Medication Preferences and Adherence Among Individuals With Severe Mental Illness and Psychiatric Advance Directives
Poor medication adherence remains a significant problem for many persons with severe mental illness ( 1 , 2 , 3 , 4 , 5 ). Medication preferences logically should affect medication adherence; patients who choose to take certain medications in accord with their personal preferences should be more likely to adhere to those medications over time. For patients, an informed decision to take a particular medication can be a highly personal choice that involves balancing perceived benefits with potential drawbacks and risks ( 6 , 7 , 8 ). To make this choice, patients must be offered opportunities to clearly communicate their preferences, and prescribers must acknowledge and respect patients' stated choices. Psychiatric advance directives provide patients with mental illness a formal way to document their treatment preferences, including medication preferences ( 9 , 10 ). It is unknown whether psychiatric advance directives can help align prescribed medications with patient preferences and thus improve medication adherence. This study examined whether patients who use psychiatric advance directives to request particular medications are actually prescribed their preferred medications and, when they are, whether concordance between preferred and prescribed medications improves medication adherence.
Barriers to medication adherence among persons with severe mental illness have been studied extensively, and they include poor efficacy of available medications for some patients ( 11 , 12 ), intolerable medication side effects ( 13 , 14 , 15 ), delusional thinking ( 16 , 17 ), lack of insight into illness ( 3 , 18 , 19 , 20 ), co-occurring substance abuse ( 1 , 17 , 18 , 21 ), lack of social support ( 22 , 23 ), and poor therapeutic alliance ( 16 , 19 , 21 , 24 ). Among individuals with physical illnesses, numerous studies also have shown that when patients perceive input into decision making about their own treatment, they are significantly more likely to adhere to that treatment ( 25 , 26 , 27 , 28 ). However, expressed patient preference for medication among persons with mental illness has been less well studied.
Psychiatric advance directives are legal documents that allow individuals with severe mental illness to document preferences for future treatment if they lose decisional capacity during a psychiatric crisis ( 9 , 29 ). Although psychiatric advance directives were designed for crisis situations, they can also be used as person-centered plans to coordinate ongoing treatment ( 30 , 31 ). Facilitated psychiatric advance directives, in which a clinician or other support person assists the patient in completing an advanced directive, provide a forum for patients to express their preferences about psychiatric medications in a nonconfrontational manner ( 28 ). Because most psychiatric medications are not uniquely indicated for acute care, it is likely that the medications individuals request on psychiatric advance directives are those that have worked well for them not only in crisis situations but also in long-term use.
Content analyses of psychiatric advance directives have reported the frequency of medication requests and refusals in these documents ( 32 , 33 , 34 ). However, no previous studies have compared medications requested in psychiatric advance directives to those actually prescribed or examined whether receiving preferred medications improves medication adherence. The goals of this study were to describe the medication preferences of individuals with severe mental illness who completed psychiatric advance directives, determine the extent to which participants' prescribed medications were aligned with their medication preferences, and examine whether the degree of alignment between prescribed and preferred medications predicted medication adherence at 12-month follow-up.
Methods
This study is part of a larger randomized controlled trial of the effectiveness of a facilitation intervention for psychiatric advance directives conducted in two county-based mental health programs in north-central North Carolina ( 32 ). The intervention, adapted from several medical and psychiatric advance directive planning tools ( 35 , 36 , 37 ), was an approximately two-hour, semistructured, manualized interview and guided discussion of choices for planning mental health care during future periods of incapacity. It incorporated all required elements of psychiatric advance directives in North Carolina statutes, including advance instructions for preferred facilities, treatments, crisis interventions, and emergency contacts, as well as the option to designate a health care power of attorney. The facilitator also assisted participants in completing legal psychiatric advance directive documents, obtaining witnesses, getting documents notarized, and filing forms in the medical record and electronic registry. In this article we address only the medication portion of the facilitated advance directives; previous articles have reported on other aspects of patient preference ( 32 , 33 , 38 ).
