An Examination of Premature Mortality Among Decedents With Serious Mental Illness and Those in the General Population
It is well established that persons with mental illness experience excess mortality compared with the general population ( 1 , 2 , 3 , 4 , 5 ). Studies that examine life expectancy or premature mortality have shown that persons with mental illness die much sooner than those without mental illness ( 5 , 6 , 7 ). The National Association of State Mental Health Program Directors' (NASMHPD's) report titled Morbidity and Mortality in People With Serious Mental Illness ( 7 ) reviewed the results of a number of state-level studies on premature mortality. Using data from inpatient and outpatient settings from 1997 to 2000, these studies reported that persons with serious mental illness die on average between 13.5 and 32.2 years earlier than the general population. The NASMHPD report also states, "People with serious mental illness die, on average, 25 years earlier than the general population. State studies document recent increases in death rates over those previously reported." The report also states that "60% of premature deaths in persons with schizophrenia are due to medical conditions such as cardiovascular, pulmonary and infectious diseases." Because the risk for these causes of death is associated with a number of modifiable risk factors, such as tobacco use and obesity, these deaths can be viewed as preventable ( 8 , 9 ).
Premature mortality among adults with serious and persistent mental illness has important implications for the treatment system. These include the role that the fragmented health care system plays in reducing access to primary care for persons with serious and persistent mental disorders, the relative lack of attention that both the mental health and general medical health care systems have paid to wellness and prevention activities, and the contribution of treatment itself (for example, second-generation antipsychotic medications) to premature mortality. However, to really understand premature mortality among persons with serious and persistent mental illness, we need to better understand differences in premature mortality between those with and without mental illness, as well as the factors that may explain those differences.
With the exception of one study ( 6 ), research on years of potential life lost (YPLL) among persons with serious mental illness is limited in that it typically does not take into account YPLL in the general population. By not examining differences in premature mortality, the results of these studies may have overestimated premature mortality in the population with serious mental illness. We seek to address this limitation through a comparison of YPLL in a sample of decedents with serious and persistent mental illness with a sample of decedents in the general population.
Current research on premature mortality has also focused on inpatient populations or outpatient settings that include individuals with a wide range of diagnoses. Inpatient samples may overestimate premature mortality because those patients tend to be sicker, whereas differences in mental health diagnoses among outpatient samples may account for differences in premature mortality. All of the decedents with serious and persistent mental illness in this study were, at the time of death, receiving treatment in a community mental health center serving only clients with serious and persistent mental illness.
We also took into account differences in social factors and cause of death that may account for differences in premature mortality. There are a number of studies that examine the relationship between social factors and mortality in the general population. They show that gender, race, education, and marital status are all associated with mortality ( 10 , 11 , 12 , 13 ). Additionally, social factors explain some of the difference between those with mental illness and the general population in terms of the rates at which people die. For example, one study ( 14 ) found that standardized mortality ratios were significantly reduced when the analyses adjusted for socioeconomic factors. However, studies using YPLL as a measure of premature mortality tend not to account for variation in social factors.
The purpose of this study was to broaden the understanding of the relationship between serious mental illness and premature mortality. We compared decedents with serious and persistent mental illness who were treated in a community-based setting with decedents in the general population for the same period and in the same community to examine whether there were significant differences in YPLL, whether social factors and cause of death explained any of the difference in YPLL, and whether there were particular causes of death that differentially affected YPLL among persons with serious and persistent mental illness.
Methods
Study setting
The data for this study came from death records and clinical records. First, death records were obtained from the Ohio Department of Health for 1998 through 2004. Death records were then linked to clinical case management files from Community Support Services (CSS), a community mental health center in Akron, Ohio. CSS serves the majority of adults in the county who have serious and persistent mental disorders and is funded by the county behavioral health authority. These disorders include psychotic disorders (schizophrenia and schizoaffective disorder), mood disorders (dysthymic, major depressive, and bipolar disorders), and other disorders (anxiety and personality disorders). Consumers with a primary diagnosis of substance use disorder or dementia were excluded from analysis, because these diagnoses were deemed by the research team to fall outside the definition of serious and persistent mental illness. During the study period CSS served about 3,000 individuals annually, with an active caseload between 2,000 and 2,500. The CSS population was predominantly white or African American, with approximately 33.7% African Americans and 65.8% whites during the study period (the study sample was limited to African Americans and whites). The record link identified CSS consumers who died during the seven-year period and allowed us to determine axis I diagnoses for these consumers. A comparison group, composed of persons who were not CSS consumers and who died during this same period, was created by querying all of the deaths among adults 18 and older with addresses in Akron. Because the majority of CSS clients live in Akron (78.2%), city-level data (as opposed to state or county data) were used for the comparison group to provide a better sociodemographic match to the CSS population. This resulted in a total sample size of 16,164: 647 CSS cases and 15,517 non-CSS cases.
