Correlates of Adverse Childhood Experiences Among Adults With Severe Mood Disorders
Children and adolescents have a high level of exposure to traumatic events, such as the unexpected loss of a loved one and physical or sexual abuse, and to other adverse experiences, such as parental divorce, parental mental illness, or being placed in foster care ( 1 , 2 ). For example, the National Comorbidity Survey found that 50% of respondents in the general population reported experiencing two or more such adverse events in childhood ( 1 ). Similarly, the Adverse Childhood Experiences study, which was conducted in a primary care setting, found that more than 50% of respondents had experienced at least one type of adverse childhood experience in childhood, and 25% reported more than two types ( 3 ).
Results from these studies also suggest that adverse childhood experiences, such as abuse, domestic violence, and other forms of household dysfunction, frequently co-occur ( 2 , 3 ). For example, 80% of individuals who were sexually abused in childhood reported at least one other type of adverse childhood experience, and 50% reported two or more types ( 2 ). Moreover, increased exposure to adverse childhood experiences is related to a greater likelihood of developing a variety of behavioral, health, and mental health problems, including smoking, multiple sexual partners, heart disease, cancer, lung disease, liver disease, sexually transmitted diseases, substance abuse, depression, and suicide attempts ( 4 , 5 , 6 , 7 , 8 ).
Aside from findings of the Adverse Childhood Experiences study, there is abundant evidence that adults with mood disorders have often experienced adverse childhood experiences, including childhood sexual and physical abuse, neglect, witnessing domestic violence, early parental loss, parental divorce, parental mental illness, and out-of-home placement ( 1 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ). However, fewer studies have examined the long-term health and mental health implications of adverse childhood experiences among persons with severe mood disorders. The few available studies suggest that exposure to adverse childhood experiences is associated with worse subsequent functioning among those with major depression or bipolar disorder. For example, individuals with mood disorders who were exposed to parental mental illness in childhood tend to have an earlier onset of depression, more depressive episodes, more severe and persistent symptoms, and greater impairment ( 18 ). In addition to having a genetically transmitted familial risk ( 19 , 20 ), persons with mood disorders exposed to parental mental illness may experience heightened stress and negative or disengaged parenting behavior in their developmental years ( 21 ). Exposure to child abuse among individuals who develop mood disorders is associated with an increased likelihood of self-injurious behavior ( 21 , 22 ), impulsivity ( 22 ), and higher severity and number of suicide attempts ( 22 , 23 ). Moreover, among adults with bipolar disorder severe physical, sexual, and emotional abuse in childhood has been linked to earlier onset of the disorder, rapid cycling, and more frequent suicide attempts ( 24 , 25 ).
Thus research indicates that exposure to adverse experiences in childhood is related to more severe symptoms and a worse course of illness among individuals with mood disorders. However, previous research has focused mainly on the relationship between specific adverse childhood experiences and course of illness among those with major mood disorders. Fewer studies have examined the correlates of exposure to the broad range of adverse childhood experiences and mental health functioning in mood disorders or between adverse childhood experiences and long-term health and functioning in this population. A study of mental health functioning among 569 adults with schizophrenia suggested that increased exposure to adverse childhood experiences is strongly related to psychiatric problems (suicidal thinking, hospitalizations, distress, and posttraumatic stress disorder [PTSD]), substance abuse, physical health problems (HIV infection), medical service utilization (physician visits), and poor social functioning (homelessness or criminal justice involvement) ( 26 ). This suggests the need to examine the correlates of exposure to the broad range of adverse childhood experiences and mental health functioning as well as long-term health and functioning in mood disorders.
In the study reported here, we examined the relationship between cumulative exposure to adverse childhood experiences in a large, multisite sample of public-sector mental health clients diagnosed as having major mood disorders. We hypothesized that greater exposure to adverse childhood experiences would be related to worse functioning across several domains of functioning, including psychiatric problems, substance use disorders, physical health problems, trauma exposure in adulthood, high-risk behavior, and community adjustment.
