Changing Perceptions of Depression: Ten-Year Trends From the General Social Survey
Depression is among the most common mental illnesses and a leading cause of disability ( 1 ). According to a recent national study, the lifetime prevalence of major depression among adults is 16.2% and the 12-month prevalence is 6.6% ( 2 ). Depression accounts for an estimated $83.1 billion in medical care and workplace costs ( 3 ).
Over the past decade there have been numerous efforts across the public and private sectors to increase knowledge and awareness of depression. Multimedia public service campaigns, such as Depression Is Real ( www.depressionisreal.org ), CBS Cares ( www.cbs.com/cbs_cares/topics/?sec=5 ), and Real Men Real Depression ( www.nimh.nih.gov/health/publications/real-men-real-depression.shtml ), focused on recognition and treatment of depression. The 1990s saw the initiation of National Depression Screening Day ( 4 ) and were declared "The Decade of the Brain" by former President George H. W. Bush in order to "enhance public awareness of the benefits to be derived from brain research" ( www.loc.gov/loc/brain ). These campaigns emphasize depression as a chronic medical illness, implying that treatment should be sought from a medical doctor ( 5 ). The past decade has also seen an increased focus on direct-to-consumer advertising by pharmaceutical companies, with a more than threefold increase in spending in that period ( 6 ). The increase in advertising of antidepressant medications has been associated with greater use of these medications ( 7 ).
While rates of mental illness have remained stable in the past decade, rates of treatment have risen significantly ( 8 ). Treatment rates from the National Comorbidity Survey (NCS) showed an increase in the treatment of persons with a 12-month history of depression, from 30% in 1990 ( 9 ) to 52% in 2003 ( 2 ). Prescriptions for antidepressants have tripled in the past decade, with recent data suggesting that 7% of Americans have used an antidepressant in the past month ( 10 ). Intercontinental Marketing Services found antidepressants were the most common class of medications prescribed in the United States in 2007 ( 11 ). Relative use of psychotherapy for depression has declined, from 71% to 60% between 1987 and 1997 ( 12 ). The general medical setting has now become the most common place for mental health treatment overall, with a growth of 153% between 1990 and 2000 ( 13 ). A comparison of treatment rates between 1990 and 2003 from the NCS found significant differences among treatment rates for all mental disorders when stratified by age, race, sex, education, and marital status ( 8 ).
Stigma against people with mental illness has long been recognized. Conceptualizations of stigma include factors at both the society and individual levels. Negative social consequences, such as loss of status and opportunities for the individual, as well as discriminatory public policies can result from identification with a stigmatized group. Strong emotional responses on the part of the person being stigmatized, such as shame and fear, and by the stigmatizer, such as anger or pity, are also potentially harmful to those labeled as mentally ill ( 14 ). Negative qualities of incompetence, dangerousness, and blame are often attributed to persons with mental illness ( 15 ). Data from the 1996 General Social Survey (GSS) showed that Americans are likely to view persons with mental illnesses as more dangerous and less socially desirable than those without a mental illness ( 16 ) and that there are substantial differences in how people think about depression among children versus adults ( 17 ). Attitudes about depression influence acceptance of its diagnosis ( 18 ) and treatment ( 19 ), and beliefs about the causes of depression influence understanding of the utility of treatments ( 20 , 21 ). Analysis of the 1996 GSS mental health module also showed that there was a correlation between attributing depression to biological causes, such as brain chemistry and genetics, and recommending treatment in a medical setting ( 22 ). An understanding of how the American public thinks about depression is crucial to reducing stigma and increasing rates of appropriate treatment.
In this study, using data from the GSS, a nationally representative survey of attitudes about depression and its treatment, we investigated whether there has been a change in beliefs among Americans about depression and whether these beliefs differ by sociodemographic characteristics. The GSS is the largest sample of the changing cultural perceptions about depression and its treatment in the United States.
