Coercion and Treatment Satisfaction Among Involuntary Patients
Increasing patients' satisfaction with treatment has long been regarded as an important target in mental health care ( 1 , 2 , 3 ). Some factors contributing to satisfaction among inpatients have been determined, with involuntary legal status consistently identified as a predictor of lower levels of satisfaction ( 4 ). However, less research has focused on treatment satisfaction and related factors specifically among involuntary patients ( 5 , 6 , 7 ).
Targeting involuntary patients' satisfaction is not only of clinical importance, but it is also an ethical issue, because these patients cannot discontinue their treatment, even when they are displeased with it. It might also be cost-effective, because treatment satisfaction has been associated with reduced risk of involuntary readmissions in this group ( 8 ). Studying involuntary patients' satisfaction might appear pointless, because they may be assumed to automatically be dissatisfied with their hospital care. However, previous research has revealed that a significant proportion of committed patients are positive overall toward their treatment ( 7 , 9 ).
Factors that are associated with satisfaction in this group remain poorly understood, and there is no evidence on how the experience of coercion, particularly common among committed patients ( 10 ), affects their evaluations. Higher levels of coercion at admission and during treatment might be associated with less treatment satisfaction. A link between clinical improvement and satisfaction has also been suggested ( 11 , 12 ). A better understanding of the reasons why some patients are more satisfied than others could inform the design of interventions to increase their satisfaction ( 8 , 13 , 14 ).
In the study presented here, we aimed to assess involuntary patients' satisfaction with treatment, its changes over time, and factors influencing it. We were particularly interested in the association between patients' satisfaction and coercion, both perceived and documented in the medical records. We also explored the potential significance of clinical and sociodemographic characteristics and clinical improvement.
Methods
Design, sample, and procedure
An observational prospective study on outcomes of involuntary hospitalization was conducted in 67 acute wards in 22 hospitals in England (run by eight provider organizations, that is, National Health Service Trusts), covering a geographical spread of urban and rural areas. Consecutive patients either involuntarily admitted (through sections 2, 3, or 4 of the Mental Health Act 1983 [MHA]) or voluntarily admitted whose status became involuntary within seven days of admission were recruited between July 2003 and July 2005. Section 4 allows detention for up to 72 hours, section 2 provides for assessment for up to 28 days, and section 3 allows treatment for up to six months. The detailed inclusion criteria and recruitment process have been described elsewhere ( 8 ).
Of the 1,570 eligible patients, 778 (50%) gave written informed consent to participate in the study and were interviewed within a week after admission. Of those, 546 (70%) were followed up at one month, 473 (61%) at three months, and 396 (51%) at one year. The patients were given £7 per interview to reimburse them for their time and expenses. Data are presented elsewhere for the reasons for not participating in the study or dropping out of follow-ups and for comparisons between all eligible patients and those interviewed at baseline and followed up ( 8 ). No substantial significant differences were found between all eligible patients and those interviewed at baseline and followed up ( 8 ).
The study design was approved by the Multi-Centre Research Ethics Committee (reference MREC/03/0/96). The collection of data on age, gender, ethnicity, diagnosis, legal status, and length of stay for all eligible patients to examine the representativeness of the participating sample was approved by the Patient Information Advisory Group (reference PIAG 2-10(d)/2005).
Measures
Satisfaction with treatment during the index hospitalization was measured at baseline, one month, three months, and one year on the Client's Assessment of Treatment Scale (CAT) ( 15 ). The scale comprises seven items on different aspects of hospital treatment ("Do you believe you are receiving the right treatment for you?" "Does your psychiatrist understand you and is he/she engaged in your treatment?" "Are relations with other staff members pleasant for you?" "Do you believe you are receiving the right medication for you?" "Do you believe the other elements of treatment are right for you?" "Do you feel respected and regarded well?" and "Has treatment been helpful for you?"). Each item is rated from 0, not at all, to 10, yes entirely; mean score of all items used), and the scale has been widely used with psychiatric inpatients ( 16 , 17 , 18 ).
