Effectiveness of Education Programs in Changing Clinicians' Attitudes Toward Treating Borderline Personality Disorder
A review of recent studies revealed that attitudes toward patients diagnosed as having borderline personality disorder tend to be negative and derogatory ( 1 , 2 , 3 , 4 ). In terms of promoting more positive attitudes, access to education about borderline personality disorder has been demonstrated to have a significant effect on clinicians' attitudes toward working with persons with this disorder. After a two-day training session on borderline personality disorder, clinicians found an increased optimism, enthusiasm, and positive feeling toward working with these patients, which was maintained at three- to five-month follow-up ( 5 ). Further assessment of attitudes with a larger sample of clinicians from public mental health and substance abuse services also supported an increase in confidence in working with patients with borderline personality disorder after specific training ( 6 ). However, a review of the literature failed to find distinctions between the different theoretical frameworks that can be taught in education programs to instigate improvement in clinicians' attitudes.
A common approach used in public mental health services, and one of the core practice techniques I use when working with borderline personality disorder, is the cognitive-behavioral therapy approach, which identifies the disorder as stemming from a biological problem with emotional regulation ( 7 ). These problems with regulation then combine with a childhood environment that has been invalidating of the patient's emotions, creating a cycle of intense affect ( 7 ). The chronic invalidation of emotional responses results in the patient's having inadequate coping skills for normal life; the self-injury episodes observed among these patients are conceptualized as their way of coping with intense affect ( 7 ). Cognitive-behavioral therapy, particularly a form known as dialectical behavior therapy, has been demonstrated to be effective in the treatment of personality disorders ( 8 ). The effectiveness of the cognitive-behavioral theoretical framework in facilitating clinician understanding and empathy has yet to be studied.
More traditional conceptual frameworks of borderline personality disorder stem from the psychoanalytic paradigm. One of the first pioneers to discuss the masochistic tendencies of some patients, including deliberate self-harm behaviors, was Sigmund Freud ( 9 ). Freud described a moral form of masochism "where the subject, as a result of an unconscious sense of guilt, seeks out the position of victim without any sexual pleasure being directly involved" ( 10 ). I have observed when treating these patients that often a sense of guilt and need for punishment are expressed before, during, or after an act of self-harm. Following the Freudian line of thought on moral masochism, the true source of this guilt is not an immediate stressor in the patient's environment (as is often reported by the patient after self-harm); rather, it is attached to some past trauma ( 11 , 12 ). Although it is a concept that was developed in 1924, I have successfully used the premise of moral masochism in the conceptualization of behavioral disturbance, and therefore, it may have some value in educating clinicians in understanding deliberate self-harm behaviors observed in today's presentation of borderline personality disorder.
This study aimed to address the gap in the literature by examining two types of theoretical frameworks (cognitive-behavioral and psychoanalytic) to see how they compared in changing clinicians' attitudes toward deliberate self-harm behaviors in borderline personality disorder. Education programs using the cognitive-behavioral framework of dialectical behavior therapy or the psychoanalytic framework of moral masochism were provided to clinicians between January 2007 and March 2008. To determine attitude change, a standardized assessment tool for quantifying attitude levels was used.
Methods
The emergency medicine and mental health clinicians from two Australian health services (Ballarat Health Services and Barwon Health) and a New Zealand health service (Nelson Marlborough District Health Board) who were registered health practitioners and had some contact with patients with borderline personality disorder were asked to participate in this study, and a random multistage sampling procedure was used to assign these participants to the three groups: cognitive-behavioral education program, psychoanalytic education program, and control group (no education program). In addition, emergency medicine clinicians at Ballarat Health Services who did not attend the education program were invited to participate in the control condition. Similarly, mental health clinicians at Ballarat Health Services who were employed in the rural areas were sent a letter through the mail inviting them to participate in the control condition.