Methods
Participants
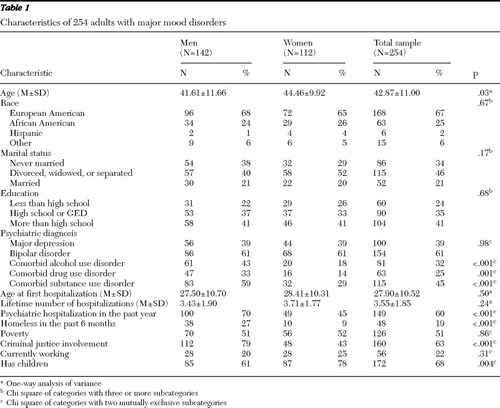
The participants were 274 adults with severe mood disorders (major depression or bipolar disorder) drawn from a larger investigation of risky behavior and sexually transmitted diseases among persons with severe mental illness ( 27 ). All participants were receiving treatment through the public mental health systems of Connecticut, Maryland, New Hampshire, or North Carolina or through the Durham, North Carolina, Department of Veterans Affairs (VA) Medical Center. Most were receiving some form of disability income as a result of their psychiatric disorder. The mental health centers were located in rural, urban, and metropolitan areas. Specifically, 8% of the participants were located in urban and metropolitan areas, 20% were receiving services from a VA medical center, and 43% were recipients of inpatient services. Among the 274 persons with mood disorders, 254 had complete data on adverse childhood experiences and were included in the analyses. Characteristics of the sample are presented in Table 1 .
 |
Measures
This study assessed adverse childhood experiences, psychiatric problems, substance use disorders, physical health, and community functioning through chart review, structured interviews, and self-report instruments.
Psychiatric diagnoses. Psychiatric diagnoses were based on chart records for 222 participants (81%) and on the Structured Clinical Interview for DSM-IV (SCID) ( 28 ) for 52 participants (19%). Four of the sites assessed the validity of the chart diagnoses by administering the SCID and found high concordance rates ( κ =.72). This supports the validity of chart diagnoses for the study participants.
Adverse childhood experiences. Standardized, self-report measures administered in an interview format were used to assess childhood abuse, household dysfunction, and losses that occurred during the first 16 years of participants' lives. Childhood sexual abuse was assessed with the Sexual Abuse Exposure Questionnaire ( 29 ). This scale identifies ten categories of increasingly invasive sexual experiences via self-report and has good test-retest reliability among clients with severe mental illness ( 30 ). Participants were considered to have experienced childhood sexual abuse if they responded affirmatively to any of the six items involving physical sexual contact.
Childhood physical abuse was assessed by the three most severe items from the violence subscale of the Conflict Tactics Scales ( 31 ). An affirmative response on any of the three questions (being hit, being knocked down or thrown, and being burned or scalded on purpose) was used to indicate a history of physical abuse.
Parental separation or divorce was defined by an affirmative response to the question, "When you were growing up, did your parents/caretakers get a divorce or separation?" Domestic violence was assessed by the question, "When you were growing up, did you see or hear your parents/caretakers arguing or fighting a lot?" Foster/kinship care was assessed by two questions that asked whether the respondent was placed in an orphanage, foster home, boys' home, reformatory, detention, jail, or similar placement or sent to live with relatives, family friends, or other people. Parental mental illness was derived by an affirmative response to the question, "When you were growing up, did your parent(s)/caretaker(s) ever see a counselor, psychologist, or psychiatrist, or go to a mental hospital, or take medication for an emotional problem?" Parental death was based on client self-report of whether the client's father or mother died before the client turned 16.
Psychiatric problems. Suicidal ideation, self-injurious behavior, and recent suicide attempts were assessed by asking participants if they felt so low that they thought of suicide, if they tried to hurt themselves, and if they attempted suicide in the past six months. Hospitalization history was measured via self-report by age at first hospitalization, the total number of psychiatric hospitalizations, and the number of hospitalizations in the previous year.
PTSD was assessed with the PTSD Checklist (PCL) ( 32 ), a self-report measure. The PCL includes 17 questions, one for each DSM-IV PTSD symptom; it requires the respondent to rate the severity of each symptom over the past month on a 5-point Likert scale. A PTSD diagnosis is made if at least one criterion B (intrusive) symptom, three criterion C (avoidant) symptoms, and two criterion D (hyperarousal) symptoms are rated at 3 or above on the Likert scale or if the total PCL score is 45 or more. The PCL has strong test-retest reliability and convergent validity among persons with severe mental illness ( 33 ).
Substance use disorders. Current alcohol and drug use disorders were identified with the Dartmouth Assessment of Lifestyle Instrument (DALI) ( 34 ). The DALI is an 18-item screening tool for substance use disorders (abuse or dependence) that was specifically developed and validated for persons with severe mental illness. It has high classification accuracy for DSM-IV current substance use disorders involving alcohol, cannabis, or cocaine. Cutoff scores have been developed by use of an empirically derived algorithm. Clients were categorized as having a substance use disorder if the DALI was positive.
