Economic Grand Rounds: Rural Telepsychiatry Is Economically Unsupportable: The Concorde Crashes in a Cornfield
Telepsychiatry, the use of communication technologies to offer psychiatric services, has become a topic of great interest as a means of overcoming the effects of the shortage of psychiatrists in rural areas (1,2,3,4). The idea of using telecommunication in psychiatry is not new. In fact, examples can be found as far back as 1959, and the topic has been well reviewed (1,4,5,6).
Although the technology has improved to the point of providing adequate audiovisual interactions, the cost-effectiveness of these interactions remains unassessed. Clearly, technological feasibility does not eliminate the need for economic practicality. Before relying on telepsychiatry as a solution to inadequate psychiatric services in rural areas, we need to consider economic variables such as the cost of the equipment, charges for maintaining connections, the volume of use, and reimbursement. We also need to consider its impact on existing systems of care into which it would be introduced.
We studied the feasibility of implementing a telepsychiatry system to link psychiatrists at Michigan State University with patients at a community mental health center (CMHC) in rural Michigan. The target county we studied has a population of 58,000 and is approximately 75 miles from the university. The county is poor and demographically similar to many rural counties and is designated by the U.S. Department of Health and Human Services as an area with a shortage of mental health professionals. Many people lack transportation.
Based on our feasibility study, this column examines the economics of setting up a telepsychiatry system through which care can be provided to a rural area. Moreover, we estimated the cost of delivering one type of patient care (medication management) via this system. The purpose of the paper is not to provide a technological discussion of designing a system. Rather, we offer an analysis of economic issues and systems problems encountered in setting up a very basic telepsychiatry installation at the low end of the cost range.
Costs of telepsychiatry
Currently, at least 25 telepsychiatry projects report to the National Institute of Mental Health (7). The reports indicate a wide range in the frequency of use of this technology, and most reports state that some sort of evaluation will be conducted. Evaluations looking at diagnostic reliability and validity, users' perceptions of the encounters, and technical aspects such as the quality of the picture are already being reported (8,9,10,11) even as new uses are being proposed (12). As significant as these areas are to address, in our feasibility study it became obvious that an additional very important question must be asked: Would technology actually solve the problem at hand?
In the case of rural mental health, the problem that needs solving is how to provide affordable high-quality mental health care to patients in areas with few psychiatric resources. When looked at in this way, it becomes clear that quality of care is only half of the problem. The cost and practicality of providing telepsychiatric care also need scrutiny, regardless of the capacity of the technology.
Estimating costs for a telepsychiatry project is confounded by a large number of variables, such as equipment costs, volume of use, cost of clinic personnel attending the patient at the remote location, and installation, maintenance, and updating of equipment. There are also hidden costs—for example, the cost of training individuals, maintaining duplicate records, transmitting written copies of the treatment encounter, acquiring space for the telecommunications setup, and other infrastructure costs. All of these costs are in addition to the psychiatrist's time.
Many centers have spent between $75,000 and $100,000 per site in start-up costs (7). If one is willing to forgo studio-quality images, this figure can be reduced greatly by using desktop computer-based telecommunications equipment employing an integrated services digital network (ISDN) line. Practically speaking, with studio-quality images, one can observe halting movements associated with certain medications (cogwheel rigidity), whereas with a computer-based single ISDN line setup, all movement looks halting. We calculated costs using currently available desktop systems, a single ISDN line, and an ordinary office without special lighting.
Because every encounter involves two sites, costs estimates must be doubled for each session. Establishing several remote sites connecting to a center where a psychiatrist is located becomes very costly very quickly.
In the rural county we studied, the absence of digital lines created a major expense. Installation of digital lines in rural counties is not a high priority for telephone companies. The company we spoke with said that the projected use of such lines was too low for the company to recover its costs. However, the company offered to connect us if we paid for running a line from the nearest community that it did serve. For $6,000 a year, the company would put a single ISDN line in place in the community. There would be added time charges for its use. These costs are not likely to change any time soon.
In contrast, installing a line in a university office is only $150, and monthly charges are about $35. The charge for each 15-minute call is about $3.75 if placed from the university. Charges would be appreciably higher when the call is not initiated at the university. Therefore, the cost of a contact between a CMHC and a local hospital or clinic would be greater than the same contact between the university and a remote site.