Various aspects of perceived and documented coercion were tested as potential predictors of satisfaction. At baseline, participants were asked to rate their perceived levels of coercion at admission on the MacArthur Perceived Coercion Scale (MPCS) ( 19 ) and the Coercion Ladder (CL) ( 20 ). The MPCS measures five dimensions of perceived coercion—that is, control, choice, influence, freedom, and idea. Possible scores range from 0 to 5, with higher scores indicating higher levels of coercion. The CL is a visual analogue scale that has been used in conjunction with the MPCS ( 20 , 21 ) and measures the degree of coercion, threats, or pressure that patients experience. Possible scores range from 1 to 10, with higher scores indicating higher coercion. At the one-month follow-up, patients reported their perceived coercion during hospital treatment (as measured by CL), and they reported whether they had experienced any coercive measures—that is, restraint, forced medication, or seclusion (0, no measures, versus 1, at least one). Information on the same coercive measures within the first month of treatment (0, no measures, versus 1, at least one) was also collected from medical records (incident forms and day-to-day clinical notes). Restraint was defined as staff involuntarily holding at least one of the patient's limbs; forced medication was defined as the administration of medication against the patient's will, commonly by using restraint; and seclusion was defined as the involuntary placement of a patient in a designated locked room.
The following baseline and one-month follow-up variables were collected from medical records and were also assessed as potential predictors of satisfaction: age, gender, ethnicity (the United Kingdom census 2001 categories collapsed into two categories: white, 0, versus ethnic minority, 1), diagnosis ( ICD-10 categories collapsed into three categories: schizophrenia or other psychosis, F20–F29, 1; affective disorder, F30–F39, 2; and other, 3), legal status (section 3 of the MHA, 0, versus sections 2 or 4, 1) and the documented reasons for the index admission (risk to self, risk to others, severe danger to health, inability to care for self: yes, 1, versus no, 0, for each item). In baseline interviews, participants were asked to provide information on other characteristics: housing (with place to stay, 1, versus homeless, 0), employment (yes, 1, versus no, 0), living situation (living with others, 1, versus living alone, 0), past hospitalizations (yes, 1, versus no, 2). Researchers also rated patients' severity of symptoms on the Brief Psychiatric Rating Scale (BPRS) ( 21 ) (possible scores range from 24 to 168, with higher scores indicating more severe symptoms), and they rated global functioning on the Global Assessment of Functioning (GAF) ( 22 ) (possible scores range from 1 to 100, with higher scores indicating enhanced functioning). Improvement on the BPRS and GAF were measured as the difference between baseline and one-month follow-up scores. Information on the total length of stay for the index admission was collected from medical records.
Statistical analysis
Descriptive statistics on satisfaction at all time points and on baseline and follow-up characteristics potentially associated with satisfaction were calculated. In order to check the internal consistency of the satisfaction scale in this group, Cronbach's alpha scores were calculated for all time points. The associations between the various measures of perceived coercion (MPCS and CL mean scores at baseline and at the one-month follow-up) were assessed with Pearson's r correlations, and the relationship between self-reported and documented coercive measures were assessed with chi square tests.
Two different models predicting treatment satisfaction were produced. First, potential baseline predictors of satisfaction were explored in a mixed-effect model combining satisfaction scores from all time points (baseline, one month, three months, and one year) as an outcome. To account for possible correlations among repeated measurements, a linear mixed-effect model was employed, with patients' characteristics measured at baseline and time as fixed effects and participant as a random effect ( 23 ). Missing values for the follow-up assessments were assumed to occur at random.
Second, potential baseline and treatment-process predictors of follow-up satisfaction with treatment, measured after the first month of treatment, were explored in another mixed-effect model with combined satisfaction scores from the one-month, three-month, and one-year follow-ups as an outcome. In this second model, baseline satisfaction scores could not be combined with the follow-up scores as an outcome, because some of the potential predictors were measured after baseline, at the one-month follow-up.
The mixed-effect model analysis for each model was performed in three steps. First, a simple mixed model with just time effect was estimated in order to estimate the crude effect of time, and pairwise comparisons were also made. In the second step, univariate mixed-model analysis was performed and variables that were found significant at p≤.10 were subsequently considered in multivariate mixed-model analysis. In the third step, variables that became nonsignificant at p=.05 in the multivariable model were excluded one by one until all the variables became significant (p<.05). As a sensitivity analysis, the final models were repeated, with controls for the effect of the provider organization and length of hospital stay.