Physical health. Physical health was assessed with items from the Piedmont Health Survey ( 35 ), which includes questions on chronic medical problems, including asthma, diabetes, heart trouble, hypertension, arthritis, cancer, lung diseases, ulcers, stroke, epilepsy, head injury, or infectious diseases (for example, sexually transmitted diseases and hepatitis). For this study the number of problems endorsed was summed to form an overall measure of health problems. Participants were also asked to report the number of times in the past six months that they had received care for a physical health problem and the number of days hospitalized for physical health problems.
HIV, hepatitis B, and hepatitis C were assessed through laboratory analyses of blood specimens obtained through venipuncture or finger stick. Serologic tests for HIV antibodies in serum utilized the Genetic Systems HIV-1/HIV-2 enzyme-linked immunosorbent assay (ELISA), and results were confirmed by an HIV-Western blot (BioRad). Antibodies to hepatitis B core were assessed with the Abbott Corzyme test. Antibodies to hepatitis C were assessed in serum via the Abbott HCV-2 ELISA and confirmed by a recombinant immunoblot (Ortho). All serologic testing and procedures were licensed by the U.S. Food and Drug Administration and were performed in laboratories accredited by the College of American Pathologists. Details of the procedures have been described by Rosenberg and colleagues ( 36 ).
Community functioning. Information about homelessness was obtained via self-report. Homelessness was defined as having no regular residence or living in a shelter or on the street for at least one day during the past six months.
Poverty status was assessed via self-report and was based on past-year income. The 1999 guidelines of the U.S. Department of Health and Human Services were used to define poverty status; the guidelines take into account income, marital status, and number of children.
Criminal justice involvement was assessed via self-report and defined as ever having been arrested for any offense.
Work functioning was assessed via self-report and defined as whether the client was currently working or had worked in the past year.
Trauma exposure in adulthood. Exposure to physical assault or sexual assault since age 17 and in the past year was measured by the physical assault and sexual assault subscales of the Revised Conflict Tactics Scales ( 37 ). Physical assault was defined as any assault, ranging from grabbing, pushing, or shoving to using a knife or gun, that was perpetrated against the participant. Sexual assault was defined as oral, anal, or vaginal intercourse achieved through either physical force or threat.
High-risk behaviors. High-risk behaviors were those associated with increased risk of diseases transmitted via blood, such as HIV, hepatitis B, and hepatitis C (for example, unprotected sex and sharing needles for injection drug use). The AIDS Risk Inventory ( 38 , 39 ), a structured interview for assessing risk behaviors associated with acquiring and transmitting these infections, was used. The instrument was modified for this study so that it would be easily understood by respondents with severe mental illnesses. The selected risk variables include lifetime trading of sex for drugs, gifts, or money; lifetime injection of a drug; lifetime administration of a drug by sniffing; lifetime needle sharing; lifetime sex between men; and two or more sexual partners in the past six months.
Procedure
After clients gave informed consent, they participated in structured interviews that lasted from 60 to 90 minutes, received pretest counseling for HIV-AIDS, and provided blood specimens as part of a screening for HIV and other sexually transmitted diseases. All clients were paid for participation in the assessments and were provided with test results, posttest counseling, and referrals for follow-up testing and treatment as needed.
Statistical analyses
Prevalence rates of adverse childhood experiences and the association between different types of adverse childhood experiences were computed first. The association between cumulative number of adverse childhood experiences and outcomes was then examined by use of logistic regression analyses that controlled for demographic characteristics (gender, age, race, and education level).
