Advisor-Teller Money Manager (ATM) Therapy for Substance Use Disorders
People with severe psychiatric illnesses commonly use alcohol, cocaine, or both ( 1 , 2 ). Because of their substance use and disabling psychiatric illnesses, patients with co-occurring disorders are frequently poor and need to make the most of their limited income to avoid abject poverty. Unfortunately, high proportions of psychiatric patients report difficulty managing their money and have made poor financial decisions under the influence of drugs ( 3 ). Patients' desire to have money is a potentially powerful motivation to stop buying alcohol and cocaine, and people who are poor and mentally ill indicate a desire for help with concrete financial concerns ( 4 ).
Advisor-teller money manager therapy (ATM) is a money management-based intervention that targets substance use. ATM attempts to break the linkage between a patient's money and cued associations with drug use by storing the patient's funds and training him or her to budget funds for things other than substances of abuse ( 5 ). Patients in the ATM program work with their therapists to make budgets, thus mentally associating their money with planned nondrug expenditures that in turn are linked to long-term goals. Behavioral economists have described how such "mental accounting" shapes spending decisions ( 6 ), how small changes in framing goals and account management can "nudge" people toward prosocial goals ( 7 ), and how budgeting can alter subsequent spending ( 8 ).
A version of ATM in which checkbooks, not patient funds, were stored was tested in a randomized clinical trial among 85 veterans with recent substance use. This low-intensity ATM was acceptable to participants, in that three-quarters of veterans assigned to ATM at some point voluntarily turned a checkbook or banking card over to the study therapist to store ( 9 ). However, high abstinence rates in the control group limited the power to determine efficacy. Other financial counseling approaches to substance abuse treatment have been studied but usually as part of bundled interventions, such as assertive community treatment ( 10 ).
Another bundled money management-based intervention is the assignment of a representative payee to manage Supplemental Security Income (SSI) or Social Security Disability Income (SSDI) payments for patients who are judged incapable of managing their own funds. Substance use is frequently the reason for payee assignment ( 11 , 12 ). Studies suggest that properly implemented payee programs can reduce substance use ( 13 , 14 ), but retrospective cohort studies in which payeeship practice was not specified have had more modest or no benefits ( 12 , 15 ).
Therefore, studies of case management and representative payee assignment suggest they may ameliorate substance use, but in these interventions, the type of money management is not specifically structured to prevent drug use. The aim of this study was to compare the efficacy of ATM with a control condition in reducing substance use among patients receiving psychiatric treatment for serious mental illness at a public community mental health center.
Methods
Participants
Participants were recruited at a community mental health center by advertisement, referral from other study participants, and encouragement from clinicians to contact study staff. Participants were asked to provide written informed consent only if they were able to accurately answer a four-question quiz concerning the study procedures. The study was approved by the Yale Institutional Review Board.
We enrolled participants with histories of a DSM-IV-defined substance use disorder involving cocaine, alcohol, or both within the past five years; Global Assessment of Functioning (GAF) scores <65; and monthly income ≤$450. Patients were excluded if they were working with a representative payee or conservator or if there was a plan to do so. The first 31 participants had to come to the randomization visit with either funds or a checkbook—a requirement that was later dropped to broaden enrollment.
Study design
This was a single-site randomized, single-blind, controlled clinical trial. Enrollment began in July 2004 and ended in March 2008. After recruitment and confirmation of study eligibility, patients completed assessments and were then scheduled for another appointment for random assignment. Patients were assigned to treatment condition with an urn randomization procedure ( 16 ), which adjusted for sex, race, and cocaine or alcohol use (use of both substances was defined as cocaine use).
Interventions
Both interventions were delivered by the same bachelor's-level research staff (crossed design) at a community mental health center. Patients were encouraged to attend scheduled sessions of both therapies weekly, but therapists allowed drop-in visits and interruptions in therapy attendance. Patients received ATM at the mental health center in addition to treatment as usual, which was typically weekly group psychotherapy and psychotropic medication targeting psychiatric symptoms.
Patients in the ATM condition were encouraged but not required to store their funds in an account accessible by only the study therapist. At weekly meetings, patients reviewed adherence to the budgets they had made, reviewed completion of planned activities from the previous week, obtained funds from their account that had been prebudgeted, and submitted breath for alcohol analysis and urine for on-site toxicology testing for cocaine. Patients who had used drugs or alcohol reviewed the circumstances surrounding the relapse, and their treating clinicians (not connected with the study) were informed. A description of ATM is available on request, and updated materials are posted at www.behaviorchange.yale.edu .