Results
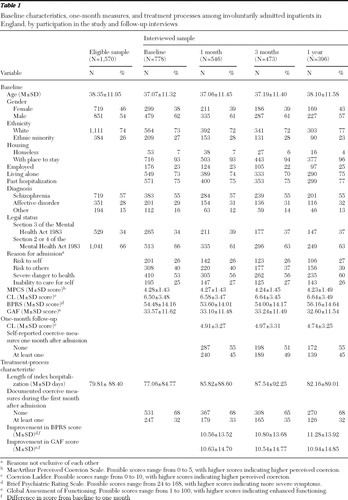
Table 1 summarizes baseline, one-month follow-up, and treatment-process characteristics for all eligible patients and study participants at all time points.
 |
Satisfaction with treatment over time and internal consistency
There was a significant increase as measured by the CAT in patients' satisfaction between baseline (5.51±2.90) and all follow-ups (5.81±2.78 at one month, 6.03±2.78 at three months, and 5.81±2.63 at one year), with the highest satisfaction reported at three months. Changes between one and three months were also statistically significant, although changes between three months and one year did not reach significance. At all time points the majority of participants reported a mean satisfaction score above 5 (N=390, 58%, at baseline; N=325, 63%, at one month; N=292, 66%, at three months, and N=235, 63%, at one year; all data were not available for all respondents). The Cronbach's alpha for total scores on this scale was .90 for baseline, .91 for one month, .92 for three months, and .90 for one year.
Mean satisfaction with specific treatment aspects ranged from 4.76±3.83 to 6.79±3.02 at baseline, 5.02±3.68 to 6.85±2.91 at one month, 5.57±3.61 to 6.90±2.79 at three months, and 5.28±3.49 to 6.74±2.84 at one year. At all time points participants reported the lowest scores on the item rating satisfaction with their psychiatrist and the highest scores on the item rating satisfaction with other staff.
Coercion measures
Perceived coercion ranged from 0 to 5 on the MPCS (frequencies: 6% had a total score of 0, 3% a score of 1, 4% a score of 2, 5% a score of 3, 9% a score of 4, and 73% a score of 5) and from 1 to 10 on the CL at admission (frequencies: 18% had a score of 1, 4% a score of 2, 6% a score of 3, 3% a score of 4, 8% a score of 5, 3% a score of 6, 8% a score of 7, 9% a score of 8, 7% a score of 9, and 35% a score of 10) and at one month (frequencies: 25% had a score of 1, 6% a score of 2, 10% a score of 3, 7% a score of 4, 10% a score of 5, 6% a score of 6, 6% a score of 7, 9% a score of 8, 4% a score of 9, and 16% a score of 10). These measures were significantly, but weakly to moderately, correlated at all time points, with coefficients not exceeding r=.43. The chi square test between self-reported and documented coercive measures was significant ( χ2 =16.34, df=1, p<.001).
Model 1
Table 2 shows baseline factors that were univariately associated with treatment satisfaction (combined scores from baseline and all follow-ups) and the final multivariable model.
 |
In multivariable model 1, patients who were detained on sections 2 or 4 of the MHA and those with lower perceived coercion at admission on both the MPCS and the CL were more satisfied with their treatment. Having no past hospitalization was univariately associated with higher satisfaction, but it lost significance in the multivariable model.
When the model was repeated while controlling for the effect of provider organization and length of hospital stay as a sensitivity analysis, all the above predictors except for perceived coercion on the MPCS remained significant.
Model 2
Multivariable model 2 shows baseline and treatment-process factors associated with satisfaction ( Table 2 ). In the model, patients with higher levels of perceived coercion at admission and during treatment (as rated by CL) and those reporting at least one coercive measure were less satisfied at the follow-ups. Those with higher symptom improvement one month after admission (as rated by BPRS) were more satisfied. Perceived coercion at admission on the MPCS and improvement in global functioning (as rated by GAF) were univariately associated with satisfaction, but they did not remain significant in the multivariable model. Similarly, detention on sections 2 or 4 of the MHA did not reach significance in the model, although it demonstrated a trend (p=.053).
When the model was repeated while controlling for the effect of provider organizations and length of stay, all of the above predictors remained significant.