To be eligible for the study, participants had to be 18 to 65 years old and have a chart diagnosis of schizophrenia, schizoaffective disorder, bipolar disorder with psychotic features, or major depressive disorder with psychotic features. All participants were outpatients receiving community-based treatment in one of two county-based programs. Eighty-three percent of participants (N=390) were randomly drawn from deidentified client lists of the two mental health programs and were prescreened for eligibility. In order to increase the study's generalizability to patient populations with severe mental illness at high risk of relapse and with decisional incapacity, the remaining 17% of participants (N=79) were identified from sequential admissions from the mental health programs to the regional state hospital. These individuals were contacted, screened, and randomly assigned after discharge to the facilitation group or the control group.
A total of 636 individuals were screened for inclusion; of these, 469 enrolled and provided written informed consent after receiving a complete description of the study. A total of 239 were randomly assigned to the facilitation group; 230 were randomly assigned to the control group, which was provided with general information about psychiatric advance directives, copies of standard psychiatric advance directive forms, and a toll-free number for the local consumer organization that provides consultation on psychiatric advance directives. All participants completed a structured baseline interview to obtain personal demographic, clinical, and attitudinal information. Of the 239 individuals randomly assigned to the treatment group, 174 participated in a facilitation session and 146 completed a legal psychiatric advance directive. Of these 146 individuals, 123 completed a 12-month follow-up interview. Interviews were conducted between October 2004 and September 2006. The study presented here is restricted to the 123 participants who completed the intervention and the 12-month follow-up interview. The Duke University Medical Center Institutional Review Board approved this study.
Measures
At baseline and the 12-month follow up, participants completed a structured interview to obtain personal demographic, clinical, and attitudinal information. They identified all medications they were currently taking and estimated their level of adherence to their medication regimen on a 6-point scale. Possible scores ranged from 1 (never took medication) to 6 (never missed taking medicine), with higher scores indicating better adherence. For data analysis, we dichotomized the responses as "never missed taking medicine" versus all other responses, because our sample had a high overall adherence rate; 65 (53%) reported that they had never missed taking any medication. Previous studies have documented that individuals tend to overestimate their adherence to medications ( 39 , 40 ), which may partly explain this finding. Using the strictest criteria for adherence may help counteract self-report bias.
We reviewed participants' psychiatric advance directives and recorded patient medication preferences. During the psychiatric advance directive facilitation, participants were assisted in completing their psychiatric advance directives through open-ended prompts to identify medications they would request for treatment if they were in a crisis. Likewise, they were prompted to identify medications they would not be willing to take. All medications that patients explicitly consented to or refused in their psychiatric advance directives were listed as "requested medications" or "refused medications," respectively.
Analysis
Descriptive statistics and correlations were calculated for relevant variables. We used Wilcoxon matched-pairs testing to compare change in medications from baseline to 12 months. We also compared participants' medication preferences with their report of medications they were prescribed at baseline and at 12 months. Because of the small sample, we used forward-selected stepwise logistic regression to identify factors associated with medication adherence at 12 months. Our possible predictor variables included age, sex, race, diagnosis, Brief Psychiatric Rating Scale (BPRS) score ( 41 ), positive score on either drug or alcohol abuse screens (CAGE screens) ( 42 , 43 ), history of hospitalization in the past 12 months, baseline medication adherence, and concordance between participants' medication preferences and their prescribed medication at baseline and at 12 months. We used SAS, version 9.1, for all data analysis.
Results
Of the 123 study participants, 73 (59%) were female. Sixty-five (53%) were African American, and the remainder were Caucasian. Mean±SD age was 44.5±9.9 years. Seventy-seven (63%) had either schizoaffective disorder or schizophrenia, 31 (25%) had bipolar disorder, and 15 (12%) had major depressive disorder with psychotic features. Although 37 (30%) individuals reported using drugs or alcohol in the past 30 days, only eight (7%) had a chart diagnosis of a substance use disorder. Nineteen (15%) scored positive on the CAGE questionnaire (a widely used method of screening for alcoholism) ( 42 ), and ten (8%) scored positive on a version of the CAGE adapted for drug abuse screening ( 43 ). The average BPRS ( 41 ) score was 33.3±8.9, which is consistent with mild impairment ( 44 ). (Possible scores on the BPRS range from 18 to 126, with higher scores indicating more severe pathology.) Twenty-eight individuals (23%) had experienced a psychiatric hospitalization in the past 12 months. Seventy (57%) were living independently, 21 (17%) were married or cohabiting, and 31 (25%) were currently employed. When we compared the participating individuals to the 23 individuals who completed psychiatric advance directives but did not complete the 12-month follow-up interview, we found no significant differences in demographic characteristics or clinical data.