A minimal control intervention was provided in which patients were given a workbook containing budgeting forms. Therapists helped patients complete the forms by identifying patients' income and expenses. At follow-up appointments, therapists supported patients' efforts to adhere to budgets and refrain from substance use.
Assessments and measurements
At intake, patients underwent an extensive battery of tests, which included the Structured Clinical Interview for DSM-IV Axis I Disorders ( 17 ) and the Addiction Severity Index (ASI), version 5 ( 18 ). To determine substance use, every other week for 36 weeks we had patients submit on-site urine toxicology tests for cocaine metabolites, cannabis, and opioids (Syva, Dade Behring), and we interviewed them and used a timeline follow-back method to record their reports of substance use on calendars ( 19 ). Every four weeks, patients were administered abbreviated versions of the alcohol and drug composite subsections of the ASI, and their nonstudy clinicians were asked to estimate patients' alcohol use and drug use on a 5-point scale anchored by 1, abstinent, and 5, dependent ( 20 ).
At the baseline random assignment and every four weeks for 36 weeks thereafter, patients were given GAF scores based on a brief assessment, and they completed the Brief Symptom Inventory (BSI) ( 21 ). Attendance at nonstudy treatment at the mental health center was tracked by a questionnaire. Therapy processes, a 25-item Likert rating subscale, was administered (available on request) to measure participants' experience of components of the therapies. Exploratory factor analysis of this questionnaire yielded factors representing perceived benefit from the study therapy, satisfaction with therapy, and spending. Finances were tracked by a questionnaire with inquiries about sources of income and expenses during the preceding 30 days. All longitudinal assessments were completed again at week 52. Patients were paid with gift cards for local stores after assessment sessions and could earn a total of $380 if all assessments were completed.
Data analysis
All 90 patients who completed at least one outcome assessment were considered in this intent-to-treat analysis. Initially, proportional hazards regression analyses were conducted to determine whether study retention evaluated by completion of assessments differed between groups. Baseline differences between patients assigned to the two treatments were evaluated with t tests for continuous measures and chi square tests for categorical variables. The primary outcome measures were urine toxicology results for cocaine use and weeks of self-reported alcohol use as indicated on the substance use calendar. Monthly cash balance was not normally distributed, so its natural log was analyzed, and dichotomous values (substance use versus nonuse) were analyzed for clinician ratings of drug and alcohol use and for expenditures on drugs.
Outcome measures were then entered into hierarchical linear models with time in weeks as a level 1 variable and time modeled on level 2 as a function of group assignment. With few exceptions, the baseline value of each dependent variable was included as a covariate to account for preexisting differences. In addition, in all models we assessed as covariates demographic variables on which groups differed at baseline. Only statistically significant demographic covariates were retained in the respective models. Normal or Bernoulli distributions were specified, depending on the outcome. Analyses were conducted with HLM 6.0 software ( 22 ) and full maximum likelihood estimation. For toxicology-measured abstinence from cocaine, moderator analyses were conducted by including potential treatment moderator variables in the level 2 time-slope model along with group assignment and the product of group assignment and the relevant variable. All statistical tests were two tailed, with trends (p<.10) and significance (p<.05) reported. We calculated effect size as the standardized mean difference in slopes ( 23 ). Finally, we used ordinary least-squares regression to assess the contribution of treatment utilization variables (number of appointments attended and storage of funds) to the prediction of treatment outcome (slope of cocaine abstinence).
Results
Recruitment and patient flow
Many more patients were screened (N=376) than were randomly assigned and followed (N=90). [A CONSORT diagram showing patient flow is available as an online supplement to this article at ps.psychiatryonline.org .] As has been typical of studies in this population ( 24 ), substance-using patients who were screened and accepted into the study often did not participate in the follow-up screening (N=135).