Discussion
Main findings
On average, patients' ratings of satisfaction with their treatment were in the positive half (that is, a score over 5) of the full range of a scale that ranges from 0 to 10. The positive ratings were found at all time points, and there was a statistically significant, although small, increase in satisfaction within three months after admission. Between three months and a year, satisfaction scores decreased, but not significantly, and mean satisfaction at one year was still significantly higher than at admission. Patients' perceptions of coercion were consistently associated with treatment satisfaction, with those reporting less coercion overall (both at admission and during the first month of treatment) and not having experienced coercive measures (such as restraint, forced medication, and seclusion) being more satisfied. MPCS scores at admission were the only measure of perceived coercion that, although associated with overall satisfaction (model 1) and univariately associated with satisfaction at the follow-ups, were not a statistically significant predictor in the multivariable model 2 when other factors were controlled for (unlike CL scores, which remained significant). In contrast to perceived coercion, we did not find an association between coercive measures that were documented in the medical records and satisfaction.
Symptom improvement, an obvious target for treatment (along with the reduction of risk), was also associated with higher levels of satisfaction. Patients detained on section 3 of the MHA, allowing for the longest detention in the hospital and for coercive interventions when necessary, were more dissatisfied than those detained on sections 2 or 4. No baseline demographic or clinical factors were linked to patients' satisfaction with their treatment.
Strengths and limitations
This is the largest national prospective study of involuntary hospitalization to date. Although patients' views on whether their commitment was appropriate or beneficial have been sought in earlier, smaller studies, using mostly single items ( 7 , 11 , 12 , 24 ), satisfaction with treatment on an established scale has rarely been assessed among involuntary patients. The scale used in this study is likely to provide more reliable scores than single items and reflects a relatively wide concept of satisfaction. It captures patients' overall appraisal of their hospital treatment and their assessment of specific treatment components. Despite addressing different aspects of care, the scale has high internal consistency, and the mean score summarizes patients' personal experience and evaluation of hospital treatment. The prospective design allowed the assessment of changes in patients' evaluations over time. A wide range of baseline characteristics and admission and treatment-process factors were tested as potential predictors of satisfaction. Although only 50% of the eligible patients took part in the study, the response and attrition rates were satisfactory for this group, compared with earlier studies ( 8 ). Comparisons between all eligible patients and those participating revealed no major differences between the groups. One might, however, speculate as to whether patients who refused to participate in interviews were less satisfied with treatment.
The study also has several limitations. Because this was an observational study, no conclusions can be drawn on the causality of associations. One might argue that perceived coercion and satisfaction are not distinct concepts: they are both self-reported and might reflect patients' overall evaluations of their treatment ( 25 ). They were, however, measured at different time points and the analysis was prospective. Illness characteristics and symptom severity might have confounded the relationship between satisfaction and perceived coercion. However, diagnosis and baseline severity of symptoms and global functioning showed no significant associations with satisfaction. Although both incident forms and day-to-day clinical notes were checked to assess documented coercion, the documentation of incidents in the records might have been inaccurate. Although a number of factors were tested as potential predictors of satisfaction, other factors that were not assessed (for example, familiarity with professionals involved in the admission and therapeutic relationships during treatment) might also be of importance. Finally, memory biases might have influenced patients' reports, especially as some participants may have been hospitalized briefly but were asked about their experience up to a year after the index admission.
Implications
The results indicate that even when treated involuntarily, patients might not hold particularly negative views regarding their treatment. As shown previously, involuntary legal status is not synonymous with overall extreme negative views of hospital treatment ( 5 , 6 , 10 ). Patients' ratings of satisfaction improved significantly within three months after admission, which is also consistent with evidence from other studies ( 9 , 26 ). The satisfaction ratings in our study, however, are still relatively low in comparison to those of voluntary inpatients—for example, voluntary inpatients' mean scores on the same scale ranged between 7.33 at admission and 8.06 at discharge in five European countries ( 16 ) and between 6.77 at discharge and 6.15 three months after discharge in London ( 17 ).
Increasing involuntary patients' satisfaction with their treatment is a challenge for inpatient services. This study identified a consistent link between perceived coercion (at admission and during treatment) and satisfaction. Although perceiving some coercion in a situation that is by definition coercive may be warranted, reducing patients' feelings of coercion might lead to higher satisfaction overall ( 27 , 28 , 30 ). The importance of perceived rather than documented coercion suggests that patients' feelings of coercion may depend less on the use of specific coercive measures and more on overall experiences of involuntary treatment and on the way such treatment is delivered, negotiated, and explained. These findings are in line with previous research suggesting that when patients perceive procedural justice (that is, when their opinions are heard and taken into account and treatment decisions are made in good faith and with their best interests in mind) and feel persuaded rather than forced or threatened, they feel less coerced, even under objectively coercive circumstances ( 10 , 27 , 31 , 32 , 33 , 34 , 35 ). Qualitative research has also shown that involuntary patients feel aggrieved about not participating in their care and having to comply with hospital regulations, even in the absence of physical force ( 14 ).