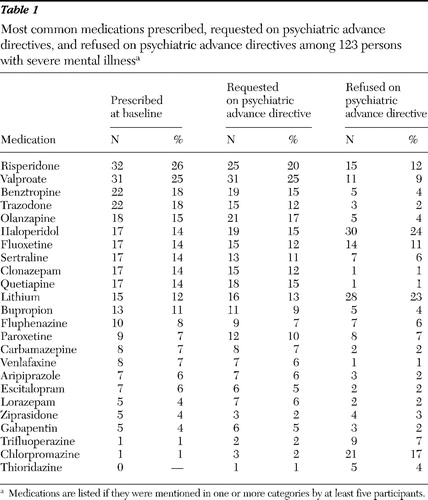
Most individuals reported taking several medications; they reported taking a mean of 2.4±1.2 medications at baseline and at 12 months (median, two; range, one to six). Individuals requested a mean of 2.4±1.4 medications in their psychiatric advance directives (median, two; range, zero to six) and refused a mean of 1.5±1.6 medications (median, one; range, zero to ten). The most common medications that were prescribed, requested, and refused are reported in Table 1 .
 |
Concordance between individual participants' requested medications and prescribed medications increased between baseline and the 12-month follow-up. Between baseline and follow-up there was a 27% increase in the number of prescribed medications that had been requested on the psychiatric advance directive (Wilcoxon matched pairs, p<.001). For the 113 persons for whom data were available, only seven (6%) had a decrease between baseline and the follow-up in the number of requested medications they were receiving, whereas 77 (68%) had no change and 29 (26%) had an increase ( Figure 1 ). Because listing more medications on the psychiatric advance directive would increase the probability of having a positive change (for example, if a participant requested ten medications, by chance alone there would be a greater possibility of adding a requested medication than if she or he listed only one), we corrected for the number of medications listed in the psychiatric advance directive by dividing the number of requested medications prescribed by the total number of medications requested. Mean corrected concordance was .73 at baseline and .82 at the 12-month follow-up, a 10% increase that remained significant (Wilcoxon matched pairs, p<.001).

Our final reduced regression model of self-reported adherence at 12 months (R 2 =.33) showed that receiving at least one requested medication at the 12-month follow-up predicted greater adherence at 12 months (odds ratio [OR]=7.8, 95% confidence interval [CI]=1.8–34.0, p<.01). This remained significant after the analysis controlled for adherence to medications at baseline (OR=8.2, CI=3.4–19.9, p<.001). No other variables were retained in the final model.
Discussion
Examining psychiatric advance directives for medication instructions provides a unique way to identify medication preferences among individuals with severe mental illness. Individuals who requested particular medications on their psychiatric advance directives were more likely to report being prescribed those medications at the 12-month follow-up, and individuals who were taking at least one requested medication at the 12-month follow up were more likely to report adherence to their medications. These findings are consistent with literature on adherence to medical treatment showing that patient preferences are associated with better adherence ( 14 , 26 , 28 ). Given the correlation between preferences expressed in the psychiatric advance directive and the individual's medication regimen one year later, psychiatric advance directives may offer an important new tool for providers to incorporate shared decision making with patients and elicit patient preferences.
It is important to note that although there was an increase in average concordance between medication preferences as expressed in participants' psychiatric advance directives and the medications they received one year later, 77 individuals reported no change in the number of preferred medications they were taking over the study period. Completing a psychiatric advance directive is clearly not a guarantee that a patient will receive preferred medications. However, even among individuals who had no increase in the number of preferred medications over the study period, adherence was greater after 12 months as long as they reported taking at least one preferred medication. That is, individuals were more likely to adhere to medication regimens that included at least one preferred medication, regardless of whether they were switched to that medication or maintained one that they were already taking at baseline.