Participant follow-up with assessments after random assignment was excellent. The average percentage of scheduled assessment appointments kept was 79% (746 of 940) for participants assigned to ATM and 73% (624 of 860) for those assigned to the control condition. There was no significant difference between groups in the proportion of participants lost to follow-up. The week 36 assessment was attended by 77% (36 of 47) of ATM participants and 79% (34 of 43) of control group participants, and the last assessment (week 52) was attended by 83% (39 of 47) of ATM participants and 72% (31 of 43) of control group participants.
Patient characteristics
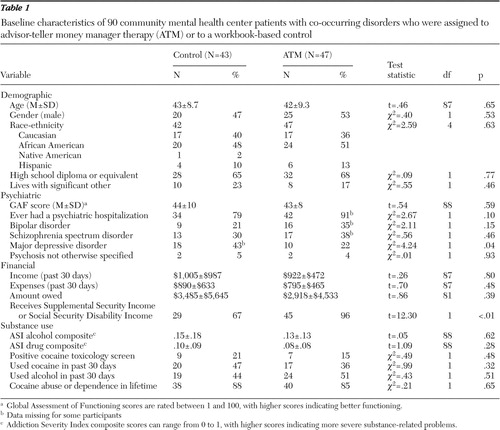
The demographic characteristics of the patients served by this urban community mental health center are shown in Table 1 . A high proportion (74 of 90, 82%) received SSI or SSDI, and 80 of 89 (90%) had one of the major axis I psychiatric disorders listed. Random assignment resulted in two significant treatment group differences ( Table 1 ). Patients assigned to ATM were significantly more likely to be recipients of SSI or SSDI and less likely to have a diagnosis of major depression.
 |
Treatment participation
As expected, ATM patients attended many more face-to-face appointments than did patients in the control group (mean±SD 22.5±15.48 sessions for the ATM group versus 3.0±2.22 sessions for the control group; t=-8.5, df=48, p<.001). ATM patients' participation in money management was extensive, too. Altogether, 37 of 46 (80%) patients assigned to ATM involved their money manager in storing their funds—15 of 46 (33%) deposited funds to the group account, 16 of 46 (35%) had the ATM therapist store the patient's checkbook, and six of 46 (13%) did both. (Data were missing for one patient.)
Payee assignment
Payee assignment was not a planned part of ATM, but a question concerning whether a payee or conservator had been assigned was added at weeks 36 and at 52. Ten of the 47 patients assigned to ATM were assigned a payee or conservator during the 12 months after randomization and only two patients in the control group were ( χ2 =5.6, df=1, p=.02). Five of these ATM patients were assigned payees toward the end of the study and had had good relationships with the ATM therapist, two were assigned money managers after clinical worsening, and three met with money managers after receiving greater attention to their finances by their clinicians (N=2) or by the Social Security Administration (N=1).
Substance abuse outcomes
Patients assigned to ATM had significantly more toxicology-determined abstinence from cocaine over time than control group participants ( Table 2 ). Consistent with the improved toxicology-measured abstinence, ATM participants were more likely to be abstinent from drugs, as rated by their nonstudy clinicians. These findings were robust (effect size of .74 for toxicology difference and effect size of .86 for clinician ratings). Groups also differed significantly on self-reported money spent on substances; ATM participants were significantly less likely to report purchasing substances over time than were control group participants (p=.04, df=88). The effect of ATM on cocaine abstinence was not moderated by any of the measures tested, indicating an equal treatment effect for subgroups based on age, gender, race and ethnicity, and psychiatric diagnosis.
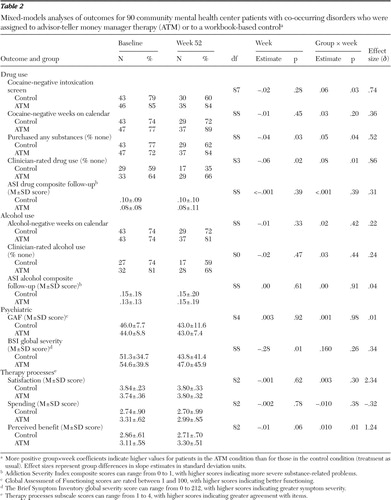 |
As shown by the group means over time, the between-groups differences in drug use emerged toward the end of the assessment period and were greatest at week 52. [A figure showing the group means over time is available as an online supplement to this article at ps.psychiatryonline.org .] The group means also showed that more participants had positive toxicologies for cocaine than self-reported use of it. With analyses controlling for treatment assignment, attendance at appointments did not predict cocaine use, and among ATM-assigned participants, depositing funds was also not a significant predictor of abstinence from cocaine.