Another interesting finding was that MPCS scores lost significance in the multivariable model 2, although CL scores did not. Although MPCS has good psychometric properties and has been widely used in U.S. studies ( 19 ), findings from a multicenter Nordic study indicate that acutely ill involuntary patients might find the concepts that it measures (control, choice, influence, freedom, and idea) abstract and harder to understand, whereas the CL might be more user friendly ( 36 ).
Conclusions
Improving involuntary patients' satisfaction with treatment may require enhanced participation of patients in their care and effective communication between staff and patients, rather than only a reduction in the use of coercive measures. This may be a major challenge for inpatient services, for which ready-made solutions do not yet exist.
Acknowledgments and disclosures
This study was funded by grant 0230072 from the Department of Health, United Kingdom. The views expressed in this article are those of the authors and not necessarily those of the Department of Health. The funding source had no role in the study design and conduct of the study, data collection, management, data analysis, data interpretation, or writing of the report or with the preparation, review, or approval of the manuscript. The authors also thank Ksenija Yeeles, B.Sc., Olive Bennewith, B.A., Louisa Bolt, B.Sc., Simon Clarke, B.Sc., Susan Collinson, Ph.D., Suzi Curtis, D.Clin.Psych., Rosemary Davies, M.A., Rebekka Evans, D.Clin.Psych., Sarah Grant, M.Sc., Danielle Oliver, B.Sc., Felicitas Rost, M.Sc., Rebecca Read, B.Sc., Rajinder Sidhu, Ph.D., Emma Williams, Ph.D., Jessica Zetteler, D.Clin.Psych., for their contributions to the study.
The authors report no competing interests.
1. Rossberg J, Friis S: Patients' and staff's perceptions of the psychiatric ward environment. Psychiatric Services 55:798–803, 2004Google Scholar
2. Ruggeri M, Lasalvia A, Salvi G, et al: Applications and usefulness of routine measurement of patients' satisfaction with community-based mental health care. Acta Psychiatrica Scandinavica 116:53–65, 2007Google Scholar
3. Hackman A, Brown C, Yang Y, et al: Consumer satisfaction with inpatient psychiatric treatment among persons with severe mental illness. Community Mental Health Journal 43:551–564, 2007Google Scholar
4. Greenwood N, Key A, Burns T, et al: Satisfaction with in-patient psychiatric services: relationship to patient and treatment factors. British Journal of Psychiatry 174:159–163, 1999Google Scholar
5. Spensley J, Edwards DW, White E: Patient satisfaction and involuntary treatment. American Journal of Orthopsychiatry 50:725–729, 1980Google Scholar
6. Svensson B, Hansson L: Patient satisfaction with inpatient psychiatric care. Acta Psychiatrica Scandinavica 90:379–384, 1994Google Scholar
7. Kjellin L, Anderson K, Candefjord I: Ethical benefits and costs of coercion in short-term inpatient psychiatric care. Psychiatric Services 48:1567–1570, 1997Google Scholar
8. Priebe S, Katsakou C, Amos T, et al: Patients' views and readmissions 1 year after involuntary hospitalisation. British Journal of Psychiatry 194:49–54, 2009Google Scholar
9. Katsakou C, Priebe S: Outcomes of involuntary hospital admission: a review. Acta Psychiatrica Scandinavica 114:232–241, 2006Google Scholar
10. Monahan J, Hoge S, Lidz C, et al: Coercion and commitment: understanding involuntary mental hospital admission. International Journal of Law and Psychiatry 18:249–263, 1995Google Scholar
11. Kane JM, Quitkin F, Rifkin A, et al: Attitudinal changes of involuntarily committed patients following treatment. Archives of General Psychiatry 40:374–377, 1983Google Scholar
12. Beck JC, Golowka EA: A study of enforced treatment in relation to Stone's "thank you" theory. Behavioral Sciences and the Law 6:559–566, 1988Google Scholar
13. Salize HJ, Dressing H: Coercion, involuntary treatment and quality of mental health care: is there any link? Current Opinion in Psychiatry 18:576–584, 2005Google Scholar
14. Katsakou C, Priebe S: Patients' experiences of involuntary hospital admission and treatment: a review of qualitative studies. Epidemiologia e Psichiatria Sociale 16:172–178, 2007Google Scholar