Results
Prevalence and interrelationships
The prevalence of adverse childhood experiences in the sample is summarized in Table 2 , along with the prevalence in large community samples ( 1 , 3 , 40 , 41 ). In this sample of 254 adults with mood disorders, the most common types of adverse childhood experience were physical abuse and exposure to domestic violence. Women experienced a greater number of adverse childhood experiences than men, and Caucasians experienced more adverse childhood experiences than African Americans. Only 11% of participants reported that they had experienced no adverse childhood experiences; 17% reported one event, and 50% reported three or more events. In comparison, studies of adverse childhood experiences in community samples have found lower rates; about one-fifth of respondents in the Adverse Childhood Experiences study reported three or more adverse events ( 3 ), and only one-third of respondents in the National Comorbidity Study reported three or more events ( 1 ). No site effect was found (urban versus rural site, VA medical center versus community mental health center, or inpatient versus outpatient setting). These findings suggest that adults with severe mood disorders have had greater exposure to adverse childhood experiences than the general population.
 |
Table 3 summarizes the co-occurrence of different adverse childhood experiences. Most clients who had experienced one adverse event had also experienced between two and three other events. For example, among those who had a parent with a mental illness, more than half also had experienced parental divorce, foster care, and physical and sexual abuse; among those who had experienced sexual abuse, more than half had also experienced physical abuse, witnessed domestic violence, and been placed in foster care. Parental mental illness was associated with the highest number of co-occurring adverse childhood experiences, with an average of three other events.
 |
Association between adverse experiences and adult functioning
The results of the logistic regression analyses evaluating associations between cumulative exposure to adverse childhood experiences and functioning are summarized in Table 4 . In this study all the functional, mental health, and physical health variables were coded as dichotomous dependent variables. The independent variables included the number of adverse childhood experiences, age, gender, educational attainment, and race. Each experience variable was dichotomized (score of 0 or 1, absent or present). The total score of the number of adverse childhood experiences served as an overall adversity index and was entered into the multiple logistic regression analysis. Age and educational attainment were measured in terms of years. Gender and race (coded as white versus other) were dichotomous. Multiple logistic regression analysis was used to adjust for the potential confounding effects of age, gender, race, and educational attainment on the relationship between the number of adverse childhood experiences and functional, health, and mental health outcomes. If the odds ratio is greater than 1.0, it suggests that the odds of the outcome increase when the number of the adverse childhood experiences is increased by 1. If the odds ratio is less than 1.0, it suggests that the odds of the outcome decrease when the number of experiences increases.
 |
As shown in Table 4 , the odds of being hospitalized before the age of 17 and having a current substance use disorder, recent suicidal behavior, and a diagnosis of PTSD were increased when the number of adverse childhood experiences increased. Meanwhile, adverse childhood experiences were also significantly related to some of the measures of health functioning, including number of visits to the doctor and number of health problems. With respect to community functioning, adverse childhood experiences were related to homelessness and also to criminal behavior, but less strongly. Adverse childhood experiences were not related to work or poverty. Finally, adverse childhood experiences were strongly related to increased physical or sexual victimization in the past year and since age 17; they were also related to most high-risk behaviors, including risky sexual practices and drug behaviors.
Discussion
Compared with findings from national surveys of the U.S. general population ( 1 , 3 ), the results of this study indicate that adults with severe mood disorders were more likely to have experienced a range of adverse childhood experiences. The most common adverse childhood experiences in this population were witnessing domestic violence and being physically abused, followed by being sexually abused, being placed in foster or kinship care, and experiencing parental separation or divorce, parental mental illness, and parental death. A majority of clients who were exposed to one type of adverse childhood experience were also exposed to two or three others. This pattern of high co-occurrence between different adverse childhood experiences is consistent with results found in the general population ( 3 ).
Previous research has shown that exposure to any one of the various types of adverse childhood experience, such as parental mental illness or child abuse, is related to worse outcomes in mood disorders ( 1 , 18 , 42 , 43 ). The study reported here goes beyond previous research this area by documenting relationships between cumulative exposure to adverse childhood experiences and different functional outcomes among adults with mood disorders. Specifically, cumulative exposure to adverse childhood experiences was related to younger age at first hospitalization and number of recent suicide attempts; revictimization in adulthood and a diagnosis of PTSD; health risk behaviors, such as having multiple sexual partners and sharing needles for injection drug use; diagnosis of a substance use disorder; self-reported health problems and medical service utilization; and homelessness. There was a significant association between adverse childhood experiences and suicide attempts. Similar findings have been reported for the general population ( 4 ) and from other studies of mood disorders ( 24 , 25 ). Furthermore, the association between adverse childhood experiences and younger age at first hospitalization is in line with findings from studies on bipolar disorders ( 26 ) and depression ( 18 ) and suggests that experiencing adverse events in childhood not only increases the risk of developing a mood disorder but also portends a more severe disorder.
