A Cost Analysis of San Diego County's REACH Program for Homeless Persons
Housing-first programs provide targeted groups of homeless people direct or nearly direct placement into permanent housing by using a consumer-driven, psychosocial rehabilitation model ( 1 ). Although supportive services are readily available, housing-first programs do not require that participants enter treatment or achieve sobriety before they receive housing. Assertive outreach is used to engage homeless people with mental illness who are reluctant to enter shelters or engage in services. A low-demand model is used to respond to substance abuse by addressing the harms caused by risk-taking behavior without requiring clients to abandon the behavior altogether. A continued effort is made to provide case management services and to hold housing for clients who leave the program housing for short periods (usually up to 90 days).
In 1999 the California state legislature passed California Assembly Bill (AB) 34, which provided $10 million for pilot programs offering integrated housing, mental heath, and supportive services in Los Angeles, Sacramento, and Stanislaus counties. At the time, these programs were unique in California in their focus on homeless persons with serious mental illness, their mandate to provide immediate housing, and their flexibility of funding. On the basis of early success in these counties, the legislature passed AB2034 in 1999, which provided the resources to expand the program statewide. An understanding of the net service costs of these programs will provide valuable information on the allocation of fiscal resources associated with a major mental health policy experiment in California that could serve as a model for Medicaid programs throughout the country.
On November 2, 2004, California voters approved Proposition 63, which was signed into law as the Mental Health Services Act (MHSA). The MHSA applied a tax of 1% on incomes over $1 million to fund public mental health services. Twenty-eight percent of MHSA funding is allocated to full-service partnerships, housing-first programs that do whatever it takes to improve residential stability and mental health outcomes. Although the full-service partnership programs created by Proposition 63 have not yet been evaluated, useful information about their likely effects can already be gleaned by studying AB2034 programs, which served as the model for the full-service partnerships. Although reports have shown that these programs were successful in housing clients ( 2 ), we are not aware of any detailed evaluation of mental health services costs associated with AB2034.
In this study, we examined mental health service utilization and costs associated with the AB2034 program in San Diego County: Reaching Out and Engaging to Achieve Consumer Health (REACH). REACH was established in 2000 in response to concerns that homeless people with serious mental illness were being displaced by a new sports stadium in downtown San Diego ( 3 ). In response the San Diego County Adult and Older Adult Mental Health Services applied for and received from the state a $10.3 million competitive grant to implement integrated services for homeless clients with serious mental illness. REACH adopted a housing-first program that adopted a "whatever it takes" approach to engage and house clients by providing assertive outreach through a homeless outreach team, multiple housing options, assertive community treatment team-based case management, and outpatient services ( 3 ).
Clients for REACH are recruited from the shelters, a homeless outreach team, and community-based mental health programs. Housing for REACH clients is supported primarily by 100 Section 8 vouchers provided by the U.S. Department of Housing and Urban Development (HUD). Housing options include a residential treatment program ("Safe Haven") with 19 beds, a resident assistant, shared bathrooms, and a shared kitchen; single-room occupancy hotels in downtown San Diego, each with a sink, refrigerator, and small kitchen area and shared bathrooms on each floor; and scattered-site apartments. Although the process varies, clients are typically housed in Safe Haven for four to six months while they apply for Supplemental Security Income, Social Security Disability Income, or Department of Veterans Affairs (VA) benefits. Once they obtain financial support, clients obtain housing (rent ranges from $600 to $850 a month) by using a Section 8 voucher and contributing 30% to 40% of their income. In addition, the REACH program provides supplemental support of approximately $100 per month in food vouchers. Although REACH does not require sobriety for receipt of services, Safe Haven and many single-room occupancy hotels have strict limits on substance use. The only treatment requirement of clients is to meet with biweekly with a case manager ( 3 ).
Housing-first and related programs are expensive, which may result in a large amount of resources being allocated to relatively few clients ( 4 ). However, several studies in other settings have concluded that these programs are cost-effective, resulting from cost offsets from reductions in use of inpatient and emergency services, criminal justice system services, shelters, and other social services. In a study of the New York-New York housing-first initiative, Culhane and colleagues ( 5 ) found significant declines in shelter days, hospital days, and incarcerated days and increases in outpatient days among those receiving housing placement in comparison to a matched control group: the annualized cost reduction in service utilization was estimated to be $12,145 per participant. A similar study of a housing-first program in Denver, Colorado, found declines in inpatient admissions, emergency room visits, detoxification visits, and incarceration days and estimated a cost savings of $31,545 per participant ( 6 ). A large, randomized study of the HUD-VA supported-housing program found that the supported housing cost $45 more than standard care per additional day in supported housing ( 7 ). A randomized study of the housing-first, psychosocial rehabilitation program Pathways to Housing in New York found that the program increased consumer choice and days housed and reduced use of substance abuse services over a two-year period ( 2 ); this improvement was verified in a four-year follow-up study ( 8 ).