The figures shown in Table 1 are based on low-cost, desktop-computer-based equipment. The costs are lower than those for systems described in the literature. Based on our interviews with rural mental health providers and patients, and our experience providing consultation to CMHCs in this rural area of Michigan, we think that the maximum number of telepsychiatry consults would be 260 per year. A telepsychiatry project covering the state of Montana, which has a population of 850,000, reported about 500 telepsychiatry consults per year using 12 sites (13). The Michigan county, with a population base of 58,000, can be expected to generate far fewer consults.
Currently, a psychiatrist is on site at the Michigan CMHC for one and a half to two days each week. Based on the number of patients served by this center, staffing guidelines issued by Michigan's Department of Community Health call for a full-time psychiatrist. A psychiatrist is needed on site to evaluate new patients, periodically reassess established patients, provide consultations to staff, and so forth. The need for such direct psychiatric services would not be reduced by installation of telepsychiatry. Telepsychiatry in rural areas provides otherwise unavailable services—it does not replace existing services. As shown below, the additional costs incurred when telepsychiatry is used make it worth considering only when other alternative forms of service provision are exhausted.
The cost of a telepsychiatry session was calculated in two ways depending on the location of the consulting psychiatrist (that is, the sites connected by the technology). Two formulas were used, and calculations are shown below—one for the per-session cost for a contact between the university and the rural CMHC and one for the per-session cost for a contact between the CMHC and another rural site, such as a medical unit of a hospital, to which the patient is brought. Given the estimated rate of 260 contacts a year for the system, for the calculations it was assumed that 130 contacts will take place between the university and the CMHC and the other 130 between the CMHC and another rural site. The CMHC will thus incur a cost for all 260 contacts, while the university and the other rural site will incur a cost for 130 contacts each.
The first calculation shows how the cost of a single telepsychiatry session between the university and the CMHC is calculated using the total costs per site per year shown in Table 1:
The per-session cost of $179 is derived by summing the per-session cost for each institution and adding a $4 time charge for using the ISDN line from MSU and a $15 charge for the time spent by the social worker who is present with the patient at the CMHC. For the university, the per-session cost is calculated by dividing the average annual cost of the telepsychiatry system to the university ($11,167, see Table 1) by 130 sessions. For the CMHC, the per-session cost is calculated by dividing the average annual cost of the telepsychiatry system to the CMHC ($19,167, see Table 1) by 260 sessions (the denominators are based on the arbitrary assumptions noted above).
The following calculation shows how the cost of a single telepsychiatry session between the CHMC and another rural site is derived.
The per-session cost of $244 is derived by summing the per-session cost for each site and adding an $8 time charge for using the ISDN line (the cost is higher for the nonuniversity line) and a $15 charge for the time spent by the social worker who is present with the patient. For the university, the per-session cost is calculated by dividing the average annual cost of the telepsychiatry system to the university ($11,167, see Table 1) by 130 sessions. For the CMHC, the per-session cost is calculated by dividing the average annual cost of the telepsychiatry system to the CMHC ($19,167) by 260 sessions. For the other rural site, the cost is calculated by dividing the system's average annual cost ($19,167) by 130 sessions.
The cost of a session of direct-service medication management at the CMHC is $78.50, based on $52.50 for the clinic costs plus $26 for the psychiatrist. For a telepsychiatry medication management session, which is a common application of telepsychiatry, the cost would depend on which two sites are linked by the technology. For a telepsychiatry contact between the university and the CMHC, $78.50 would be added to the lower per-session cost of $179, yielding $257.50. For a contact between the CMHC and another rural site, $78.50 would be added to the higher per-session cost of $244, yielding $322.50.
For purposes of illustration, we have based costs on the use of three sites—the university, the CMHC, and another rural site. If more sites were used, the total number of contacts might increase, but the cost per remote contact would increase dramatically because volume per site would inevitably fall. If technologically more sophisticated equipment and more digital lines were used to obtain a better image, costs could very easily reach $1,000 per telepsychiatry visit.
The figures presented above do not include the time and expense of transmitting records, making telephone calls to set up appointments, and so forth. Therefore, they are very conservative estimates of costs, which increase the certainty of our findings about the magnitude of additional costs incurred in using telepsychiatry.