The alcohol self-report measures—ASI composite alcohol scores and calendar-recorded ratings of alcohol use—did not differ between groups, nor did scores for clinician-rated alcohol use.
Psychiatric outcomes
There were no differences in GAF score or BSI total severity scores between groups over time ( Table 2 ). BSI subscale analyses showed trends toward more paranoia (p=.05) and more psychosis over time (p=.06) among patients assigned to ATM. There was no difference between groups in the proportion of patients attending nonstudy treatment, indicating that ATM neither facilitated treatment at the mental health center nor substituted for it.
Therapy-related adverse events
One patient in ATM assaulted the money manager. The patient had stopped taking his prescribed antipsychotic medication, became homeless, came to an ATM session asking for his SSDI check, and then assaulted the money manager when she informed him that the check had not arrived. Another patient became agitated when his clinicians initiated conservatorship hearings.
Therapy processes and budgeting
As shown in Table 2 , patients assigned to ATM rated themselves significantly higher on items reflecting perceived benefit from ATM but not significantly higher on measures reflecting altered spending or satisfaction. Mean satisfaction in the control group was 3.8 or above (on a scale of 1 to 4) throughout, leaving little room for improvement.
Discussion
ATM significantly reduced drug use by two important measures—urine toxicology tests and clinician ratings. Self-reported measures were less robust, albeit in the same direction. The effects were not explained by differential adherence to follow-up assessments; high proportions of participants in both ATM and control groups were followed, and if missing urinanalyses were scored as positive ( 24 ), there would have been an even larger difference favoring ATM. The significant reduction in cocaine use in the ATM condition is noteworthy because there is limited empirical support for any specific substance abuse treatment for indigent people with concomitant substance use and severe and persistent mental disorders ( 25 ). Some of the treatments that have shown promise are quite extensive—residential treatment ( 26 ), case management ( 27 ), a multicomponent biweekly approach ( 24 ), and incentivized participation in a Veterans Health Administration work program ( 28 ).
The finding that cocaine toxicology and clinician ratings were sensitive to ATM's effects but self-reported cocaine use was less sensitive may be partially explained by the lower rates of self-reported cocaine use than positive toxicologies ( 29 ), creating less room to detect improvement with ATM. Furthermore, the ASI self-report measure has not been a consistently valid indicator of drug use severity in this population ( 30 ). The lack of an ATM effect on alcohol consumption may reflect the fact that heavy alcohol use is less expensive than heavy cocaine use and may be less responsive to money management intervention.
Even in a voluntary intervention in which clients could discontinue participation at any time, money management was emotionally charged, as indicated by the assault on the money manager and trends toward higher ratings of psychosis and paranoia. Conflict between representative payees and clients has been described previously ( 31 , 32 ). It has been suggested that the main reason for conflict between clients and representative payees is because of coercion by the payees ( 33 ). However, our findings suggest that a financial approach and stewardship are emotionally charged, even among ATM participants who were not in mandated, coerced treatment.
In this study, additional therapist training in crisis de-escalation was provided after the adverse events occurred, so that therapists would be better prepared for the possibility that ATM patients would demand their money. Patients were seen in open areas with other staff present when there was concern about potential violence. There were no other study-related adverse events with the subsequent patients. These precautions are necessary to safely conduct ATM.
The finding that patients in ATM were disproportionately assigned representative payees was unexpected. Other work has shown that patients in a treatment setting that emphasizes payeeship were more likely to be assigned representative payees ( 12 , 34 ), and the emphasis on money management in ATM may have had the same effect. Our clinical impression was that payee assignment more often reflected a positive experience in ATM and desire to continue to receive money management after the study, rather than a mandate imposed on beneficiaries by third parties, but both desire for a payee and coercion were factors to varying degrees for different patients.