Of the 445 clinicians who were asked to participate in this study, 140 accepted (31% overall response rate). There was a 61% acceptance rate (N=54 of 89) from four psychiatric and emergency medicine departments within Ballarat Health Services, a 13% acceptance rate from all psychiatric and emergency medicine departments within Barwon Health (N=30 of 224), and a 42% acceptance rate from all psychiatric and emergency medicine departments within Nelson Marlborough District Health Board (N=56 of 132). Forty-one (29%) were assigned to the control group, 50 (36%) were assigned to the cognitive-behavioral group, and 49 (35%) were assigned to the psychoanalytic group.
Participants were provided with an explanatory statement and consent form. The explanatory statement differed for the experimental and control groups in terms of requirements of participation; however, the statement for the experimental groups did not reveal the theoretical framework to be utilized in the applicable education program. This was revealed after the outcome measures were completed.
Participants were provided with a demographic questionnaire (gender, years of clinical experience, formal education completed, primary occupation, service setting, and average clinical contact with patients with borderline personality disorder) and were given the Attitudes Towards Deliberate Self-Harm Questionnaire (ADSHQ) ( 4 ). All participants were asked to consider their responses on the ADSHQ only in relation to their contacts with patients who deliberately harmed themselves and were diagnosed as having borderline personality disorder. The ADSHQ consists of 33 items scored on a 4-point Likert scale ranging from 1, strongly disagree, to 4, strongly agree. In order to reduce response bias, one-third of the items are phrased in the negative direction. Possible scores range from 33 to 132, with higher scores indicating more positive attitudes. Sample items are "Dealing with self harm patients is a waste of the health care professional's time," "I deal effectively with deliberate self harm patients," and "Self harm patients just clog up the system." In the study presented here, the Cronbach's alpha coefficient for the total scale was satisfactory (.75).
The education programs were held during staff development time at each health service. The first 45 minutes of both types of education programs (cognitive-behavioral and psychoanalytic) covered research findings on attitudes toward borderline personality disorder, prevalence rates, DSM-IV diagnostic criteria, etiological factors, definitions and rates of self-harm and suicide, and therapeutic responses to borderline personality disorder. The next 45 minutes was spent discussing and illustrating the applicable concepts of the theoretical discussions of borderline personality disorder using three case studies of female patients diagnosed as having this disorder. The cognitive-behavioral education program (which covered a dialectic behavioral therapy approach) used these three case studies to illustrate the use of deliberate self-harm behaviors as a means by which to modulate overwhelming affective experiences among patients who had developed affective instability through a process of invalidation in childhood. The psychoanalytic education program (which covered the theoretical framework of moral masochism) used these three case studies to illustrate the use of deliberate self-harm behaviors as a process by which to discharge an unconscious sense of guilt. The psychoanalytic education program detailed how the women in the case studies had experienced some form of psychological trauma in childhood that was reawakened by current social stressors. Clinical guidelines, including guidelines on crisis intervention in emergency departments ( 13 ) and the national clinical practice guideline on self-harm ( 14 ), were discussed in the last 30 minutes of the lecture. I presented the education programs in a lecture format, with a total of two hours of lecturing.
At the end of the education program, all participants in the experimental conditions were required to complete the ADSHQ again; this was collected before the participants returned to their usual clinical practice. Six months after completing the measure (for the control group) or attending the education program (for the two experimental groups), participants received the ADSHQ through the mail.
The study received ethical approval by Monash University and the three health services.
Results
Of the 140 clinicians who participated in the original research program, 22 (16%) had left the health services before the six-month follow-up; therefore, only 118 (84%) clinicians were available to participate. Of these, 65 participants (55%) responded to the follow-up request. Of these 65 participants, 25 (38%) were from the psychoanalytic experimental condition, 18 (28%) were from the cognitive-behavioral experimental condition, and 22 (34%) were from the control condition.
Among these 65 participants, 26 (40%) were male and 39 (60%) were female. Forty-eight (74%) were from the mental health service setting. The other 17 (26%) were emergency medicine clinicians. Across this sample, 47 (72%) were nurses, 11 (17%) were allied health professionals, and seven (11%) were medical practitioners. Nearly half held postgraduate qualifications (N=32, 49%), 25 (38%) had an undergraduate degree, and eight (12%) had hospital-based training. Twenty-six (40%) reported having more than 16 years of clinical experience, and 14 (22%) reported five or fewer years.