We can only speculate about the actual processes through which documenting medication preferences in a psychiatric advance directive could result in changes to patients' prescribed medications. Although we did not assess whether participants discussed their psychiatric advance directives with their outpatient providers, it is possible that they used their psychiatric advance directives as a tool for direct communication with their clinicians, leading to a change in medication based on their explicitly expressed preferences. It is also possible that the act of completing a psychiatric advance directive, which requires thinking about preferences, may have indirectly affected participants' interactions with their clinicians. The process of completing a psychiatric advance directive can help patients recognize and articulate their preferences for the first time. In subsequent interactions with clinicians, patients who have completed psychiatric advance directives may feel empowered and may become more assertive and articulate in stating their preferences. Regardless of mechanism, our findings suggest that psychiatric advance directives could have benefits beyond those of their original crisis-related purpose.
Results for specific medications that participants requested and refused on the directives are interesting, but given the small sample, it is difficult to make detailed inferences from this information. Our results do suggest that preferences for medication are highly individualistic, as suggested by the occurrence of haloperidol and risperidone as among the most commonly preferred and the most commonly refused medications in our sample. It is also worth noting that the average number of refused medications was 1.5, whereas the average number of requested medications was 2.4. Some clinicians fear that psychiatric advance directives will enable patients with poor insight to refuse all treatment, even treatment that might be beneficial ( 38 , 45 ). However, in this study, individuals on average provided prior consent to more medications than they refused. For these individuals, psychiatric advance directives should help clinicians provide patient-centered care rather than hinder them.
The size of our sample limits the precision of our results, particularly in our statistical model of adherence; results should be considered preliminary. Another limitation of the sample is that it may not be representative of the population of persons with severe mental illness as a whole. Although our participants were drawn from a randomized study, we examined only those who completed the study. These participants were willing to spend several hours completing a psychiatric advance directive and to be recontacted after a year; thus it is possible that this group was more motivated and more interested in self-determined care than the overall group from the randomized trial or from this population in general. Our results may be most applicable to patients who have expressed interest in self-directed care or desire to participate actively in their treatment. Finally, the use of self-report to measure adherence may limit our findings. Previous studies have shown that individuals tend to overestimate their adherence to medications ( 43 , 44 , 46 ). Self-report measures of adherence are less reliable than objective measures (for example, pill counts) and may also be less reliable than pharmacy records. Without corroborating evidence from external sources, a bias toward overestimation of adherence exists. We attempted to correct for this bias by using a highly stringent definition of adherence.
Conclusions
Our results indicate that psychiatric advance directives have the potential to be useful tools in facilitating medication treatment decisions between physicians and patients. In this study, completing a psychiatric advance directive allowed participants to express their preferences about medications and may have positively influenced medication adherence up to a year later. Individuals who requested medications in their psychiatric advance directive were more likely to be taking those medications a year later. Further, individuals who were taking at least one medication that they had requested in their psychiatric advance directive were significantly more likely than those who were not taking a requested medication to adhere to their medication regimen. This suggests that wider use of psychiatric advance directives could increase patient participation in medication choice and potentially improve adherence to treatment regimens.
Acknowledgments and disclosures
This study was funded by grants 5-R01-MH-063949, T32-MH019117, and K02-MH67864 from the National Institutes of Health and by the John D. and Catherine T. MacArthur Foundation.
Dr. Swanson and Dr. Swartz have received research support from Eli Lilly. Dr. Swartz has also received consulting and educational fees from AstraZeneca, Bristol-Myers Squibb, Eli Lilly, and Pfizer. The other authors report no competing interests.