We examined ways of bringing costs down. The most obvious step would be to dramatically increase the use of the equipment so the cost per use is lower. To do this, the equipment at both ends would have to be in general medical settings with a high volume of nonpsychiatric users. This scenario would be impossible in most rural counties, where no high-volume medical facilities exist. Furthermore, the CMHC in our study is not located on the site of a medical facility. Even if the conditions existed to share hardware, line charges, and other expenses, administrative problems would increase in the areas of scheduling and the equipment needs of the various participants, complicating a system whose intent is to ease the availability of consultation.
Problems of systems and boundaries
We found that setting up a rural telepsychiatry program among unrelated systems is very different from setting up a program within one all-encompassing system. In our project, as would be the case in many areas around the country, we were attempting to bring together a university, a private computer vendor, telephone companies, rural community mental health agencies, and rural private practitioners. As opposed to setting up a project within an integrated health network, the task of working with separate entities is horrendously time consuming and frustrating.
In our investigation of equipment, we found that no units can be simply plugged in and used. In many rural areas such as ours, it would take hundreds of hours to line up resources to establish a functioning site. At a local level a lack of control of critical components such as special transmission lines and unstable equipment suppliers would always exist, as would difficulties in maintaining a consistent level of technical support.
Once the technology is set up, additional systems enter the equation. In the needs assessment component of our feasibility study, the patients, mental health care workers, and primary care physicians whom we interviewed pointed out that factors such as privacy and security and legal and jurisdictional issues need to be considered. Another system to consider is insurers (6). In the two formulas for calculating per-session costs for telepsychiatry, would insurers be willing to pay for the psychiatrist on one end of the connection and a social worker on the other end? It should also be noted that the Health Care Financing Administration currently does not reimburse for telepsychiatry.
The CMHC in our rural area interacts with a number of systems of which it is not a part, including hospitals, other agencies, and groups of medical care providers. Adding to this mix psychiatrist consultants who lack a physical connection to the clinic or to the patient creates the need to deal with records, billing, and other matters that would increase the complexity of care. CMHCs in our state are facing immediate problems in terms of bringing costs down and increasing worker productivity. To establish an operating telepsychiatry consultation service, the commitment of human and financial resources would jeopardize a CMHC's capacity to meet its other demands. In this sense, telepsychiatry becomes unaffordable even if the equipment is paid for.
We have come to believe that the combination of eliminating boundaries between systems and finding the time and money to tackle problems is at least as big a hindrance to creating a working model as the more obvious technical and financial considerations. On one hand, the need for improved access to psychiatric services makes telepsychiatry attractive. On the other hand, so many problems exist in the organization of services and interacting systems that technologic solutions may be inappropriate. Although others have also alluded to these issues, (1,4,6) their importance appears to be underestimated in the enthusiasm for an enticing technology.
Where we are now?
The Concorde, a supersonic jet passenger plane, entered commercial service about 21 years ago. This graceful marvel of technology continues to fly passengers from New York to Paris in three and a half hours, about half the time of regular jet service. Today, a round-trip flight costs about $8,000, and no discounted fares exist. In comparison, a round trip using regular commercial jet service costs about $800.
The benefits of flying the Concorde are not worth the added costs, except in unusual circumstances in which money is no object. In addition, the Concorde serves only a very limited number of cities, so it remains irrelevant to the travel needs of an overwhelming number of air passengers.
Rural telepsychiatry may also be justified in unusual circumstances and when money is not a relevant consideration because of generous grants. Nearly 40 years have passed since the first remote psychiatric consultations were done using video technology. As with the Concorde, costs remain high, and the economic and practical feasibility of such services remains low for the typical rural county like the one we studied.
Deregulation of telephone services threatens to diminish or eliminate subsidies, and the price of rural service may rise. The rural economic base does not make it worthwhile for telephone companies to install expensive digital lines. Other types of technology using fiber optic lines, modified cable television, and so forth, are also very expensive. Considering the impoverished conditions in most of rural America, it would appear that the return on such investments would be questionable, limiting private investment. Government spending is declining, leaving no identifiable source of capital for nonprofit enterprises.