In terms of frequency of contact with patients with borderline personality disorder, 14 (22%) had daily contact, 31 (48%) had weekly contact, nine (14%) had contact every two weeks, and 11 (17%) had contact monthly or less frequently. In terms of prior training, 32 (49%) said that they had not received education on borderline personality disorder. The proportion of women was significantly less in the control group than the other two groups (seven women in the control group, or 32%, versus 14 women in the cognitive-behavioral group, or 78%, and 18 women in the psychoanalytic group, or 72%) ( χ2 =11.15, df=2, p<.01), but there were no other statistically significant differences between the groups in terms of service setting, level of university training, years of experience, completion of prior training, frequency of contact, and occupational areas.
Following a review of the data set that revealed a normal distribution and equal variance, univariate and multivariate analyses were conducted. No data were missing from the data set. The mean±SD scores on the ADSHQ across the three participant conditions are reported in Table 1 .
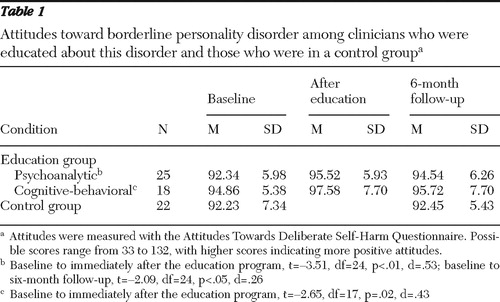 |
Data for the two experimental groups, psychoanalytic and cognitive-behavioral, indicated a statistically significant improvement in attitude ratings immediately after the education program, with medium effect sizes. At the six-month follow-up, the statistically significant improvement in attitude ratings was maintained only for the psychoanalytic condition, with a small effect size.
Although the follow-up ADSHQ score for the cognitive-behavioral group was higher than the pre-education score, the difference was not significant. As expected, there were no significant changes from baseline to follow-up in ADSHQ scores for participants within the control condition.
Discussion and conclusions
In this cohort of participants, a statistically significant improvement in attitude ratings toward working with patients with borderline personality disorder and understanding any associated deliberate self-harm behaviors was found immediately after attending an education program, across both the psychoanalytic and cognitive-behavioral theoretical frameworks. Both conceptualizations appear to be able to improve attitudes of emergency medicine and mental health clinicians. To address the current difficulties described in the literature with regard to existing negative attitudes toward this complex disorder, it appears that access to various forms of clinical education may improve attitudes. Access to targeted clinical education is therefore suggested for all clinicians who come into psychotherapeutic or medical contact with patients with borderline personality disorder.
Over a six-month period the statistically significant improvement in attitude ratings observed for participants in the cognitive-behavioral group was not maintained. The cognitive-behavioral paradigm, although well supported by empirical research as an efficacious treatment option ( 7 , 8 ), appeared here to be limited in its ability to maintain improved clinicians' attitudes over a longer duration. The psychoanalytic group, which received education on the theoretical framework of moral masochism, showed a small decline in attitude ratings over the six-month period; however, the statistically significant improvements in their attitude ratings were maintained with a small effect size. Although the lower baseline ratings for the psychoanalytic group, compared with the cognitive-behavioral group, need to be considered in interpreting the rating changes at follow-up, the statistical significance of the results found here suggest that clinicians who receive education on the unconscious processes underlying deliberate self-harm may develop a greater ability to empathize with the difficulties of the patient.
The conceptualization of behavioral disturbance in borderline personality disorder, according to a cognitive-behavioral framework, implies a level of consciousness by patients in their use of self-harm to relieve distress and cope with an aroused affective state. The difficulty is that repeated presentations of deliberate self-harm behaviors in response to an unappeased emotional state do not seem to generate compassionate responses by clinicians, with many evaluating the behaviors to be manipulative ( 3 ). Freud's concept of moral masochism from 1924 suggests that patients with borderline personality disorder who unconsciously engage deliberate self-harm show a reduced responsibility for their behavior. A clinician may rightly expect that a patient will describe conscious concerns in his or her life; however, unconscious aspects also need consideration. Allowing clinicians to develop greater insight into these unconscious processes appears to assist in a greater recognition of the complexity of this disorder. The moral masochism framework, which attributes the origin of deliberate self-harm to an unconscious sense of guilt related to past trauma, may indeed have some value in the conceptualization of behavioral disturbance in borderline personality disorder, through enabling an effective framework by which to interpret and thus understand such presentations.