Increased exposure to adverse childhood experiences was related to a higher likelihood of physical and sexual assault in adulthood, both in the adult lifetime and in the past year. This finding is consistent with research showing that early victimization increases the chances of subsequent revictimization both in the general population ( 43 , 44 , 45 , 46 , 47 , 48 , 49 ) and among people with severe mental illnesses, such as schizophrenia ( 30 , 50 , 51 ). In addition, the association between exposure to adverse childhood experiences and PTSD diagnosis, which is likely strengthened by subsequent revictimization, is consistent with findings from studies of adolescents ( 52 , 53 ) and research on the correlates of childhood sexual abuse ( 29 , 54 , 55 ).
Consistent with findings from the general population ( 6 , 56 ) and among people with schizophrenia or schizoaffective disorder ( 22 ), our results indicate that adverse childhood experiences had a significant association with development of a drug use disorder and an overall significant relationship with development of a substance use disorder. In addition, exposure to adverse childhood experiences was also associated with high-risk behaviors, such as injection drug use and trading sex for drugs or money. Similar findings in the general adult population indicate a link between child abuse and subsequent high-risk behaviors. For example, research has documented the relationship between childhood sexual abuse and adulthood high-risk behaviors, such as promiscuity, unprotected sex, exchange of sex for money or other necessities (such as drugs), and injection drug use ( 44 , 57 , 58 , 59 ).
The findings of this study have three important implications. They suggest that most clients with mood disorders in the public mental health system are likely to have been exposed to serious adverse experiences in childhood; that the social and psychological consequences of these early experiences include increased trauma exposure in adulthood and PTSD, high-risk behavior, and worse health, mental health, and functional outcomes; and that treatment for people with mood disorders should recognize the complex set of treatment needs—over and above the need for effective treatment of depression or bipolar disorder—that it is necessary to address in order to reduce morbidity and mortality among these clients. Mental health providers will be challenged to develop and test integrated models of care that address the most common and serious conditions that are comorbid with mood disorders, including exposure to trauma, high-risk behavior, and substance use disorders.
The study has several limitations. This was a retrospective study, and thus underreporting or overreporting of adverse childhood experiences may have occurred. However, longitudinal follow-up studies of adults with documented childhood abuse have shown that retrospective reports of childhood abuse are more likely to underestimate actual occurrence ( 60 , 61 ). Second, although a large, multisite sample was used, it was nevertheless a convenience clinical sample of clients with severe mood disorders and may not be representative of all clients with mood disorders or all clients of the U.S. public mental health system. For example, the sample underrepresents the Hispanic population in these settings. Finally, the measures used in this study were self-report measures and also were not identical to those used in the National Comorbidity Survey and the Adverse Childhood Experiences study, which prevents precise comparisons between findings.
Conclusions
This study provides evidence that routine clinical assessment of self-reported adverse childhood experiences is warranted in the care of persons with mood disorders. Multiple forms of chronic childhood stress may place the developing child in a vulnerable position biologically ( 2 , 3 ) and mentally. The clinical implications of this study include the following: in the care of people with severe mood disorders, it is important to ask questions routinely during intakes in order to elicit information about possible adverse childhood experiences. If these experiences are confirmed, it is important to assess the degree to which the client exhibits risk behaviors or posttraumatic symptoms that might be addressed clinically (for example, PTSD symptoms that might be addressed through evidence-based cognitive-behavioral therapy). Particular treatment approaches for people with mood disorders include integrated care for trauma and drug use along with management of high-risk behaviors. Frontline clinicians often do not have adequate training in interventions to address consequences in adulthood that are related to exposure to adverse childhood experiences among clients with mood disorders. Training in the areas of the prevention of retraumatization, treatment of PTSD, management of high-risk sexual and drug use behaviors, and suicidal attempts may help improve outcomes. Ultimately, the findings suggest that prevention of adverse childhood experiences is important for adult mental health.