Pursuing new ideas is essential to solving health care delivery problems in psychiatry. However, in any exploration, it is important to differentiate between studying options and moving on to implementation. Obviously, we cannot study telepsychiatry without using it. Still, it is critical to keep in mind whether a system is being set up to study the technology or as a reliable solution to a problem. All of the programs we have identified in telepsychiatry have been funded through grants or are run at a loss. We have not found a program that would be sustainable through the delivery of services, nor do we think such a program is possible.
After considering economic and other variables involved in a simple case of telepsychiatry, we conclude that telepsychiatric services are technologically feasible, pragmatically difficult, and not economically supportable at this time.
Acknowledgments
This study was supported by an all-university outreach grant from Michigan State University. The authors thank James W. Dearing, Ph.D., Esther E. Onaga, Ph.D., Jody Ross, M.A., David Rovner, M.D., Kenzie Cameron, and Scott Preston for their help in this project.
Dr. Werner is professor of psychiatry in the department of psychiatry at Michigan State University, East Fee Hall, East Lansing, Michigan 48824-1316 (e-mail, [email protected]). Dr. Anderson is a resident in psychiatry at Oregon Health Sciences University in Portland. Steven S. Sharfstein, M.D., is editor of this column.
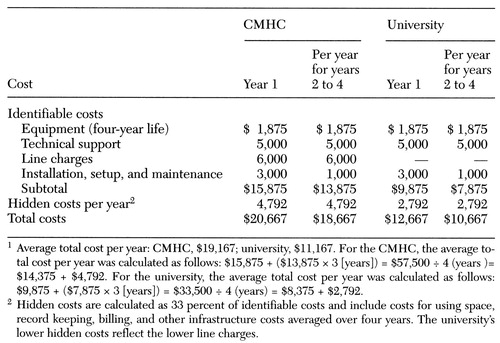 |
Table 1. Costs of establishing a telepsychiatry system to link psychiatrists at Michigan State University with patients at a community mental health center (CMHC) in rural Michigan, by site1
1. Preston J, Brown FW, Harley B: Using telemedicine to improve health care in distant areas. Hospital and Community Psychiatry 43:25-32, 1995 Google Scholar
2. Santos AB, Mallard DJ, Reicke CL: The high-tech solution to the rural service shortage. Hospital and Community Psychiatry 43:5, 1992 Abstract, Google Scholar
3. Graham MA: Telepsychiatry in Appalachia. American Behavioral Scientist 39:602-615, 1996 Crossref, Google Scholar
4. Field MJ (ed): Telemedicine: A Guide to Assessing Telecommunications in Health Care. Washington, DC, National Academy Press, 1996Google Scholar
5. Brown FW: Rural telepsychiatry. Psychiatric Services 49:963-964, 1998 Link, Google Scholar
6. Bennett J, Huang MP, Alessi N: Barriers to telemedicine in psychiatry, in Mental Health Computing. Edited by Miller MJ, Hammond KW, Hile MG. New York, Springer-Verlag, 1996Google Scholar
7. LaBella S, Magruder K, Pollitt A, et al: A Compendium of Telecommunications Projects With Mental Health Applications. Rockville, Md, National Institute of Mental Health, Office of Rural Mental Health Research, 1995Google Scholar
8. Dongier M, Tempier R, Lalinec-Michaud M, et al: Telepsychiatry: psychiatric consultation through two-way television: a controlled study. Canadian Journal of Psychiatry 31:32-34, 1986 Crossref, Medline, Google Scholar
9. Baer L, Cukor P, Jenike MA, et al: Pilot studies of telemedicine for patients with obsessive-compulsive disorder. American Journal of Psychiatry 152:1383-1385, 1995 Link, Google Scholar
10. Zarate CA Jr, Weinstock L, Cukor P, et al: Applicability of telemedicine for assessing patients with schizophrenia: acceptance and reliability. Journal of Clinical Psychiatry 58:22-25, 1997 Crossref, Medline, Google Scholar
11. McLauren PM, Laws VJ, Ferreira AC, et al: Telepsychiatry: outpatient psychiatry by videolink. Journal of Telemedicine and Telecare 2(suppl 1):59-62, 1996 Medline, Google Scholar
12. Jones BN, Colenda CC: Telemedicine and geriatric psychiatry. Psychiatric Services 48:783-785, 1997 Link, Google Scholar
13. Kostreski F: Telepsychiatry gains in popularity. Clinical Psychiatry News 25(4):1-2, 1997 Google Scholar