Methods
The data in this study are from the 1996 and 2006 mental health topical modules of the GSS. The GSS is conducted by in-person interviews with a full-probability sample of adults living in households in the United States. It is administered biannually. In 1996 the GSS had a response rate of 76% (N=1,444) and in 2006 a response rate of 71% (N=1,523). Detailed descriptions of the GSS and the mental health module methodology have been reported elsewhere ( 23 ). The data are publicly available without identifiers, and this study was granted exemption status by the institutional review board of the University of Pennsylvania.
In the GSS mental health module, each respondent was asked questions regarding a vignette that described an individual with symptoms consistent with DSM-IV criteria ( 24 ) for a particular condition. We examined data from respondents who were given the vignette describing major depression in 1996 (300 respondents) and in 2006 (397 respondents). A transcript of the vignette has been published elsewhere ( 16 ).
Causal beliefs
Respondents were asked questions about potential causes of the vignette character's problem. Responses that the problems were "likely" or "somewhat likely" to be caused by "a chemical imbalance in the brain" or "a genetic or inherited problem" were considered as endorsing a biological cause of depression. These causes appeared to match most closely those endorsed by the current medical model. The variable for nonbiological causes of the character's depression included endorsements of "the way he was raised," "the person's own bad character," and "God's will." These causal categories were not mutually exclusive. We also examined the response for "stressful circumstances" as a cause of depression.
Treatment options
Respondents were asked what the vignette character should do and were given a list of options to endorse. Then they were asked to prioritize all the options they selected. We categorized their first-ranked responses as either biological or nonbiological. The biological variable consisted of seeking help from a general doctor, seeking help from a psychiatrist, or taking prescription medications—all options involving medical treatment. Nonbiological treatment included talking to a therapist or counselor, joining a self-help group, or talking to a clergy member or other religious leader—all options that have a talk-centered emphasis. Discussing the problem with friends or family was commonly ranked as the first treatment choice. Because this response does not represent clear treatment and may precede treatment from either a biological or nonbiological route, we categorized for analysis the second-choice treatment option for those who responded this way. The categories of biological and nonbiological treatments were mutually exclusive. We also present data individually for each treatment option, including discussing the problem with friends or family.
Demographic characteristics
Age was measured in years and divided into three categories, 18–34 years, 35–54 years, and 55 years or greater. Race, determined by self-report, was categorized into white and nonwhite groupings. Education level was grouped into three categories; less than, equal to, or greater than completion of high school. We used self-report of social class as an indicator of socioeconomic status and created two categories, working class or poor, and middle or upper class. The GSS classified the population density of each respondent's neighborhood in keeping with U.S. Census convention, and we divided these categories into urban, suburban, and rural settings.
Statistics
We compared the demographic characteristics of the study population to determine whether they differed by year. We then compared rates of endorsement of biological and nonbiological causes and treatments by year overall, as well as for each specific sub-item, and created the unadjusted risk ratio (RR) to show the change in the proportion of responses from 1996 to 2006, which was tested by chi square analysis to determine statistical significance. Next we examined stratified rates of endorsement of biological causes, nonbiological causes, and biological treatments and examined changes over time for each stratum. Each proportion reported was weighted to account for sampling design. We also used a log-linear model to examine whether the relative risks for certain demographic variables differed across strata. This model included main effects for year, the demographic variables, and their interaction. Statistical significance of the interaction term was indicative of a difference across strata. All analyses were conduced with SAS version 9.1.3 ( 25 ) and SUDAAN version 9.0 (26) to account for the complex sample design variables and the sampling weights.
Results
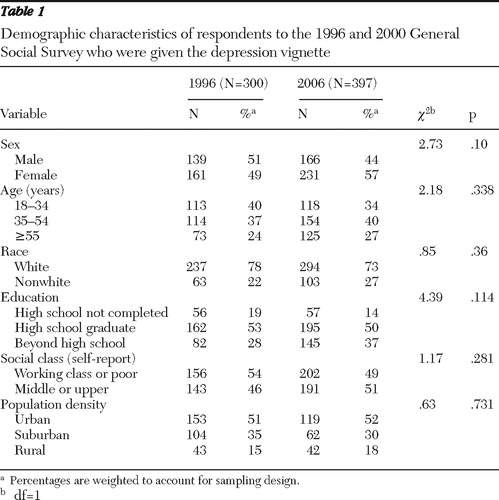
There was an increase in the proportion of respondents who identified the person in the vignette as having a mental illness, from 68% of respondents in 1996 to 75% in 2006, but this trend did not reach statistical significance. When respondents were subsequently asked if they thought the person described was likely to have depression, most people agreed with that description in both years (94% in 1996 and 95% in 2006; data not shown). Table 1 indicates that the sample populations in 1996 and 2006 were statistically equivalent in their demographic characteristics.