15. Priebe S, Gruyters T, Heinze M, et al: Subjective evaluation criteria in psychiatric care: methods of assessment for research and general practice [in German]. Psychiatrische Praxis 22:140–144, 1995Google Scholar
16. Kallert TW, Priebe S, McCabe R, et al: Are day hospitals effective for acutely ill psychiatric patients? A European multicentre randomized controlled trial. Journal of Clinical Psychiatry 68:278–287, 2007Google Scholar
17. Priebe S, Jones G, McCabe R, et al: Effectiveness and costs of acute day hospital treatment compared with conventional in-patient care. British Journal of Psychiatry 188:243–249, 2006Google Scholar
18. Kallert TW, Glöckner M, Onchev G, et al: The EUNOMIA project on coercion in psychiatry: study design and preliminary data. World Psychiatry 4:168–172, 2005.Google Scholar
19. Gardner W, Hoge S, Bennett N, et al: Two scales for measuring patients' perceptions of coercion during mental hospital admission. Behavioral Sciences and the Law 11:307–321, 1993Google Scholar
20. Hoyer G, Kjellin L, Engberg M, et al: Paternalism and autonomy: a presentation of a Nordic study on the use of coercion in the mental health care system. International Journal of Law and Psychiatry 25:93–108, 2002Google Scholar
21. Lukoff D, Nuechterlien K, Ventura J: Manual for the Expanded Brief Psychiatric Rating Scale. Schizophrenia Bulletin 13:261–276, 1986Google Scholar
22. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
23. Fitzmaurice GM, Laird NM, Ware JH: Applied Longitudinal Analysis. New York, Wiley, 2004Google Scholar
24. Edelsohn GA, Hiday VA: Civil commitment: a range of patient attitudes. Bulletin of the American Academy of Psychiatry and the Law 18:65–66, 1990Google Scholar
25. Hansson L, Bjorkman T, Priebe S: Are important patient-rated outcomes in community mental health care explained by only one factor? Acta Psychiatrica Scandinavica 116:113–118, 2007Google Scholar
26. Gardner W, Lidz CW, Hoge SK, et al: Patients' revisions of their beliefs about the need for hospitalization. American Journal of Psychiatry 156:1385–1391, 1998Google Scholar
27. Bennett N, Lidz CW, Monahan J, et al: Inclusion, motivation, and good faith: the morality of coercion in mental hospital admission. Behavioral Sciences and the Law 11:295–306, 1993Google Scholar
28. Watson A, Angell B: Applying procedural justice theory to law enforcement's response to persons with mental illness. Psychiatric Services 58:787–793, 2007Google Scholar
29. Lasalvia A, Bonetto C, Salvi G, et al: Predictors of changes in needs for care in patients receiving community psychiatric treatment: a 4-year follow-up study. Acta Psychiatrica Scandinavica 116:66–76, 2007Google Scholar
30. Sorgaard KW: Patients' perception of coercion in acute psychiatric wards: an intervention study. Nordic Journal of Psychiatry 58:299–304, 2004Google Scholar
31. Lidz CW, Hoge SK, Gardner W, et al: Perceived coercion in mental hospital admission: pressures and process. Archives of General Psychiatry 52:1034–1039, 1995Google Scholar
32. Hiday VA, Swartz MS, Swanson J, et al: Patient perceptions of coercion in mental hospital admission. International Journal of Law and Psychiatry 20:227–241, 1997Google Scholar
33. Lidz CW, Mulvey EP, Hoge SK, et al: Factual sources of psychiatric patients' perceptions of coercion in the hospital admission process. American Journal of Psychiatry 155:1254–1260, 1998Google Scholar
34. Swartz MS, Wagner HR, Swanson JW, et al: Consumers' perceptions of the fairness and effectiveness of mandated community treatment and related pressures. Psychiatric Services 55:780–785, 2004Google Scholar
35. McKenna BG, Simpson A, Coverdale JH, et al: An analysis of procedural justice during psychiatric hospital admission. International Journal of Law and Psychiatry 24:573–581, 2001Google Scholar
36. Høyer G, Kjellin L, Engberg M, et al: Paternalism and autonomy: a presentation of a Nordic study on the use of coercion in the mental health care system. International Journal of Law and Psychiatry 25:93–108, 2002Google Scholar



