Datapoints: Self-Reported Unmet Need for Mental Health Care After California's Parity Legislation
California's mental health parity law required private health insurance plans to offer mental health coverage as part of health benefit packages and eliminate mental health benefit limit and cost-sharing requirements that are less comprehensive than those for general medical conditions after July 2000 ( 1 ). This could have increased use of mental health care services and reduced unmet need among the privately insured, although it would not directly affect persons with public or no insurance. Self-insured health plans are also exempted from the parity legislation under the Employee Retirement Income Security Act ( 1 ). In addition, the 2004 Mental Health Services Act (Proposition 63) funded improvements to mental health services in the public sector ( 2 ).
We tracked changes in use of mental health care services and self-reported unmet need from 2001 to 2005 using the California Health Interview Survey, a repeated cross-sectional survey. A total of 56,270 and 43,020 adults aged 18 years or older were included in waves 2001 and 2005, respectively. Perceived need for mental health care was assessed with the question, "During the past 12 months, did you think you needed help for emotional or mental health problems, such as feeling sad, blue, anxious, or nervous?" Among those expressing need, use of mental health care services was assessed with the question, "Not counting overnight stays, emergency room visits, or visits for drug or alcohol problems, in the past 12 months, have you seen a psychiatrist, psychologist, social worker, or counselor for emotional or mental health problems?" We defined unmet need as expressing need but not having used services.
Figure 1 shows that use of mental health care services among the privately insured significantly decreased (p<.05), even though it increased among persons with public insurance (p<.05). No significant change in use was found among the uninsured.
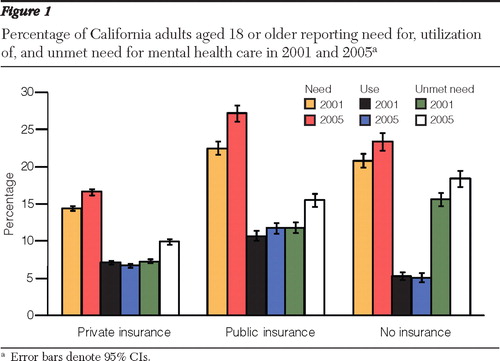
Perceived need for mental health care services increased significantly in all groups, however, resulting in a net increase of unmet need among the privately insured, among those with public insurance, and among the uninsured (p<.001 for all).
Parity legislation applied to the privately insured, but it did not result in increased use of mental health care services in this group. Maybe more important, parity legislation cannot address the substantial disparities in mental health care utilization by insurance status.
Acknowledgments and disclosures
Research support was provided by grant R21AA017265 from the National Institute on Alcohol Abuse and Alcoholism.
The authors report no competing interests.
1. Rosenbach ML, Lake TK, Williams SR, et al: Implementation of mental health parity: lessons from California. Psychiatric Services 60:1589–1594, 2009Google Scholar
2. Feldman S: The "millionaires tax" and mental health policy in California. Health Affairs 28:809–815, 2009Google Scholar



