Psychiatry 171:319-327, 1997Crossref, Medline, Google Scholar
10. Liberman RP, Mueser KT, Wallace CJ: Social skills training for schizophrenic individuals at risk for relapse. American Journal of Psychiatry 143:523-526, 1986Link, Google Scholar
11. Fowler D, Garety PA, Kuipers L: Cognitive Behaviour Therapy for Psychosis: Theory and Practice. Chichester, England, Wiley, 1995Google Scholar
12. Ventura J, Green M, Shaner A, et al: Training and quality assurance with the Brief Psychiatric Rating Scale: "the drift busters." International Journal of Methods in Psychiatric Research 3:221-224, 1993Google Scholar
13. Andreasen NC: The Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, University of Iowa, 1984Google Scholar
14. Andreasen NC: The Scale for the Assessment of Negative Symptoms (SANS). Iowa City, University of Iowa, 1983Google Scholar
15. Liberman RP, Van Putten T, Marshall BD Jr, et al: Optimal drug and behavior therapy for treatment-refractory schizophrenic patients. American Journal of Psychiatry 151:756-759, 1994Link, Google Scholar
16. Paul GL, Lentz RJ: Psychosocial Treatment of Chronic Mental Patients: Milieu Versus Social-Learning Programs. Cambridge, Mass, Harvard University Press, 1977Google Scholar