 |
Distribution of causal beliefs
Table 2 presents the distribution of perceived causes of depression in 1996 and 2006. Biological etiologies were more highly endorsed in 2006, with 88% of respondents rating at least one of these causes as likely, compared with 77% of respondents in 1996 (RR=1.14, p<.01). A chemical imbalance in the brain and a genetic or inherited problem remained the first and second most commonly endorsed causes of depression, respectively. There was a modest decrease in the endorsement of nonbiological causes of depression, but this difference did not reach statistical significance. In both study years, life stresses were endorsed by about 95% of all respondents as a cause of depression.
 |
Distribution of treatment beliefs
Table 2 also illustrates that in 2006, 60% of respondents believed that biological treatment for depression was an appropriate first choice, compared with 48% in 1996 (RR=1.29, p<.05). When the treatment recommendations were examined individually, we found a significant increase in the proportion of respondents who recommended seeking treatment from both general medical doctors and psychiatrists. There was a trend toward greater recommendation of prescription medications. Talking to friends or family remained the most commonly endorsed treatment option in both years. Also notable was a large increase in the proportion of respondents who endorsed seeking help for depression from a spiritual healer, from 22% in 1996 to 42% in 2006 (RR=1.92, p<.001). Only one respondent in 1996, and none in 2006, felt that no treatment was appropriate for the person described in the vignette.
Sociodemographic variables
There was an increase in attribution of depression to biological causes among male respondents, with 71% endorsing these causes in 1996 versus 87% in 2006 (RR=1.22, p<.01) ( Table 3 ; a more detailed version of this table, showing specific sample sizes, is available as an online supplement to this article at ps.psychiatryonline.org ). Among female respondents there was a significant decrease in endorsing nonbiological causes, from 64% to 52% (RR=.80, p<.05), but there was no real change among men in supporting nonbiological causes of depression.
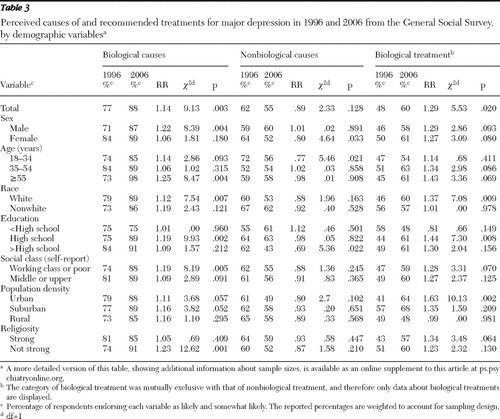 |
White respondents showed an increase in attributing depression to biological causes, from 79% in 1996 to 89% in 2006 (RR=1.12, p<.05), and an increase in support of biological treatment, from 46% in 1996 to 60% in 2006 (RR=1.37, p<.05). There was no significant change in attitudes about the causes or treatment of depression among nonwhite respondents.
Among the oldest age group there was an increase in support of biological causes of depression, from 73% in 1996 to 98% in 2006 (RR=1.25, p<.01), a trend that was not statistically significant in the younger age groups. Only the youngest age group showed a significant decrease in support of nonbiological causes of depression, from 72% to 56% (RR=.77, p<.05).
The distribution of causal attribution varied by education level. Among those with a high school education there was a marked increase in endorsement of biological causes (75% versus 89%; RR=1.19, p<.01), whereas there was no significant change in the other education strata. Those with more than a high school education were less likely to endorse nonbiological causes in 2006 compared with 1996 (43% versus 62%; RR=.69, p<.05), whereas the other two education categories showed minimal change in this variable. Those with a high school education showed a greater support of biological treatment options. Nonsignificant patterns were seen in the other education groups.
