A Tentative Model of Aggression on Inpatient Psychiatric Wards
Abstract
Violence in psychiatric hospitals threatens the safety and well-being of patients and staff members. The determinants and correlates of inpatient aggression are not well understood. The authors present an explanatory model of aggressive behavior that attempts to integrate patient, staff, and ward variables. In the proposed model, the patient's psychopathology and distorted cognitions are exacerbated by environmental and communication stressors found on psychiatric wards. The model emphasizes that repeated inpatient aggression may be the result of a vicious circle, whereby a patient's violent behavior is often followed by an increase in stress on the patient caused by environmental or communication factors, heightening the risk of another outburst of violence.
Aggression by patients on psychiatric wards is a prevalent phenomenon. One study of a closed psychiatric ward with 20 beds found nearly one aggressive incident a day (1). Apart from physical and psychological consequences, violent behavior by patients has considerable financial implications (2).
Whittington and Wykes (3) noted that the vast majority of aggressive incidents in their study (86 percent) were preceded by some form of aversive stimulation of the patient by the staff. This finding suggests that environmental and interpersonal variables contribute to aggression, in addition to psychopathological and biological factors. Harris and Rice (4) have argued that attempts to reduce aggression "must be guided by what we know about the empirical relationships between situational variables and personal characteristics on the one hand and violence and antisocial behavior on the other."
This paper describes a tentative model that attempts to account for inpatient aggression in terms of psychopathology, such as distorted cognitions, as well as situational factors relevant to psychiatric wards.
The model
Patient, ward, and staff variables
Figure 1 presents the proposed model. On the left side are listed the three categories of variables that contribute to aggression— patient, ward, and staff variables. The model shows how these variables may interact to cause or exacerbate aggression.
Serious psychopathology is thought to be one of the major sources of inpatient aggression. Psychotic disorders, mania, personality disorders, substance abuse, and organic brain disease all have been found to be associated with impulsive behavior (5). The core variable in the model, psychopathology, leads to the patient's admission to a psychiatric ward. However, hospitalization inevitably introduces new situational stress on the patient.
After admission to the ward, several environmental stressors come into play. Patients may have to be locked up for safety reasons and generally will have little privacy on the ward. On a crowded psychiatric ward, patients can become overstimulated due to ward turmoil (6,7). Furthermore, patients may be exposed to therapies that may be too demanding. On the other hand, understimulation resulting from a lack of interesting activities may also lead to disruptive behavior.
Several staff variables are also stressors. Problematic communication between staff members and patients may contribute to aggression (3). Patients may become frustrated and angry if they perceive that staff members are not accessible or if they encounter obstacles to obtaining information (3). Inconsistencies in limit setting may also fuel aggression.
At the center of Figure 1 is the patient variable of cognitive stress. Patients' appraisal of the situation on the ward plays a key role in whether they will become aggressive. When patients are experiencing psychopathological symptoms, environmental and communication stressors may enhance their distorted cognitive interpretations of ward activities. For example, some patients may think "they're going to lock me up for ever" or "they're slowly poisoning me with pills." As a result of such thinking, patients may interpret environmental and communication stressors as being extremely threatening. Tension and anxiety will build up and panic or aggressive behavior may eventually occur.
Vicious circle
After a first outburst of aggression, a vicious circle is likely to develop. In response to the patient's violent behavior, environmental stressors may have to be increased to guarantee the safety of all parties. The patient may have to be secluded or may not be allowed to leave the ward. These measures are likely to reinforce the distorted beliefs that led to the patient's aggressive behavior and may make the patient more afraid of the ward team (8). Clearly, such an intensification of distorted cognitions will have a negative influence on the therapeutic alliance. Furthermore, aggressive behavior may result in negative countertransference reactions among staff members, creating additional problems in communication. Thus as a result of the inevitable increase in environmental and communication stressors, a repetitive pattern of violent behavior followed by the use of more restrictive measures may emerge.
Implications of the proposed model
The model suggests a number of interventions for which protocols can be set up and evaluated. Although no specific treatment for violence exists, several psychoactive drugs such as antipsychotics, lithium, antidepressants, sedatives, anxiolytics, anticonvulsants, and beta blockers have been successfully prescribed in the treatment of aggression secondary to psychopathology (8). For the large majority of psychotic patients, the administration of antipsychotics with or without sedatives will reduce hallucinations and delusions, thereby reducing violence (9).
Normalization of psychotic patients' cognitions will facilitate communication between staff and patients, reducing the need for further restrictive measures. Unfortunately, no unequivocal pharmacological strategy exists for preventing violence among patients with treatment-resistant schizophrenia, cluster B personality disorders, or impulse control disorders. In these cases, measures at the level of ward and staff variables should be carefully considered.