The results of this study suggest that access to clinical education on borderline personality disorder can improve attitudes of emergency medicine and mental health clinicians and suggest that regular access to such education may help maintain positive attitudes, because the improved attitudes remained for both education groups at six-month follow-up. The usefulness of the shift in attitude ratings, averaging 2–3 points on the ADSHQ, in terms of true attitude change and clinical practice is not certain. The ADSHQ requires participants to respond with a clear indication of agreement or disagreement, with no neutral response allowed, which suggests that there may be some functional improvements in attitude ratings across the sample. Further limitations of this study are related to the sample size, and replication of this study with a larger sample is recommended to further understand the use of different theoretical frameworks in clinician education. Assessing the direct impact of clinician attitude change on clinical practice was beyond the scope of this study and remains a topic for future research.
Acknowledgments and disclosures
The author acknowledges the support and guidance of Leonardo Rodríguez, Ph.D., and Andrew Lewis, Ph.D., as well as the financial support of the School of Psychiatry, Psychology, and Psychological Medicine at Monash University. This study was undertaken in part for Ms. Commons Treloar to fulfill the requirements of a doctor of philosophy degree in psychological medicine at Monash University.
The author reports no competing interests.
1. Commons Treloar AJ, Lewis AJ: Professional attitudes towards deliberate self-harm in patients with borderline personality disorder. Australian and New Zealand Journal of Psychiatry 42:578–584, 2008Google Scholar
2. Bowers L, Allan T: The Attitudes to Personality Disorder Questionnaire: psychometric properties and results. Journal of Personality Disorders 20:281–293, 2006Google Scholar
3. Potter NN: What is manipulative behavior anyway? Journal of Personality Disorders 20:139–156, 2006Google Scholar
4. McAllister M, Creedy D, Moyle W, et al: Nurses' attitudes towards clients who self harm. Journal of Advanced Nursing 40:578–586, 2002Google Scholar
5. Krawitz R: Borderline personality disorder: clinician attitude change following brief training. Australian and New Zealand Journal of Psychiatry 34:A40, 2000Google Scholar
6. Krawitz R: Borderline personality disorder: attitudinal change following training. Australian and New Zealand Journal of Psychiatry 38:554–559, 2004Google Scholar
7. Linehan MM: Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York, Guilford, 1993Google Scholar
8. Leichsenring F, Leibing E: The effectiveness of psychodynamic therapy and cognitive-behavior therapy in the treatment of personality disorders: a meta-analysis. American Journal of Psychiatry 160:1223–1232, 2003Google Scholar
9. Freud S: The economic problem of masochism; in The Standard Edition of the Complete Psychological Works of Sigmund Freud, Vol 19. Edited and translated by Strachey J. London, Hogarth, 1924Google Scholar
10. Laplanche J, Pontalis JB: The Language of Psychoanalysis. London, Karnac Books, 1988Google Scholar
11. McAllister M: Multiple meanings of self harm: a critical review. International Journal of Mental Health Nursing 12:177–185, 2003Google Scholar
12. Van der Kolk B: The compulsion to repeat the trauma: re-enactment, re-victimization, and masochism. Psychiatric Clinics of North America 12:389–411, 1989Google Scholar
13. Mitchell P: Crisis Intervention and Primary Care: Evaluation of the National Youth Suicide Prevention Strategy: Technical Report, Vol 3. Melbourne, Australia, Australian Institute of Family Studies, 2000Google Scholar
14. Self-Harm: The Short-Term Physical and Psychological Management and Secondary Prevention of Self-Harm in Primary and Secondary Care: National Clinical Practice Guideline no 16. Leicester, British Psychological Society, National Collaborating Centre for Mental Health, 2004Google Scholar