Lessons learned from these and other studies of housing programs for persons with chronic homelessness and serious mental illness suggest that housing-first programs and supported and supportive housing programs may improve housing, clinical, and psychosocial outcomes and that participants experience increases in outpatient care and cost offsets in inpatient and emergency services and criminal justice system services ( 9 , 10 , 11 , 12 , 13 , 14 ). However, the bulk of this research examined programs in New York City and within the VA. Because New York City allocates a relatively large amount of resources to its mental health programs and the Veterans Affairs system is the largest organized medical provider in the world, this research may not be generalizable to other programs. Less is known about the costs of the programs of more modest intensity implemented in 26 counties in California under AB34 and AB2034. These early programs were created to provide integrated housing, assertive community treatment team-based case management, mental health and recovery services, and supported employment services, and they served as the basis for a widespread implementation of full-service partnerships across the state of California.
In this study, we examined mental health service utilization and cost among REACH clients from up to two years before entry into the program and two years after entry. A comparison group was matched by propensity score in a quasi-experimental difference-in-difference design (that is, pre-post comparison with a contemporaneous control group). We hypothesized that there would be increases in outpatient service costs and declines in inpatient, emergency, and criminal justice systems service costs. The primary objective of this research was to estimate the magnitude of the cost offset related to this housing-first program.
Methods
Data, sample, and independent variables
Data from San Diego County's Adult and Older Adult Mental Health Services encounter-based management information system (MIS) were used to identify clients initiating the REACH program between July 1, 2002, and June 30, 2005. The MIS includes detailed information on demographic characteristics (that is, age, gender, race or ethnicity, and preferred language for services), clinical diagnosis, and Global Assessment of Functioning (GAF) score. For each REACH client, we collected information on demographic characteristics, axis I primary clinical diagnosis, GAF score, and initial date of service.
Using propensity score matching, we identified a comparison group ( 15 , 16 ). The propensity score approach is a useful method for constructing comparison groups that are balanced with respect to observable characteristics. In our application, propensity scores allowed us to identify a comparison group of homeless clients with serious mental illness who had demographic and clinical characteristics similar to those of REACH clients and were initiating services at the same time as REACH clients. This control group allowed us to account for service utilization changes when a homeless client initiates service (typically, utilization will increase), and it allowed us to control for contemporaneous, systemwide time trends in utilization (for example, utilization that might result from the opening or closing of programs). Propensity score matching helps to ensure that the control group is similar in observable demographic and clinical characteristics to the group of REACH clients.
In the MIS, living situation is recorded at the initiation of each episode—for example, when beginning to receive services at an outpatient clinic or upon admission to an inpatient or emergency psychiatric unit. We obtained data on all initial episodes in case management or outpatient programs in which the individual was homeless, including data on client demographic characteristics, diagnosis, and date of service. We estimated a propensity score of REACH participation that was based on age, gender, race or ethnicity, preferred language for services, clinical diagnosis, GAF score, and fiscal year of initiation of service by using a logistic regression model. We found no significant effects for interactions between the predictor variables. Goodness of fit was assessed with a modified Hosmer-Lemeshow test as well as by Pregibon's link test.
The resulting propensity scores were used to identify a comparison group by using nearest-neighbor matching ( 17 ). Nearest neighbors were determined by first sorting all episodes by the estimated propensity score and then by searching forward and backward for the closest episodes for potential clients for the control group; if the forward and backward matches were equally close, the forward or backward match was chosen at random. We retained multiple client episodes if they were identified within the same (backward or forward) match.
The MIS also includes detailed information on service utilization, including date of service, the program where the service was provided, procedure codes, and service minutes. The MIS system is similar to a claims-based system except that it does not contain the amounts paid for services. Costs for each service were determined from detailed analysis of these encounter data combined with information from program-specific cost reports. We used cost reports to allocate the total costs of an entire program (including staff, supplies, administration, overhead, and capital costs) to each type of service provided. For outpatient programs, costs are allocated to service minutes for assessments, case management, crisis intervention, medication management, rehabilitation and recovery services, and individual, group, and family therapy. Costs for emergency services are allocated to hours of crisis stabilization. Costs for inpatient services are allocated to a 24-hour day. Service costs were calculated by multiplying the units of each service by the cost per unit for that service.