Personal identifiers in clinical records were accessed for matching purposes only and were removed from the data file before analyses were conducted. The study was deemed exempt by the institutional review board at the Northeastern Ohio Universities Colleges of Medicine and Pharmacy.
Cause of death
Cause of death was determined using the underlying cause of death as documented by ICD-9 or ICD-10 codes on the death record. A variable was created for each cause of death and assigned a value of 1 if present and a value of 0 if not present.
YPLL
YPLL is a widely used measure of premature mortality that is based on the mean survival age for a living cohort at each age ( 4 , 6 ) and was determined for each case on the basis of U.S. life expectancy in the year of death (data from the Centers for Disease Control and Prevention [CDC], 1998–2004) ( www.cdc.gov/nchs/fastats/lifexpec.htm ). For all years of the study combined, the mean YPLL was calculated for all causes of death.
Social factors
Information on gender, race, marital status, and level of education, all of which were obtained from the death record, were included in all multivariate models.
Age adjustment
Because the CSS and non-CSS cases had different age distributions, a weight was created to adjust for this difference following direct standardization procedures recommended by the CDC ( 15 ) and utilized in previous research ( 2 , 6 ). The formula used to compute the final weight was W=PGP/PCSS, where W is the final analysis weight for each CSS case by age, PGP is the proportion of Akron cases for each age, and PCSS is the proportion of CSS cases for each age. The final analysis weight was applied to the data and used in all subsequent analyses. After weighting, the CSS sample size was 649 and the non-CSS sample was 22,828.
Analysis
Chi square analyses and t tests were conducted to determine whether there were significant differences between CSS decedents and non-CSS decedents in YPLL, social factors, and causes of death. Analysis of covariance was used to estimate average YPLL with adjustment for social factors. Multivariate ordinary least-squares (OLS) regression models were estimated to determine whether differences in cause of death accounted for differences in YPLL. Interaction terms were then added to these models to test whether particular causes of death had a greater effect on YPLL for CSS decedents than for the community comparison group. SPSS, version 15.0, was used for all analyses.
Results
Table 1 presents descriptive information for the study sample, as well as the results of t tests for differences in means and proportions for all study variables. Mean age of decedents in the sample was 79.4±11.1 years. Fifty-six percent were female, and 20% were African American. The unadjusted mean YPLL for CSS decedents was 14.5±10.6, compared with 10.3± 6.7 for the non-CSS group. On average, CSS decedents died at the age of 73.4±15.4, compared with 79.6±10.9 years for the non-CSS population. There were also significant differences in three of the sociodemographic variables used in this study. Although level of education was similar in both groups, there was a larger percentage of women and a smaller percentage of African Americans in the CSS group. Persons with serious and persistent mental illness were less likely to be married at the time of death. Most of the decedents with mental illness had a diagnosis of some psychotic disorder (47%), 36% had a mood disorder, and the remaining 17% had some other diagnosis.
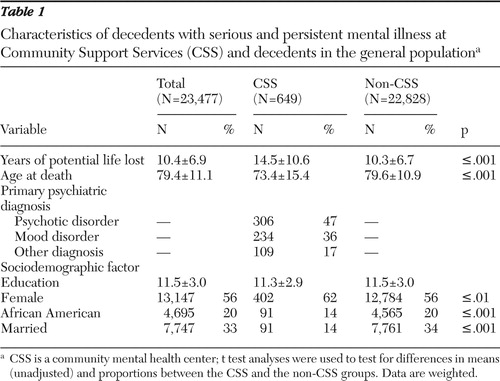 |
Table 2 presents leading causes of death for the U.S. population ( 16 ) and the two study groups. Heart disease was the top cause of death in all three groups. In contrast, although cancer was the second leading cause of death in the U.S and non-CSS populations, cancer was only the fifth leading cause of death in the CSS sample.