At the ward level, environmental stress may be reduced by creating units with enough privacy by providing patients with their own rooms, preventing overcrowding, and making sure that ward activities fit the needs and capacities of patients. At the staff level, communication stress may be diminished by providing patients with better information about treatment goals, investing more time in explaining why certain restrictions are necessary during treatment (10), and training staff to prevent and manage aggression. Increasing the number of skilled staff members to better meet the demands of patients may also reduce patient aggression.
Conclusions
The tentative model presented here encompasses psychopathological, cognitive, environmental, and communication variables to explain inpatient aggression. However, it is clear that these variables have different weights in different groups of patients. Krakowski and Czobor (6) demonstrated that environmental stress— specifically, ward turmoil— had a greater impact on transiently violent patients than on persistently violent patients. Persistent violence was found to be linked to poor frontal-lobe functioning.
Even in cases in which psychopathology is the primary antecedent of violent behavior, the contribution of environmental and communication stressors to aggression should not be ruled out. The model may help clinicians look beyond patient variables to consider situational variables involved in eliciting aggression.
Several assumptions underlying the proposed model need further testing. In particular, the influence of staff and ward variables on inpatient aggression is a neglected area of research. Evaluating the effects of interventions to prevent inpatient aggression may be hindered by the costs of the interventions, as well as the costs of evaluation research. However, large-scale attempts to prevent violent incidents may reduce the costs of treatment in the long run by producing a decline in sick leave among staff members (2) and enhancing their job satisfaction. Such programs may also result in shorter hospital stays, particularly for patients with schizophrenia.
Mr. Nijman is a senior researcher, Dr. à Campo is a psychiatrist, and Dr. Ravelli is a psychiatrist and member of the board of directors at the Psychiatric Hospital Welterhof in Heerlen, the Netherlands. Dr. Merckelbach is professor and Mr. Nijman is a senior researcher in the department of psychology at Maastricht University in Maastricht, the Netherlands. Address correspondence to Mr. Nijman at Psychiatrisch Centrum Welterhof, P.O. Box 4436, 6401 CX, Heerlen, the Netherlands (e-mail, [email protected]).
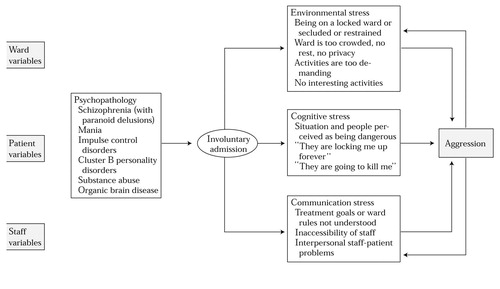
Figure 1. A tentative model of inpatient aggression
1. Nijman HLI, Allertz WWF, Merckelbach HLGJ, et al: Aggressive behaviour on an acute psychiatric admissions ward. European Journal of Psychiatry 11:106-114, 1997Google Scholar
2. Hunter M, Carmel H: The cost of staff injuries from inpatient violence. Hospital and Community Psychiatry 43:586-588, 1992Abstract, Google Scholar
3. Whittington R, Wykes T: Aversive stimulation by staff and violence by psychiatric patients. British Journal of Clinical Psychology 35:11-20, 1996Crossref, Medline, Google Scholar
4. Harris GT, Rice ME: Risk appraisal and management of violent behavior. Psychiatric Services 48:1168-1176, 1997Link, Google Scholar
5. Tardiff K: The current state of psychiatry in the treatment of violent patients. Archives of General Psychiatry 49:493-498, 1992Crossref, Medline, Google Scholar
6. Krakowski M, Czobor P: Violence in psychiatric patients: the role of psychosis, frontal lobe impairment, and ward turmoil. Comprehensive Psychiatry 38:230-236, 1997Crossref, Medline, Google Scholar
7. Palmstierna T, Huitfeldt B, Wistedt B: The relationship of crowding and aggressive behavior on a psychiatric intensive care unit. Hospital and Community Psychiatry 42:1237-1240, 1991Abstract, Google Scholar
8. Corrigan PW, Yudofsky SC, Silver JM: Pharmacological and behavioral treatments for aggressive psychiatric inpatients. Hospital and Community Psychiatry 44:125-133, 1993Abstract, Google Scholar
9. Tardiff K: Use of emergency medication, in Assessment and Management of Violent Patients, 2nd ed. Washington, DC, American Psychiatric Press, 1996Google Scholar
10. Nijman HLI, Merckelbach HLGJ, Allertz WWF et al: Prevention of aggressive incidents on a closed psychiatric ward. Psychiatric Services 48:694-698, 1997Link, Google Scholar