Greater support of biological causes and treatments held across socioeconomic classes and population density, although this finding was statistically significant among only those who identified as poor or working class and those living in urban areas. There was a strongly significant difference in attribution of biological causes among those who said that they were not strongly religious (74% to 91%; RR=1.23, p<.01) but there was no significant change in any of the outcome variables for those reporting strong religious beliefs.
In the series of log-linear models there were no statistically significant differences across any of the examined strata (data not shown).
Discussion
We found substantial changes in the American public's beliefs about depression, with an increasing endorsement of biological causes and treatments over a ten-year period. Although it is unknown what led to the changes in attitudes that we observed, there are a number of potential influences. In the past decade there have been many widespread multimedia public awareness campaigns about depression and other mental illnesses, both publicly and privately funded. To our knowledge there have not been detailed studies in the United States to examine direct links between public campaigns and changes in attitudes. However, studies from other developed countries, including Australia ( 27 ) and England ( 28 ), have shown an increase in awareness and recognition of depression as well as a shift in beliefs about treatments after similar public-awareness campaigns.
Concurrent with our observations of public perceptions about depression, there has also been rapid growth in direct-to-consumer advertising of antidepressant medications that may contribute to an increasingly medicalized perspective. Although our data showed only a modest increase in the proportion of respondents who supported prescription medication as a treatment for depression, there was a substantial increase in those suggesting seeking treatment from physicians, either general practitioners or psychiatrists. It is likely that such sources of treatment would include discussion or recommendation of prescription medication. Although these advertisements are intended to increase sales of a specific medication, they appear to be framed, and may serve as, industry-sponsored public service announcements, with a description of the symptoms of depression and a message that depression is a medical illness best treated by a physician, presumably in part with medications. Furthermore, advertisements for antidepressant medications often instruct viewers to discuss the matter with their physician, which corresponds to the large increase we found in recommending treatment from a primary care doctor. Although the increase in support of medication as a treatment was modest, recommending treatment by a physician may implicitly endorse treatment with medication.
The changing attitudes about depression that we observed mirror national changes in the treatment of depression, which show that the role of primary care physicians in treating depression has grown along with the use of antidepressant medications ( 13 ). The use of psychotherapy among those receiving treatment for depression has shown a relative decline ( 12 ), which parallels the attitudes of our study populations in which few survey respondents recommended talk therapy or counseling as a first-line treatment for depression. This trend does not reflect current research on depression that demonstrates that psychotherapy is effective in treating depression ( 29 ), nor does it reflect treatment guidelines that list psychotherapy among first-line treatments for mild and moderate depression ( 30 ).
Most respondents considered the support of family and friends as a first-line treatment for depression, a finding consistent with studies in other developed countries about lay beliefs ( 31 ). Although this could be viewed simply as a type of self-help strategy ( 32 ), it may indicate an essential element of help-seeking behavior and an important gateway to mental health care. The reliance of Americans on close social networks further underscores the importance of understanding public beliefs about mental illness. It is from friends and family that information, support, and society's expectations are communicated. These forces are likely to guide recommendations to family members or friends who are in mental distress ( 17 , 33 ).
It is also important to note that we found no significant decline in endorsement of nonbiological causes of depression in the sample as a whole. A large proportion of the U.S. population—about a third of the respondents in this study—believes that depression is likely caused by bad character, despite also believing perhaps that it is a brain disorder. This belief that a deficient character may lead to mental illness illustrates that stigma about depression remains. This type of belief places blame for the illness on the person with depression, a stigmatizing attitude that may undermine progress toward acceptance of those with mental illness.
Studies in other developed countries have looked at similar issues. A study in Germany compared attitudes about treatment for major depression and schizophrenia. It found that for both illnesses there was a significant increase in the proportion of respondents who recommended seeking help from a psychotherapist or psychiatrist. This study found a decline in the proportion of those suggesting seeking help for these illnesses from a general practitioner ( 34 ). A study in Australia found that between 1998 and 2004, respondents were more likely to suggest that a person with depression seek help from a general practitioner and a counselor, but there was no meaningful change in the proportion of respondents suggesting that a person with depression seek help from a psychiatrist or psychologist or take medications ( 33 ). Another Australian study found that respondents in 2003–2004, compared with respondents in 1995, were more likely to attribute depression to a genetic cause, the death of someone close, and problems from childhood ( 35 ).