For clients in the REACH group and the control group, we calculated mental health services costs for case management, outpatient, inpatient plus emergency, and criminal justice system services. Inpatient and emergency services included hospitalizations, stays at crisis residential facilities, emergency psychiatric unit services, and psychiatric emergency response team services. Criminal justice system services included mental health services provided in the county jail. Cost data were aggregated over two years before and two years after initiation of service: for REACH clients, this date was initiation of REACH services; for the comparison group, this date was the initiation of the episode matched by propensity score. As discussed above, we limited the sample to clients initiating a case management or outpatient service between July 1, 2002, and June 30, 2005. Utilization and cost data were available from July 1, 2001, to June 30, 2006. Thus clients had a minimum of one year of exposure to services in each of the pre- and postintervention periods. We capped exposure at two years. We accounted for varying lengths of exposure (exposures between one and two years) by including an exposure offset in our regression models. The University of California, San Diego, Institutional Review Board and the San Diego County Mental Health Services Research Committee approved the use of these data for the purpose of this study in accordance with the Privacy Rule of the Health Insurance Portability and Accountability Act of 1996.
Statistical analysis
We analyzed mental health services costs using four two-part models embedded in a quasi-experimental, difference-in-difference design ( 18 ). The difference-in-difference design is essentially a pre-post comparison with a contemporaneous control group. The use of propensity matching assures the comparability of the two groups. A difference-in-difference design allowed us to account for contemporaneous trends in availability of mental health services that were not associated with the REACH program. Although our control group was matched by propensity score, it is not essential that the comparison group look identical in the preintervention period. It is only important that the time trends be comparable.
The two-part model is commonly used to estimate health care costs when the dependent variable is nonnegative and when its distribution is noticeably skewed and kurtotic (with a heavy right-hand tail) ( 19 ). We used four two-part models to separately analyze costs for each category of service. Logistic regression was used to estimate the probability of use, and a generalized linear regression (specified as having a gamma distribution with a log link function) was used to estimate costs conditional on receiving at least one service among clients in the REACH group and those in the control group ( 20 , 21 ). An indicator variable was included for clients participating in REACH; this indicator variable was set equal to one for REACH participants in both the pre- and postintervention periods. A second indicator variable was included for the postintervention period; this variable was set equal to one for all clients in the postintervention period. A third indicator variable was included for the interaction between participation in REACH and the postintervention period. Age, gender, race or ethnicity, preferred language for services, clinical diagnosis, and GAF score were included as additional control covariates. We adjusted for time at risk by including the length of time that clients were exposed to the intervention as an exposure parameter ( 22 ).
Incremental effects associated with REACH were calculated over both parts of the model and were standardized to the underlying population characteristics. For example, the total incremental cost of REACH was calculated as the average difference in total cost across clients as they were alternatively assigned to REACH and to the control group. We computed three sets of estimates from these regressions: pre- and postintervention estimates for clients in the REACH group, pre- and postintervention estimates for clients in the control group, and the difference between these estimates (difference-in-difference estimate). Total costs were calculated as the sum of the predicted costs in each model. Standard errors were calculated with the nonparametric bootstrap, and p values were computed with the percentile method from the empirical distributions of the results from 1,000 replicates ( 23 ).
Results
Summary characteristics for clients in the REACH group (N=177) and those in the matched control group (N=161) are shown in Table 1 . Matching on the propensity score reduced the potential control group from 1,151 to 161 clients. Propensity score matching improved the covariate balance primarily on diagnosis. The absolute standardized differences in rates of diagnosis were reduced for the most part; they decreased from 50 to 2 for schizophrenia, increased from 7 to 11 for bipolar disorder, and decreased from 16 to 4 for major depression, from 22 to 1 for other psychotic disorder, and from 44 to 6 for other disorder.