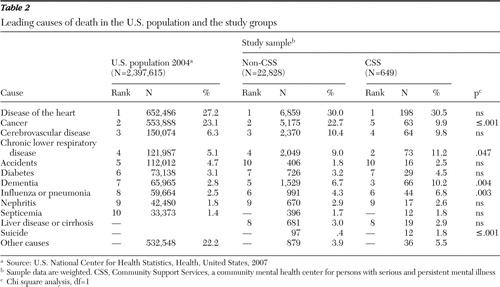 |
The leading causes of death in all three groups include heart disease, cancer, cerebrovascular disease, chronic lower respiratory disease, diabetes, dementia, influenza or pneumonia, and nephritis. In addition, the CSS and non-CSS samples included liver disease in the ten leading causes of death. Septicemia was in the ten leading causes of death for the U.S. population, but it was not a leading cause for either the CSS or non-CSS samples. Compared with non-CSS decedents, decedents with serious and persistent mental illness were more likely to die from chronic lower respiratory disease (11.2% versus 9.0%; χ2 =4.0, df=1, p=.047), dementia (10.2% versus 6.7%; χ2 =8.3, df=1, p=.004), and influenza or pneumonia (6.8% versus 4.3%; χ2 =8.9, df=1, p=.003), but they were much less likely to die from cancer (9.9% versus 22.7%; χ2 =61.2, df=1, p≤.001). Although suicide did not appear in the top ten causes of death for either study group, our results suggest that persons with mental illness were more likely to have deaths attributed to suicide (1.8% versus .4%; χ2 =22.3, df=1, p≤.001).
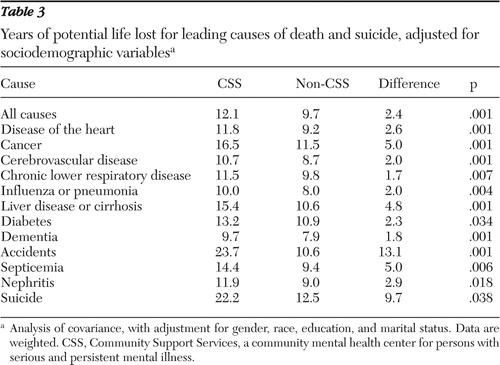
Table 3 shows that there were significant differences in YPLL between the CSS and non-CSS groups for the leading causes of death, after the analysis adjusted for gender, race, marital status, and education. For all causes combined, the CSS decedents died 12 years earlier than expected and lost over two more years of life, compared with persons in the general population. There were significant differences in YPLL for all causes after taking into account gender, race, education, and marital status. Causes of death for which the greatest difference in YPLL was found include accidents (13.1 years), suicide (9.7 years), cancers (5.0 years), septicemia (5.0 years), and liver disease (4.8 years).
 |
Next, multivariate OLS regression models were estimated to assess whether cause of death accounted for observed differences in YPLL. In addition, we added interaction terms to determine whether there were causes of death that had a differential effect on persons with serious and persistent mental illness. Results are presented in Table 4 .
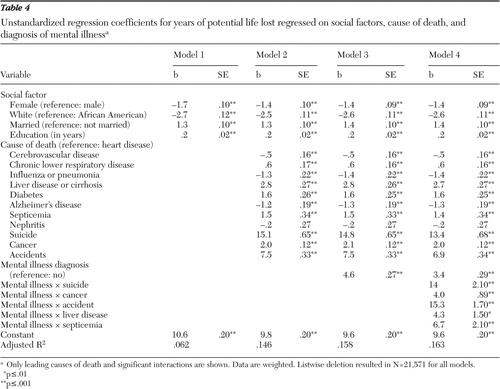 |
Model 1 shows the effect of social factor variables. All of the social factors were related to YPLL and accounted for 6% of the variance in YPLL. Women and whites lost fewer years of life, compared with men and African Americans. In addition, decedents in the study who were married or had more education lost more years of life, compared with those who were not married and those with less education. Each cause of death was added in model 2. For these analyses, heart disease was used as the reference category because it was the highest ranked cause of death for both groups. Nephritis was the only cause of death for which premature mortality was not significantly different from heart disease. Model 3 assessed the effect of having a mental illness, after adjusting for gender, race, marriage, education, and causes of death. A diagnosis of mental illness significantly increased the YPLL, regardless of cause of death.