Acknowledgments and disclosures
This research was supported by grants R01-MH-50094-03S2, P50-MH-43703, R01-MH-48103-05, P50-MH-51410-02, R24-MH-54446-05, and R01-MH-52872 from the National Institute of Mental Health, by grant UNC-CHJ from the Duke Program on Services Research for People With Severe Mental Disorders, by grant CT-DMH from Yale, and by grant EPP97-022 from the Veterans Affairs Epidemiologic Research Information Center. The authors acknowledge the contributions of the members of the five-site Health and Risk Study Research Committee: Susan M. Essock, Ph.D., and Jerilynn Lamb-Pagone, M.S.N., in Connecticut; Marvin Swartz, M.D., Jeffrey Swanson, Ph.D., and Barbara J. Burns, Ph.D., at Duke University, Durham, North Carolina; the late Marian I. Butterfield, M.D., Keith G. Meador, M.D., M.P.H., Hayden B. Bosworth, Ph.D., Mary E. Becker, Richard Frothingham, M.D., Ronnie D. Homer, Ph.D., Lauren M. McIntyre, Ph.D., Patricia M. Spivey, and Karen M. Stechuchak, M.S., in Durham, North Carolina; Fred C. Osher, M.D., Lisa A. Goodman, Ph.D., Lisa J. Miller, Jean S. Gearon, Ph.D., Richard W. Goldberg, Ph.D., John D. Herron, L.C.S.W., Raymond S. Hoffman, M.D., and Corina L. Riismandel in Maryland; and Patricia C. Auciello, M.S., George Wolford, Ph.D., Mark C. Iber, Ravindra Luckoor, M.D., Gemma R. Skillman, Ph.D., Rosemarie S. Wolfe, M.S., Robert M. Vidaver, M.D., and Michelle P. Salyers, Ph.D., in New Hampshire.
The authors report no competing interests.
1. Kessler RC, Davis CG, Kendler KS: Childhood adversity and adult psychiatric disorder in the United States National Comorbidity Survey. Psychological Medicine 27: 1101–1119, 1997Google Scholar
2. Anda RF, Croft JB, Felitti VJ, et al: Adverse childhood experiences and smoking during adolescence and adulthood. JAMA 282: 1652–1658, 1999Google Scholar
3. Felitti VJ, Anda RF, Nordenberg D, et al: Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine 14:245–258, 1998Google Scholar
4. Dube SR, Anda RF, Felitti VJ, et al: Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences study. JAMA 286: 3089–3096, 2001Google Scholar
5. Dube SR, Anda RF, Felitti VJ, et al: Adverse childhood experiences and personal alcohol abuse as an adult. Addictive Behaviors 27:713–725, 2002Google Scholar
6. Dube SR, Felitti VJ, Dong M, et al: Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the Adverse Childhood Experiences study. Pediatrics 111:564–572, 2003Google Scholar
7. Chapman DP, Whitfield CL, Felitti VJ, et al: Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders 82:217–225, 2004Google Scholar
8. Anda RF, Felitti VJ, Bremner JD, et al: The enduring effects of abuse and related adverse experiences in childhood: a convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience 256:174–186,2006Google Scholar
9. Brown GW, Moran P: Clinical and psychosocial origins of chronic depressive episodes: I. a community survey. British Journal of Psychiatry 165:447–456, 1994Google Scholar
10. Zlotnick C, Ryan CE, Miller IW, et al: Childhood abuse and recovery from major depression. Child Abuse and Neglect 19: 1513–1516, 1995Google Scholar
11. Mueser KT, Goodman LA, Trumbetta SL, et al: Trauma and posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology 66: 493–499, 1998Google Scholar
12. Goodman LA, Salyers MP, Mueser KT, et al: Recent victimization in women and men with severe mental illness: prevalence and correlates. Journal of Traumatic Stress 14: 615–632, 2001Google Scholar
13. Read J, Perry BD, Moskowitz A, et al: The contribution of early traumatic events to schizophrenia in some patients: a traumagenic neurodevelopmental model. Psychiatry 64:319–345, 2001Google Scholar
14. Gilman SE, Kawachi I, Fitzmaurice GM, et al: Socioeconomic status, family disruption, and residential stability in childhood: relation to the onset, recurrence, and remission of major depression. Psychological Medicine 33:1341–1355, 2003Google Scholar
15. Gilman SE, Kawachi I, Fitzmaurice GM, et al: Family disruption in childhood and risk of adult depression. American Journal of Psychiatry 160:939–946, 2003Google Scholar
16. Kendler KS, Kuhn JW, Prescott CA: Childhood sexual abuse, stressful life events and risk for major depression in woman. Psychological Medicine 34:1475–1482, 2004Google Scholar