Limitations of the study are the relatively small sample and the study of a heterogeneous population. Another limitation is that is that in this study, ATM, a multicomponent intervention, was compared with a weak control intervention. Therefore, the specific mechanism by which ATM participants reduced their cocaine use is not certain. Benefit from ATM was not associated with attendance at greater numbers of sessions or by storage of funds with the ATM therapist. Patients assigned to ATM who participated in it extensively to receive financial counseling likely diluted the relationship between session attendance and reduced cocaine use. It has been noted that patients with psychiatric illnesses frequently desire help with financial matters but may be ambivalent about substance abuse treatment ( 3 , 35 ). The sample was too small and payee assignment was too sporadically implemented to determine its impact on outcomes, but a descriptive review of patients who were assigned payees during the study showed no consistent change in patterns of cocaine use after the payee was assigned.
There are several implications of the study findings for treatment of persons with co-occurring disorders. One is that ATM warrants further study as a treatment for people with severe psychiatric illnesses who use cocaine. More generally, the findings suggest the promise of money management approaches to treatment of people with substance use disorders. Money management is often a component of case management, residential treatment ( 36 ), and assertive community treatment ( 10 ), albeit in less formalized formats. The outcomes reported here suggest that financial components of other interventions may contribute to their effectiveness. Finally, although this was not a study of representative payee assignment, its findings suggest the potential efficacy of payee arrangements when the representative payee also implements other components of ATM—setting goals, training patients to budget, and on-site substance abuse counseling.
Conclusions
ATM is an efficacious therapy for the treatment of cocaine abuse and dependence among people with concomitant psychiatric illness and was associated with more frequent assignment of a representative payee. However, patients may become angry at ATM therapists.
Acknowledgments and disclosures
This work was funded by grants R01-DA12952, K02 DA017277, P50 DA09241 from the National Institute on Drug Abuse and by the Veterans Integrated Service Network 1, Mental Illness Research, Education, and Clinical Center. The clinical trial is registered at www.clinicaltrials.gov (Abstinence-Linked Money Management, NCT00536900).
The authors report no competing interests.
1. Dixon L: Dual diagnosis of substance abuse in schizophrenia: prevalence and impact on outcomes. Schizophrenia Research 35(suppl):S93–S100, 1999Google Scholar
2. Kessler RC, Crum RM, Warner LA, et al: Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry 54:313–321, 1997Google Scholar
3. Rosen MI, Rosenheck RA, Shaner A, et al: Veterans who may need a payee to prevent misuse of funds for drugs. Psychiatric Services 53:995–1000, 2002Google Scholar
4. Evans JD, Wright DE, Svanum S, et al: Psychiatric disorder and unmet service needs among welfare clients in a representative payee program. Community Mental Health Journal 40:539–548, 2004Google Scholar
5. Shaner A, Eckman TA, Roberts LJ, et al: Disability income, cocaine use, and repeated hospitalization among schizophrenic cocaine abusers: a government-sponsored revolving door. New England Journal of Medicine 333:777–783, 1995Google Scholar
6. Thaler RH: Mental accounting matters. Journal of Behavioral Decision Making 12:183–206, 1999Google Scholar
7. Thaler RH, Sunstein CR: Nudge: Improving Decisions About Health, Wealth and Happiness. New Haven, Yale University Press, 2008Google Scholar
8. Thaler RH, Shefrin HM: An economic theory of self-control. Journal of Political Economy 39:392–406, 1981Google Scholar
9. Rosen MI, Carroll KM, Stefanovics E, et al: A randomized controlled trial of a money management-based substance use intervention. Psychiatric Services 60:498–504, 2009Google Scholar
10. Lehman AF, Dixon LB, Kernan E, et al: A randomized trial of assertive community treatment for homeless persons with severe mental illness. Archives of General Psychiatry 54:1038–1043, 1997Google Scholar
11. Conrad KJ, Matters MD, Hanrahan P, et al: Characteristics of persons with mental illness in a representative payee program. Psychiatric Services 49:1223–1225, 1998Google Scholar
12. Rosen MI, McMahon TJ, Rosenheck R: Does assigning a representative payee reduce substance abuse? Drug and Alcohol Dependence 86:115–122, 2007Google Scholar