There are two main limitations of our analysis. First, because of the ecological design of the GSS, we were unable to make any causal inferences between changing beliefs about the causes of depression and recommendations for treatment; we could observe only associations. Longitudinal cohort studies would be needed to make a causal link and track these trends over time. Second, although the GSS is the largest nationally representative survey to examine these issues and has a rigorous sampling technique, we examined data from only the subset of the study population that was asked about the vignette describing depression, thus limiting our sample size. Some of the trends we observed, particularly among specific demographic groups, might have been more pronounced with a larger sample.
Depression remains underrecognized and undertreated. There is much left to learn about how attitudes might translate into action when someone is faced with his or her own symptoms of depression or with symptoms of someone close. Although many effective treatments are available, too many people suffer from depression without seeking or accepting treatment. Further study about how attitudes differ between sociodemographic groups may provide an avenue to reducing disparities in treatment rates.
Conclusions
There have been changes in attitudes about the causes and treatments of depression among the American public in the past decade, with a shift toward a biological framework. Despite these changes, negative attitudes about persons with depression are prevalent. A greater understanding of beliefs about depression may lead to more effective outreach and education efforts.
Acknowledgments and disclosures
Dr. Marcus has received grants from Ortho-McNeil Janssen and has been a consultant to Eli Lilly and Company, Bristol-Myers Squibb, AstraZeneca, and Pfizer. The other author reports no competing interests.
1. Vital and Health Statistics. Series 13, no 159. Atlanta, Ga, Centers for Disease Control and Prevention, National Center for Health Statistics, Feb 2006. Available at www.cdc.gov/nchs Google Scholar
2. Kessler RC, Berglund P, Demler O, et al: The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 289:3095–3105, 2003Google Scholar
3. Greenberg PE, Kessler RC, Girnbaum HG, et al: The economic burden of depression in the United States: how did it change between 1990 and 2000? Journal of Clinical Psychiatry 64:1465–1475, 2003Google Scholar
4. Jacobs DG: National Depression Screening Day: educating the public, reaching those in need of treatment, and broadening professional understanding. Harvard Review of Psychiatry 3:156–159, 1995Google Scholar
5. Lacasse JR: Consumer advertising of psychiatric medications biases the public against nonpharmacologic treatment. Ethical Human Psychology and Psychiatry 7:175–179, 2005Google Scholar
6. Donohue JM, Cevasco M, Rosenthal MB: A decade of direct-to-consumer advertising of prescription drugs. New England Journal of Medicine 357:673–681, 2007Google Scholar
7. Donohue JM, Berndt ER, Rosenthal M, et al: Effects of pharmaceutical promotion on adherence to treatment guidelines for depression. Medical Care 42:1176–1185, 2004Google Scholar
8. Kessler RC, Demler O, Frank RG, et al: Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine 352:2515–2523, 2005Google Scholar
9. Katz SJ, Kessler RC, Lin E, et al: Medication management of depression in the United States and Ontario. Journal of General Internal Medicine 13:77–85, 1998Google Scholar
10. Health, United States, 2004. Atlanta, Ga, Centers for Disease Control and Prevention, National Center for Health Statistics, Sept 2004. Available at www.cdc.gov/nchs Google Scholar
11. 2007 Top Therapeutic Classes by US Dispensed Prescriptions. Norwalk, Conn, IMS Health, 2007. Available at www.imshealth.com Google Scholar
12. Olfson M, Marcus SC, Druss B, et al: National trends in the outpatient treatment of depression. JAMA 287:203–209, 2002Google Scholar
13. Wang PS, Demler O, Olfson M, et al: Changing profiles of service sectors used for mental health care in the United States. American Journal of Psychiatry 163:1187–1198, 2006Google Scholar