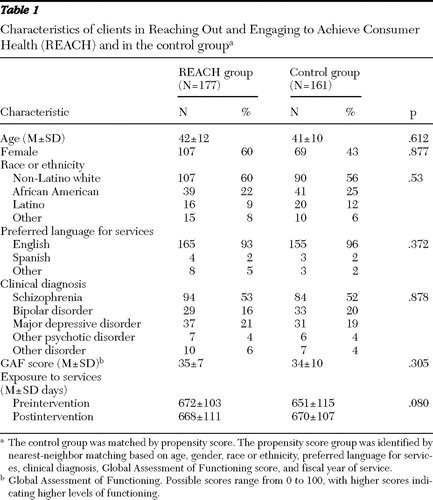 |
There were no significant differences in demographic characteristics or clinical diagnosis between the REACH and control groups. Overall, the mean±SD age was 42±11. A total of 176 (52%) were female, 197 (58%) were non-Latino white, 80 (24%) were African American, 36 (11%) were Latino, and 25 (7%) were "other" race or ethnicity. A total of 178 (53%) had an axis I primary diagnosis of schizophrenia, 62 (18%) had bipolar disorder, 68 (20%) had major depressive disorder, 13 (4%) had "other" psychotic disorder, and 17 (5%) had another disorder.
Table 2 presents standardized mental health services costs for the two years before and two years after entry into the REACH program. Costs increased substantially for case management and outpatient services (differences of $7,011 and $3,513, respectively) (p<.001 each). Costs for inpatient and emergency services and criminal justice system services declined by $5,043 (p=.008) and $573 (p=.002), respectively. Total costs increased by $4,907 (p=.044).
 |
Table 3 presents standardized mental health services costs for the two years before and two years after initiation of service for the control group. Costs increased by $608 for case management (p=.004) and by $2,826 for outpatient services (p<.001). There were no significant changes in inpatient and emergency services, criminal justice system services, or total costs. There were also no significant differences in costs during the time before REACH initiation, both overall and by subcategory, between clients in the REACH group and those in the comparison group.
 |
Difference-in-difference estimates (post-pre) are presented in Table 4 (difference estimates for REACH and control clients are presented again for reference). Difference-in-difference estimates yield the standardized marginal effects for participation in the REACH program: case management costs increased by $6,403 (p<.001), inpatient and emergency costs declined by $6,103 (p=.034), and criminal justice system costs declined by $570 (p=.020). There were no significant differences in outpatient or total costs. Notably, the net cost of services, $417 over two years, was substantially lower than the total cost of services ($20,241) ( Table 2 ).
 |
Discussion
In this study, we examined the net mental health services costs of San Diego County's AB2034 program and found that the increased costs of case management and outpatient services were essentially entirely offset by reduced expenditures on inpatient and emergency services and mental health services provided in criminal justice system settings.
We selected a propensity-score-matched control group of homeless clients with severe mental illness who had a similar demographic and clinical profile and initiated case management or outpatient services at the same time as REACH clients. Our sample was relatively small for both propensity score adjustment and for health care cost econometric analysis. As a result, small imbalances remain in the covariates, and our estimate of total net costs is somewhat less precise. In addition, our use of propensity score matching and multivariate regression adjusted for observed, but not unobserved, covariates. Thus clients in our control group may have differed from those in the REACH group on unmeasured characteristics. For example, clients in the control group may have less insight or may be otherwise less inclined to engage in assertive community treatment team-based care. Although these differences would have implications for a full implementation targeting all homeless clients, the current implementation of housing-first programs is relatively modest, and an expanded program would be able to fill its caseload relatively quickly. Indeed, the full-service partnership programs in San Diego County reached capacity in their first year of operation.
Our analysis did not include either county or federal costs of housing, income, and supplemental support, and it did not include other social costs, such as any incarceration costs beyond mental health services provided in jail or costs of crime that may have been reduced. However, by limiting the scope of the analysis to mental health services costs, we were able to provide a very detailed analysis of the majority of program resources. We were unable to measure reductions in illness severity or improvements in client satisfaction, functioning, or quality of life. Our analysis suggests that the REACH program more actively managed clients and that by providing more intensive services in an outpatient setting, the program reduced the likelihood that clients would decompensate and be admitted to an inpatient or emergency facility or receive services in jails.
Conclusions
The finding of a substantial cost offset in the AB2034 program is both important and timely. These programs served as the model for the full-service partnerships, which became the cornerstone of the largest mental health policy intervention in recent times, California's Mental Health Services Act. Some concerns have been raised about the costs of the program and the focus of a large amount of resources on a relatively small population. Our analysis suggests that these programs will offset a significant proportion of their costs, thus making available additional resources to those not receiving services from full-service partnerships.