17. Turner RJ, Lloyd DA: Stress burden and the lifetime incidence of psychiatric disorder in young adults: racial/ethnic contrasts. Archives of General Psychiatry 61:481–488, 2004Google Scholar
18. Lieb R, Isensee B, Höfler M, et al: Parental major depression and the risk of depression and other mental disorders in offspring: a prospective-longitudinal community study. Archives of General Psychiatry 59:365–374, 2002Google Scholar
19. Potash JB, Toolan J, Steele J, et al: The Bipolar Disorder Phenome Database: a resource for genetic studies. American Journal of Psychiatry 164:1229–1237, 2007Google Scholar
20. Goes FS, Zandi PP, Miao K, et al: Mood-incongruent psychotic features in bipolar disorder: familial aggregation and suggestive linkage to 2p11-q14 and 13q21-33. American Journal of Psychiatry 164:236–247, 2007Google Scholar
21. Newport DJ, Stowe ZN, Nemeroff CB: Parental depression: animal models of an adverse life event. American Journal of Psychiatry 159:1265–1283, 2002Google Scholar
22. Rosenberg SD, Lu W, Mueser KT, et al: Correlates of adverse childhood events among adults with schizophrenia spectrum disorders. Psychiatric Services 58:245–253, 2007Google Scholar
23. Gladstone G, Parker G, Wilhelm K, et al: Characteristics of depressed patients who report childhood sexual abuse. American Journal of Psychiatry 156:431–437, 1999Google Scholar
24. Brodsky BS, Oquendo M, Ellis SP, et al: The relationship of childhood abuse to impulsivity and suicidal behavior in adults with major depression. American Journal of Psychiatry 158:1871–1877, 2001Google Scholar
25. Swann AC, Dougherty DM, Pazzaglia PJ, et al: Increased impulsivity associated with severity of suicide attempt history in patients with bipolar disorder. American Journal of Psychiatry 162:1680–1687, 2005Google Scholar
26. Garno JL, Goldberg JF, Ramirez PM, et al: Impact of childhood abuse on the clinical course of bipolar disorder. British Journal of Psychiatry 186:121–125, 2005Google Scholar
27. Rosenberg SD, Trumbetta SL, Mueser KT, et al: Determinants of risk behavior for HIV/AIDS in people with severe and persistent mental illness. Comprehensive Psychiatry 42:263–271, 2001Google Scholar
28. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for DSM-IV Axis-I Disorders-Patient Edition (SCID-I/P Version 2.0). New York, New York State Psychiatric Institute, Biometrics Research Department, 1996Google Scholar
29. Rodriguez N, Ryan SW, Van De Kemp H, et al: Posttraumatic stress disorder in adult female survivors of childhood sexual abuse: a comparison study. Journal of Consulting and Clinical Psychology 65:53–59, 1997Google Scholar
30. Goodman LA, Rosenberg SD, Mueser KT, et al: Physical and sexual assault history in women with serious mental illness: prevalence, correlates, treatment and future research. Schizophrenia Bulletin 23:685–696, 1997Google Scholar
31. Straus M, Gelles R: Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8145 families. New Brunswick, NJ, Transaction Books, 1989Google Scholar
32. Blanchard EP, Jones-Alexander J, Buckley TC, et al: Psychometric properties of the PTSD Checklist. Behavior Therapy 34: 669–673, 1996Google Scholar
33. Mueser KT, Salyers MP, Rosenberg SD, et al: A psychometric evaluation of trauma and PTSD assessments in persons with severe mental illness. Psychological Assessment 13:110–117, 2001Google Scholar
34. Rosenberg SD, Drake RE, Wolford GL, et al: The Dartmouth Assessment of Lifestyle Instrument (DALI): a substance use disorder screen for people with severe mental illness. American Journal of Psychiatry 155: 232–238, 1998Google Scholar
35. Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. JAMA 264:2511–2518, 1990Google Scholar
36. Rosenberg SD, Goodman LA, Osher FC, et al: Prevalence of HIV, hepatitis B, and hepatitis C in people with severe mental illness. American Journal of Public Health 91:31–37, 2001Google Scholar
37. Straus MA, Hamby SL, Boney-McCoy S, et al: The revised conflict tactics scales (CTS2): development and preliminary psychometric data. Journal of Family Issues 17:283–316, 1996Google Scholar
38. Chawarski MC, Pakes J, Schottenfeld RS: Assessment of HIV risk. Journal of Addictive Diseases 17:49–59, 1998Google Scholar