14. Link BG, Lang LH, Phelan JC, et al: Measuring mental illness stigma. Schizophrenia Bulletin 30:511–541, 2004Google Scholar
15. Corrigan P: How stigma interferes with mental health care. American Psychologist 59:614–625, 2004Google Scholar
16. Link BG, Phelan JC, Bresnahan M, et al: Public conceptions of mental illness: labels, causes, dangerousness and social distance. American Journal of Public Health 89:1328–1333, 1999Google Scholar
17. Perry BL, Pescosolido BA, Martin JK, et al: Comparison of public attributions, attitudes, and stigma in regard to depression among children and adults. Psychiatric Services 58:632–635, 2007Google Scholar
18. VanVoorhees BW, Fogel J, Houston TK, et al: Beliefs and attitudes associated with the intention to not accept the diagnosis of depression among young adults. Annals of Family Medicine 3:38–45, 2005Google Scholar
19. Croghan TW, Tomlin M, Pescosolido BA, et al: American attitudes toward and willingness to use psychiatric medications. Journal of Nervous and Mental Disease 191:166–174, 2003Google Scholar
20. Iselin MG, Addis ME: Effects of etiology on perceived helpfulness of treatments for depression. Cognitive Therapy and Research 27:205–222, 2003Google Scholar
21. Angermeyer MC, Matschinger H, Riedel-Heller SG: Whom to ask for help in case of a mental disorder? Preferences of the lay public. Social Psychiatry and Psychiatric Epidemiology 34:202–210, 1999Google Scholar
22. Kuppin S, Carpiano RS: Public conceptions of serious mental illness and substance abuse, their causes and treatments: findings from the 1996 General Social Survey. American Journal of Public Health 96:1766–1771, 2006Google Scholar
23. Pescosolido BA, Martin JK, Link BG, et al: Americans' Views of Mental Health and Illness at Century's End: Continuity and Change. Public report on the MacArthur mental health module, 1996 General Social Survey. Bloomington, Indiana Consortium for Mental Health Services Research and Joseph P Mailman School of Public Health, Columbia University, 2000Google Scholar
24. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
25. SAS, version 9.1.3. Cary NC, SAS Institute, 2005Google Scholar
26. SUDAAN, version 9.0. Research Triangle Park, NC, RTI International, 2004Google Scholar
27. Jorm AF, Christensen H, Griffiths KM: The impact of Beyond Blue: the national depression initiative on the Australian public's recognitions of depression and beliefs about treatment. Australian and New Zealand Journal of Psychiatry 39:248–254, 2005Google Scholar
28. Paykel ES, Hart D, Priest RG: Changes in public attitudes to depression during the Defeat Depression Campaign. British Journal of Psychiatry 173:519–522, 1998Google Scholar
29. DeRubeis RJ, Hollon SD, Amsterdam JD, et al: Cognitive therapy vs medications in the treatment of moderate to severe depression. Archives of General Psychiatry 62:409–416, 2005Google Scholar
30. American Psychiatric Association: Practice guideline for the treatment of patients with major depressive disorder (revision). American Journal of Psychiatry 157(Apr suppl):1–45, 2000Google Scholar
31. Angermeyer MC, Matschinger H, Riedel-Heller SG: What to do about mental disorder: help-seeking recommendations of the lay public. Acta Psychiatrica Scandinavica 103:220–225, 2001Google Scholar
32. Jorm AF: Mental health literacy: public knowledge and beliefs about mental disorders. British Journal of Psychiatry 177:396–401, 2000Google Scholar
33. Goldney RD, Fisher RJ, Grande ED, et al: Changes in mental health literacy about depression: South Australia, 1998 to 2004. Medical Journal of Australia 183:134–137, 2005Google Scholar
34. Angermeyer MC, Matschinger H: Have there been any changes in the public's attitudes towards psychiatric treatment? Results from representative population surveys in Germany in the years 1990 and 2001. Acta Psychiatrica Scandinavica 111:68–73, 2005Google Scholar
35. Jorm AF, Christensen H, Griffiths KM: Public beliefs and causes and risk factors for mental disorders: changes in Australia over 8 years. Social Psychiatry and Psychiatric Epidemiology 40:764–767, 2005Google Scholar