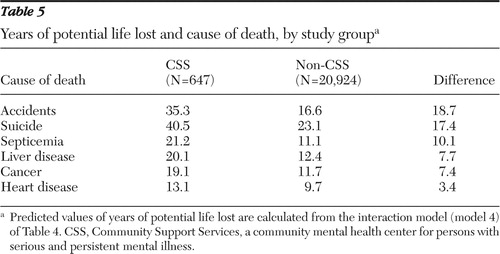
As a final step, we entered interactions terms (together and separately) for each cause of death and having a mental illness diagnosis to determine whether there were particular causes of death that had a differential effect on YPLL for persons with serious and persistent mental illness. The significant interactions are presented in model 4 of Table 4 . We used the coefficients in this model to predict YPLL for each of the significant interactions. These values are presented in Table 5 . These findings suggest that accidents, suicide, septicemia, liver disease, and cancer have a greater impact on premature mortality for persons with serious and persistent mental illness.
 |
Discussion
The purpose of this study was to broaden the current understanding of premature mortality among persons with serious mental illness. Consistent with previous studies ( 4 , 6 , 7 ) we found that for each of the leading causes of death, persons with serious and persistent mental illness lost more years of life, compared with those in the general population of Akron. Previous studies have also suggested that persons with serious mental illness are more likely to die from unnatural causes, such as suicide, accidents, and assault ( 4 , 6 ). This was true in the study presented here as well. However, most deaths among persons with mental illness in this sample were attributed to natural causes. The same causes of death appeared in the top ten for both CSS decedents and the general population. In addition, there were only four causes for which we found significant differences between the two study groups in the proportion of people dying: cancer, chronic lower respiratory disease, dementia, and pneumonia.
Much previous work has been based on samples of consumers who have been hospitalized or on mixed inpatient and outpatient samples ( 5 ). The study presented here adds to previous work in this area by examining premature mortality in a sample of consumers with serious and persistent mental disorders who received treatment primarily in a community-based treatment setting. The majority of individuals with serious and persistent mental illness live in the community; thus the sample in this study is more representative than state hospital samples. The results presented above suggest that although consumers in community settings experience a significant degree of premature mortality, they may experience it to a lesser degree than consumers who were recently hospitalized before their death.
We found that a community-based sample of adults with severe and persistent mental illness lost 14.5 years of potential life, a difference of 4.2 years from the Akron sample. This gap is smaller than that reported by Dembling and colleagues ( 6 ), who reported an 8.8-year difference in YPLL. This difference may represent overall higher mortality in an urban sample, compared with that of a statewide population, especially because Akron is a city with a poverty rate nearly twice the national average and an unemployment rate near 10% ( 17 ).
This study also makes a contribution by taking into account differences in social factors. Although we were limited to measures contained in the death record, our consideration of the role these factors play in premature mortality makes an important contribution to the literature. Our findings suggest that although gender, race, marital status, and education are importantly related to YPLL, premature mortality among persons with serious and persistent mental illness cannot be explained by sociodemographic differences.
We also asked whether differences in cause of death accounted for any of the differences in premature mortality and whether the relationship between cause of death and YPLL is moderated by a diagnosis of mental illness. We found that differences in premature mortality are not explained by differences in cause of death. Moreover, our results show that when premature mortality for heart disease was used as the reference group, premature mortality related to suicide, cancer, accidents, liver disease, and septicemia was greater for persons with serious and persistent mental illness than for persons in the general population.
Our finding that suicide and accidents are a source of premature mortality among persons with mental illness is consistent with previous research ( 4 , 6 , 18 , 19 , 20 ). However, our work adds to the growing body of literature that highlights the need for better preventive health care for persons with mental illness. Morbidity and mortality from the most common causes of death in this sample (heart disease, respiratory diseases, cerebrovascular disease, and cancer) may be reduced by effective medical care that attempts prevention, early detection, and chronic disease management.
As noted above, one important limit of our study is that we were restricted to the measures contained in the death records. For example, we did not have access to better measures of socioeconomic status. Therefore, the results we report may be related to differences in income between the CSS and non-CSS groups.
Conclusions
We found that a community-based sample of individuals with serious and persistent mental illness died prematurely, compared with a demographically similar general population sample. Social factors were related to premature mortality, but they did not account for the differences in YPLL that we observed. Although total YPLL and the difference in YPLL between the individuals with mental illness and the general population were smaller than those from hospital-based samples, deaths were largely from preventable causes. Heart disease was the top cause of death.