39. Chawarski MC, Baird JC: Comparison of two instruments for assessing HIV risk in drug abusers, in Social and Behavioral Science: Proceedings of the 12th World AIDS Conference. Bologna, Italy, Monduzzu Editore, 1998Google Scholar
40. Ehrle J, Green R, Clark R: Children Reared by Relatives: How Are They Faring? Washington, DC, Urban Institute, 2001Google Scholar
41. Ehrle J, Green R: Kin and non-kin foster care: findings from a national survey. Children and Youth Services Review 24:15–35, 2002Google Scholar
42. Levitan RD, Rector NA, Sheldon T, et al: Childhood adversities associated with major depression and/or anxiety disorders in a community sample of Ontario: issues of co-morbidity and specificity. Depression and Anxiety 17:34–42, 2003Google Scholar
43. Kessler RC, Magee WJ: Childhood family violence and adult recurrent depression. Journal of Health and Social Behavior 35:13–27, 1994Google Scholar
44. Steele JL, Herlitz CA: The association between childhood and adolescent sexual abuse and proxies for sexual risk behavior: a random sample of the general population of Sweden. Child Abuse and Neglect 29: 1141–1153, 2005Google Scholar
45. Fleming J, Mullen PE, Sibthorpe B, et al: The long-term impact of childhood sexual abuse in Australian women. Child Abuse and Neglect 23:145–159, 1999Google Scholar
46. Merrill L, Newell CE, Thomsen CJ, et al: Childhood abuse and sexual revictimization in a female Navy recruit sample. Journal of Traumatic Stress 12:211–225, 1999Google Scholar
47. Messman TL, Long PJ: Child sexual abuse and its relationship to revictimization in adult women: a review. Clinical Psychology Review 16:397–420, 1996Google Scholar
48. Sanders B, Moore DL: Childhood maltreatment and date rape. Journal of Interpersonal Violence 14:115–124, 1999Google Scholar
49. Urquiza AJ, Goodlin-Jones BL: Child sexual abuse and adult revictimization with women of color. Violence and Victims 9: 223–232, 1994Google Scholar
50. Goodman LA, Fallot RD: HIV risk-behavior in poor urban women with serious mental disorders: association with childhood physical and sexual abuse. American Journal of Orthopsychiatry 68:73–83, 1998Google Scholar
51. Cloitre M, Tardiff K, Marzuk PM, et al: Childhood abuse and subsequent sexual assault among female inpatients. Journal of Traumatic Stress 9:473–482, 1996Google Scholar
52. Hussey DL, Singer M: Psychological distress, problem behaviors, and family functioning of sexually abused adolescent inpatients. Journal of the American Academy of Child and Adolescent Psychiatry 32:954–961, 1993Google Scholar
53. McLeer S, Callaghan M, Henry D, et al: Psychiatric disorders in sexually abused children. Journal of the American Academy of Child and Adolescent Psychiatry 33:313–319, 1994Google Scholar
54. Browne A, Finkelhor D: Impact of child sexual abuse: a review of the research. Psychological Bulletin 99:66–77, 1986Google Scholar
55. Fergusson DM, Horwood LJ, Lynskey MT: Childhood sexual abuse and psychiatric disorder in young adulthood: II. psychiatric outcomes of childhood sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry 35:1365–1374, 1996Google Scholar
56. Dube SR, Anda RF, Felitti VJ, et al: Exposure to abuse, neglect, and household dysfunction among adults who witnessed intimate partner violence as children: implications for health and social services. Violence and Victims 17:3–17, 2002Google Scholar
57. Bensley LS, Van Eenwyk J, Simmons KW: Self-reported childhood sexual and physical abuse and adult HIV-risk behaviors and heavy drinking. American Journal of Preventive Medicine 18:151–158, 2000Google Scholar
58. Hillis SD, Anda RF, Felitti VJ, et al: Adverse childhood experiences and sexually transmitted diseases in men and women: a retrospective study. Pediatrics 106(1):e11, 2000Google Scholar
59. Zierler S, Feingold L, Laufer D, et al: Adult survivors of childhood sexual abuse and subsequent risk of HIV infection. American Journal of Public Health 81:572–575, 1991Google Scholar
60. Widom C, Shepard R: Accuracy of adult recollections of childhood victimization: Part 1. Psychological Assessment 8:412–421, 1996Google Scholar
61. Widom C, Shepard R: Accuracy of adult recollections of childhood victimization: part 2. childhood sexual abuse. Psychological Assessment 9:34–46, 1997Google Scholar