13. Ries RK, Comtois KA: Managing disability benefits as part of treatment for persons with severe mental illness and comorbid drug/alcohol disorders: a comparative study of payee and non-payee participants. American Journal on Addictions 6:330–338, 1997Google Scholar
14. Conrad KJ, Lutz G, Matters MD: Randomized trial of psychiatric care with representative payeeship for persons with serious mental illness. Psychiatric Services 57:197–204, 2006Google Scholar
15. Swartz JA, Hsieh CM, Baumohl J: Disability payments, drug use and representative payees: an analysis of the relationships. Addiction 98:965–975, 2003Google Scholar
16. Stout RL, Wirtz PW, Carbonari JP, et al: Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol Supplement 12:70–75, 1994Google Scholar
17. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for the DSM-IV Axis I Disorders—Patient Edition (SCID-I/P Version 2.0). New York, New York State Psychiatric Institute, Biometrics Research Department, 1996Google Scholar
18. McLellan AT, Kushner H, Metzger D, et al: The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment 9:199–213, 1992Google Scholar
19. Sacks JA, Drake RE, Williams VF, et al: Utility of the time-line follow-back to assess substance use among homeless adults. Journal of Nervous and Mental Disease 191:145–153, 2003Google Scholar
20. Rosenberg SD, Drake RE, Wolford GL, et al: Dartmouth Assessment of Lifestyle Instrument (DALI): a substance use disorder screen for people with severe mental illness. American Journal of Psychiatry 155:232–238, 1998Google Scholar
21. Derogatis LR: Brief Symptom Inventory (BSI): Administration, Scoring, and Procedures Manual, 2nd ed. Baltimore, Clinical Psychometric Research, 1992Google Scholar
22. Raudenbush SW, Bryk AS, Cheong YF, et al: HLM 6: Hierarchical Linear and Nonlinear Modeling. Lincolnwood, Ill, SSI, 2004Google Scholar
23. Raudenbush SW, Xiao-Feng L: Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychological Methods 4:387–401, 2001Google Scholar
24. Bellack AS, Bennett ME, Gearon JS, et al: A randomized clinical trial of a new behavioral treatment for drug abuse in people with severe and persistent mental illness. Archives of General Psychiatry 63:426–432, 2006Google Scholar
25. Drake RE, O'Neal EL, Wallach MA, et al: A systematic review of psychosocial research on psychosocial interventions for people with co-occurring severe mental and substance use disorders. Journal of Substance Abuse Treatment 34:123–138, 2008Google Scholar
26. Brunette MF, Mueser KT, Drake RE, et al: A review of research on residential programs for people with severe mental illness and co-occurring substance use disorders. Drug and Alcohol Review 23:471–481, 2004Google Scholar
27. Essock SM, Mueser KT, Drake RE, et al: Comparison of ACT and standard case management for delivering integrated treatment for co-occurring disorders. Psychiatric Services 57:185–196, 2006Google Scholar
28. Drebing CE, Van Ormer EA, Krebs C, et al: The impact of enhanced incentives on vocational rehabilitation outcomes for dually diagnosed veterans. Journal of Applied Behavior Analysis 38:359–372, 2005Google Scholar
29. Shaner A, Khalsa ME, Roberts L, et al: Unrecognized cocaine use among schizophrenic patients. American Journal of Psychiatry 150:758–762, 1993Google Scholar
30. Bennett ME, Bellack AS, Gearon JS, et al: Development of a comprehensive measure to assess clinical issues in dual diagnosis patients: the Substance Use Event Survey for Severe Mental Illness. Addictive Behaviors 31:2249–2267, 2006Google Scholar
31. Elbogen EB, Swanson JW, Swartz MS, et al: Family representative payeeship and violence risk in severe mental illness. Law and Human Behavior 29:563–574, 2005Google Scholar
32. Estroff SE, Swanson JW, Lachicotte WS, et al: Risk reconsidered: targets of violence in the social networks of people with serious psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology 33(suppl 1):S95–S101, 1998Google Scholar
33. Angell B, Martinez NI, Mahoney CA, et al: Payeeship, financial leverage, and the client-provider relationship. Psychiatric Services 58:365–372, 2007Google Scholar
34. Hanrahan P, Luchins DJ, Savage C, et al: Representative payee programs for persons with mental illness in Illinois. Psychiatric Services 53:190–194, 2002Google Scholar
35. Ziedonis DM, Smelson D, Rosenthal RN, et al: Improving the care of individuals with schizophrenia and substance use disorders: consensus recommendations. Journal of Psychiatric Practice 11:315–339, 2005Google Scholar
36. Tsemberis S, Gulcur L, Nakae M: Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. American Journal of Public Health 94:651–656, 2004Google Scholar