Recent efforts to improve access and quality of primary care health services by integrating such services within the community mental health center appear to be a promising approach to addressing these preventable causes of death. The concept of the mental health care home ( 21 ) holds great promise. Integrating mental health care, primary health care, and wellness-promoting activities in a single center may ensure access to the interventions needed to reverse the causes of preventable early death.
Acknowledgments and disclosures
The authors acknowledge the technical assistance provided by Jon Garey, M.S.C.I.S., Voula Androulakakis, M.S., Bayard Paschall, Ph.D., and Tom Grande, M.A.
The authors report no competing interests.
1. Felker B, Yazel J, Short D: Mortality and medical comorbidity among psychiatric patients: a review. Psychiatric Services 47:1356–1363, 1996Google Scholar
2. Cohen ME, Dembling B, Schorling JB: The association between schizophrenia and cancer: a population-based mortality study. Schizophrenia Research 57:239–246, 2002Google Scholar
3. Enger C, Weatherby L, Reynolds RF, et al: Serious cardiovascular events and mortality among patients with schizophrenia. Journal of Nervous and Mental Disease 192:19–27, 2004Google Scholar
4. Miller BJ, Paschall CB, Svendsen DP: Mortality and medical comorbidity among patients with serious mental illness. Psychiatric Services 57:1482–1487, 2006Google Scholar
5. Roshanaei-Moghaddam B, Katon W: Premature mortality from general medical illness among persons with bipolar disorder: a review. Psychiatric Services 60:147–156, 2009Google Scholar
6. Dembling BP, Chen DT, Vachon L: Life expectancy and causes of death in a population treated for serious mental illness. Psychiatric Services 50:1036–1042, 1999Google Scholar
7. Parks J, Svendsen D, Singer P, et al (eds): Morbidity and Mortality in People With Serious Mental Illness. Alexandria, Va, National Association of State Mental Health Program Directors, Medical Directors Council, 2006Google Scholar
8. Mokdad AH, Marks JS, Stroup DF, et al: Actual causes of death in the United States, 2000. JAMA 291:1238–1245, 2004Google Scholar
9. Goodarz D, Ding EL, Mozaffarian D, et al: The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Medicine 6:e1000058, 2009Google Scholar
10. Lidfeldt JT, Li Y, Hu FB et al: A prospective study of childhood and adult socioeconomic status and incidence of type 2 diabetes in women. American Journal of Epidemiology 165:882–889, 2007Google Scholar
11. Eaker ED, Sullivan LM, Kelly-Hayes M, et al: Marital status, marital strain, and risk of coronary heart disease or total mortality: the Framingham Offspring Study. Psychosomatic Medicine 69:509–513, 2007Google Scholar
12. Rask K, O'Malley E, Druss B: Impact of socioeconomic, behavioral, and clinical risk factors on mortality. Journal of Public Health 31:231–238, 2009Google Scholar
13. Dupre ME, Beck AN, Meadows SO: Marital trajectories and mortality among US adults. American Journal of Epidemiology 170:546–555, 2009Google Scholar
14. Segal SP, Kotler PL: A ten-year perspective of mortality risk among mentally ill patients in sheltered care. Hospital and Community Psychiatry 42:708–713, 1991Google Scholar
15. Curtin LR, Klein RJ: Direct Standardization (Age-Adjusted Death Rates), Healthy People 2000 Statistical Notes. DHHS pub no (PHS) 95-1237. Hyattsville, Md, National Center for Health Statistics, March 1995Google Scholar
16. Heron MP: Deaths: leading causes for 2004. National Vital Statistics Reports 56:5, 2007Google Scholar
17. American Fact Finder, American Community Survey 2005–2007. Washington, DC, US Census Bureau. Available at factfinder.census.gov Google Scholar
18. Berren MR, Hill KR, Merikle E, et al: Serious mental illness and mortality rates. Hospital and Community Psychiatry 45:604–605, 1994Google Scholar
19. Wan JJ, Morabito DJ, Khaw L, et al: Mental illness as an independent risk factor for unintentional injury and injury recidivism. Journal of Trauma, Injury, Infection, and Critical Care 61:1299–1304, 2006Google Scholar
20. Dickey B, Dembling B, Azeni H, et al: Externally caused deaths for adults with substance use and mental disorders. Journal of Behavioral Health Services and Research 31:75–85, 2004Google Scholar
21. Smith TE, Sederer LI: A new kind of homelessness for individuals with serious mental illness? The need for a "mental health home." Psychiatric Services 60:528–533, 2009Google Scholar