Acknowledgments and disclosures
Financial support was provided by grant P30-MH066248 from the National Institute of Mental Health. The authors acknowledge the San Diego County Health and Human Services Agency Adult and Older Adult Mental Health Services for access to the management information systems.
The authors report no competing interests.
1. Tsemberis S, Gulcur L, Nakae M: Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. American Journal of Public Health 94:651–656, 2004Google Scholar
2. Burt M, Anderson J: AB2034 program experiences in housing homeless people with serious mental illness, in CSH Evidence Series. Washington, DC, Corporation for Supportive Housing, 2005Google Scholar
3. Pearson C, Locke G, Montgomery A, et al: The Applicability of Housing First Models to Homeless Persons With Serious Mental Illness. Washington, DC, US Department of Housing and Urban Development, Office of Policy Development and Research, 2007Google Scholar
4. Rosenheck R: Cost-effectiveness of services for mentally ill homeless people: the application of research to policy and practice. American Journal of Psychiatry 157:1563–1570, 2000Google Scholar
5. Culhane D, Metraux S, Hadley T: The Impact of Supportive Housing for Homeless People With Severe Mental Illness on the Utilization of the Public Health, Corrections, and Emergency Shelter Systems: The New York-New York Initiative. Washington, DC, Fannie Mae Foundation, 2001Google Scholar
6. Perlman J, Parvensky J: Denver Housing First Collaborative Cost Benefit and Program Outcomes Report. Denver, Colorado Coalition for the Homeless, 2006Google Scholar
7. Rosenheck R, Kasprow W, Frisman L, et al: Cost-effectiveness of supported housing for homeless persons with mental illness. Archives of General Psychiatry 60:940–951, 2003Google Scholar
8. Stefancic A, Tsemberis S: Housing first for long-term shelter dwellers with psychiatric disabilities in a suburban county: a four-year study of housing access and retention. Journal of Primary Prevention 28:265–279, 2007Google Scholar
9. Cheng AL, Lin H, Kasprow W, et al: Impact of supported housing on clinical outcomes: analysis of a randomized trial using multiple imputation technique. Journal of Nervous and Mental Disease 195:83–88, 2007Google Scholar
10. Conrad KJ, Hultman CI, Pope AR, et al: Case managed residential care for homeless addicted veterans: results of a true experiment. Medical Care 36:40–53, 1998Google Scholar
11. Goldfinger SM, Schutt RK, Tolomiczenko GS, et al: Housing placement and subsequent days homeless among formerly homeless adults with mental illness. Psychiatric Services 50:674–679, 1999Google Scholar
12. Hurlburt MS, Hough RL, Wood PA: Effects of substance abuse on housing stability of homeless mentally Ill persons in supported housing. Psychiatric Services 47:731–736, 1996Google Scholar
13. Kasprow WJ, Rosenheck RA, Frisman L, et al: Referral and housing processes in a long-term supported housing program for homeless veterans. Psychiatric Services 51:1017–1023, 2000Google Scholar
14. Rosenheck R, Frisman L, Gallup P: Effectiveness and cost of specific treatment elements in a program for homeless mentally ill veterans. Psychiatric Services 46:1131–1139, 1995Google Scholar
15. Rosenbaum P, Rubin D: The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55, 1983Google Scholar
16. Rubin DB: Estimating causal effects from large data sets using propensity scores. Annals of Internal Medicine 127:757–763, 1997Google Scholar
17. Rubin DB, Thomas N: Matching using estimated propensity scores: relating theory to practice. Biometrics 52:249–264, 1996Google Scholar
18. Goldman HH, Frank RG, Burnam MA, et al: Behavioral health insurance parity for federal employees. New England Journal of Medicine 354:1378–1386, 2006Google Scholar
19. Manning WG, Newhouse JP, Duan N, et al: Health insurance and the demand for medical care: evidence from a randomized experiment. American Economic Review 77:251–277, 1987Google Scholar
20. Blough DK, Madden CW, Hornbrook MC: Modeling risk using generalized linear models. Journal of Health Economics 18:153–171, 1999Google Scholar
21. Manning WG, Mullahy J: Estimating log models: to transform or not to transform? Journal of Health Economics 20:461–494, 2001Google Scholar
22. Johnson N, Kotz S, Balakrishnan N: Continuous Univariate Distributions, 2nd ed: Wiley Series in Probability and Statistics, Vol 1. New York, Wiley, 1994Google Scholar
23. Efron B: An Introduction to the Bootstrap. New York, Chapman and Hall, 1993Google Scholar