1. Bebbington PE: The content and context of compliance. International Clinical Psychopharmacology 9(suppl 5):41–50, 1995Google Scholar
2. Perkins DO: Adherence to antipsychotic medications. Journal of Clinical Psychiatry 60(suppl 21):25–30, 1999Google Scholar
3. Rittmannsberger H, Pachinger T, Keppelmuller P, et al: Medication adherence among psychotic patients before admission to inpatient treatment. Psychiatric Services 55:174–179, 2004Google Scholar
4. Scott J, Pope M: Nonadherence with mood stabilizers: prevalence and predictors. Journal of Clinical Psychiatry 63:384–390, 2002Google Scholar
5. Weiden PJ, Kozma C, Grogg A, et al: Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatric Services 55:886–891, 2004Google Scholar
6. Rogers A, Day JC, Williams B, et al: The meaning and management of neuroleptic medication: a study of patients with a diagnosis of schizophrenia. Social Science and Medicine 47:1313–1323, 1998Google Scholar
7. Bissell P, May CR, Noyce PR: From compliance to concordance: barriers to accomplishing a re-framed model of health care interactions. Social Science and Medicine 58:851–862, 2004Google Scholar
8. Mitchell AJ: Adherence behaviour with psychotropic medication is a form of self-medication. Medical Hypotheses 68:12–21, 2007Google Scholar
9. Srebnik D, LaFond J: Advance directives for mental health services: current perspectives and future directions. Psychiatric Services 50:919–925, 1999Google Scholar
10. Swanson JW, Tepper MC, Backlar P, et al: Psychiatric advance directives: an alternative to coercive treatment? Psychiatry 63:160–172, 2000Google Scholar
11. Swartz MS, Stroup TS, McEvoy JP, et al: What CATIE found: results from the schizophrenia trial. Psychiatric Services 59:500–506, 2008Google Scholar
12. Falkai P: Limitations of current therapies: why do patients switch therapies? European Neuropsychopharmacology 18(suppl 3):S135–S139, 2008Google Scholar
13. Fleck DE, Keck PE Jr, Corey KB, et al: Factors associated with medication adherence in African American and white patients with bipolar disorder. Journal of Clinical Psychiatry 66:646–652, 2005Google Scholar
14. Johnson FR, Ozdemir S, Manjunath R, et al: Factors that affect adherence to bipolar disorder treatments: a stated-preference approach. Medical Care 45:545–552, 2007Google Scholar
15. Robinson DG, Woerner MG, Alvir JMJ, et al: Predictors of medication discontinuation by patients with first-episode schizophrenia and schizoaffective disorder. Schizophrenia Research 57:209–219, 2002Google Scholar
16. Holzinger A, Loffler W, Muller P, et al: Subjective illness theory and antipsychotic medication compliance by patients with schizophrenia. Journal of Nervous and Mental Disease 190:597–603, 2002Google Scholar
17. Verdoux H, Lengronne J, Liraud F, et al: Medication adherence in psychosis: predictors and impact on outcome: a 2-year follow-up of first-admitted subjects. Acta Psychiatrica Scandinavica 102:203–210, 2000Google Scholar
18. Coldham EL, Addington J, Addington D: Medication adherence of individuals with a first episode of psychosis. Acta Psychiatrica Scandinavica 106:286–290, 2002Google Scholar
19. Day JC, Bentall RP, Roberts C, et al: Attitudes toward antipsychotic medication: the impact of clinical variables and relationships with health professionals. Archives of General Psychiatry 62:717–724, 2005Google Scholar
20. Kozuki Y, Froelicher ES: Lack of awareness and nonadherence in schizophrenia. Western Journal of Nursing Research 25:57–74, 2003Google Scholar
21. Tunis SL, Faries DE, Stensland MD, et al: An examination of factors affecting persistence with initial antipsychotic treatment in patients with schizophrenia. Current Medical Research and Opinion 23:97–104, 2007Google Scholar
22. Draine J, Solomon P: Explaining attitudes toward medication compliance among a seriously mentally ill population. Journal of Nervous and Mental Disease 182:50–54, 1994Google Scholar
23. Seo MA, Min SK: Development of a structural model explaining medication compliance of persons with schizophrenia. Yonsei Medical Journal 46:331–340, 2005Google Scholar
24. Howgego IM, Yellowlees P, Owen C, et al: The therapeutic alliance: the key to effective patient outcome? A descriptive review of the evidence in community mental health case management. Australian and New Zealand Journal of Psychiatry 37:169–183, 2003Google Scholar
25. Patall EA, Cooper H, Robinson JC: The effects of choice on intrinsic motivation and related outcomes: a meta-analysis of research findings. Psychological Bulletin 134:270–300, 2008Google Scholar
26. Williams G, Freedman Z, Deci E: Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care 21:1644–1651, 1998Google Scholar
27. Williams G, Rodin G, Ryan R, et al: Autonomous regulation and long-term medication adherence in adult outpatients. Health Psychology 17:269–276, 1998Google Scholar
28. Bellg A: Maintenance of health behavior change in preventive cardiology: internalization and self-regulation of new behaviors. Behavior Modification 27:103–131, 2003Google Scholar
29. Scheyett A, Kim M, Swanson J, et al: Psychiatric advance directives: a tool for consumer empowerment and recovery. Psychiatric Rehabilitation Journal 31:70–75, 2007Google Scholar
30. Elbogen E, Swanson JW, Swartz MS, et al: Effectively implementing psychiatric advance directives to promote self-determination of treatment among people with mental illness. Psychology, Public Policy, and Law 13:273–288, 2007Google Scholar
31. Henderson C, Swanson JW, Szmukler G, et al: A typology of advance statements in mental health care. Psychiatric Services 59:63–71, 2008Google Scholar
32. Swanson JW, Swartz MS, Elbogen EB, et al: Facilitated psychiatric advance directives: a randomized trial of an intervention to foster advance treatment planning among persons with severe mental illness. American Journal of Psychiatry 163:1943–1951, 2006Google Scholar
33. Kim M, Van Dorn RA, Scheyett AM, et al: Understanding the personal and clinical utility of psychiatric advance directives: a qualitative perspective. Psychiatry 70:19–29, 2007Google Scholar
34. Srebnik D, Rutherford LT, Peto T, et al: The content and clinical utility of psychiatric advance directives. Psychiatric Services 56:592–598, 2005Google Scholar
35. Hammes BJ, Rooney BL: Death and end-of-life planning in one midwestern community. Archives of Internal Medicine 158:383–390, 1998Google Scholar
36. Advance Health Care Directives. Pub no 5088.01. Sacramento, Calif, Protection and Advocacy, 2000Google Scholar
37. Colvin ER, Hammes BJ: "If I only knew": a patient education program on advance directives. ANNA Journal 18:557–560, 1991Google Scholar
38. Elbogen EB, Swartz MS, Van Dorn RA, et al: Clinical decision making and views about psychiatric advance directives. Psychiatric Services 57:350–355, 2006Google Scholar
39. Byerly M, Thompson A, Carmody T, et al: Validity of electronically monitored medication adherence and conventional adherence measures in schizophrenia. Psychiatric Services 58:844–847, 2007Google Scholar
40. Velligan DI, Wang M, Diamond P, et al: Relationships among subjective and objective measures of adherence to oral antipsychotic medications. Psychiatric Services 58:1187–1192, 2007Google Scholar
41. Moerner MG, Mannuzza S, Kane JM: Anchoring the BPRS: an aid to improved reliability. Psychopharmacology Bulletin 24:112–117, 1988Google Scholar
42. Mayfield D, McLeod G, Hall P: The CAGE questionnaire: validation of a new alcoholism instrument. American Journal of Psychiatry 131:1121–1123, 1974Google Scholar
43. Brown RL, Rounds LA: Conjoint screening questionnaires for alcohol and drug abuse. Wisconsin Medical Journal 94:135–140, 1995Google Scholar
44. Leucht S, Kane JM, Kissling W, et al: Clinical implications of Brief Psychiatric Rating Scale scores. British Journal of Psychiatry 187:366–371, 2005Google Scholar
45. Srebnik D, Rutherford L, Peto T: The content and clinical utility of psychiatric advance directives. Psychiatric Services 56:592–598, 2005Google Scholar
46. Remington G, Kwon J, Collins A, et al: The use of electronic monitoring (MEMS) to evaluate antipsychotic compliance in outpatients with schizophrenia. Schizophrenia Research 90:229–237, 2007Google Scholar



